Podcast
Questions and Answers
What is the primary significance of presenting symptoms in extracranial carotid disease?
What is the primary significance of presenting symptoms in extracranial carotid disease?
- It is a major factor in determining treatment and prognosis (correct)
- It is a minor factor in determining treatment and prognosis
- It determines the prognosis of a stroke
- It has no impact on treatment and prognosis
What is the primary difference between a stroke and a transient ischemic attack (TIA)?
What is the primary difference between a stroke and a transient ischemic attack (TIA)?
- The severity of neurological symptoms
- The presence of complete resolution of the deficit
- The age of the patient
- The duration of neurological symptoms (correct)
What is the characteristic of a crescendo TIA?
What is the characteristic of a crescendo TIA?
- Infrequent isolated neurological attacks with complete resolution
- Frequent repetitive neurological attacks with complete resolution of the deficit between episodes (correct)
- Frequent repetitive neurological attacks with progressive deterioration
- Single severe neurological attack with permanent deficit
What is the primary distinction between a crescendo TIA and a stroke in evolution?
What is the primary distinction between a crescendo TIA and a stroke in evolution?
What is the significance of a crescendo TIA or a stroke in evolution?
What is the significance of a crescendo TIA or a stroke in evolution?
What scale is used to grade the severity of strokes?
What scale is used to grade the severity of strokes?
What is the characteristic of an intramural hematoma?
What is the characteristic of an intramural hematoma?
What is the primary cause of death in type A aortic dissections?
What is the primary cause of death in type A aortic dissections?
What is the classification system proposed by Dr. Lombardi?
What is the classification system proposed by Dr. Lombardi?
What is the zone classification of the aorta in the new system published in 2020?
What is the zone classification of the aorta in the new system published in 2020?
What is the mortality rate of untreated type A dissections?
What is the mortality rate of untreated type A dissections?
What is the incidence of acute aortic dissections?
What is the incidence of acute aortic dissections?
What is the primary symptom of a patient with a blunt thoracic aortic injury?
What is the primary symptom of a patient with a blunt thoracic aortic injury?
What is the significance of multiple false lumens in aortic dissections?
What is the significance of multiple false lumens in aortic dissections?
What is the significance of a penetrating aortic ulcer?
What is the significance of a penetrating aortic ulcer?
What is the classification of type B aortic dissections?
What is the classification of type B aortic dissections?
Which artery commonly branches off the false lumen in an aortic dissection?
Which artery commonly branches off the false lumen in an aortic dissection?
What is the danger of a false lumen in an aortic dissection?
What is the danger of a false lumen in an aortic dissection?
What is the clinical significance of a penetrating aortic ulcer with intramural hematoma?
What is the clinical significance of a penetrating aortic ulcer with intramural hematoma?
What is the primary complication of a false lumen with a diameter of more than 22mm?
What is the primary complication of a false lumen with a diameter of more than 22mm?
What is the primary significance of aortic dissection extending into the left common iliac artery?
What is the primary significance of aortic dissection extending into the left common iliac artery?
What is the primary risk factor for early complication or continued growth of an aortic dissection?
What is the primary risk factor for early complication or continued growth of an aortic dissection?
Flashcards are hidden until you start studying
Study Notes
Transient Ischemic Attack (TIA) and Stroke
- A TIA is a focal neurologic symptom that occurs suddenly and resolves within 24 hours.
- If the deficit persists beyond 24 hours, it is considered a stroke.
- Strokes are graded according to the National Institute of Health Stroke Scale (NIHSS).
Crescendo TIA vs Stroke in Evolution
- A crescendo TIA refers to frequent, repetitive neurological attacks with complete resolution of the deficit between episodes, usually within a 24-hour period, resulting in the same neurological deficit.
- A stroke in evolution is characterized by progressive deterioration in neurological function between TIA episodes.
- Crescendo TIA and stroke in evolution are both concerning findings that may indicate a need for emergent intervention.
Aortic Dissection
- Chest pain that extends to the abdomen may be a sign of mesenteric ischemia or aortic tear.
- Chest pain is a common symptom, occurring in 90% of patients, with tearing pain radiating between the shoulder blades.
Risk Factors and Causes
- Presence of multiple false lumens is associated with increased risk of aortic dissection-related death.
- Blunt thoracic aortic injury can also cause aortic dissections.
- Patients with penetrating aortic ulcers and intramural hematomas are at high risk of aortic rupture.
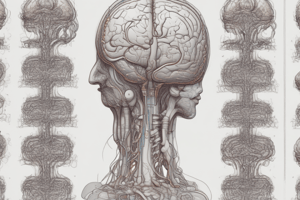
Anatomy and Pathophysiology
- The dissection most commonly extends down to the left common iliac artery rather than the right.
- The celiac trunk, SMA, and right renal artery typically arise from the true lumen, while the left renal artery arises from the false lumen.
- A false lumen can lead to end-organ ischemia by covering the ostia of branching vessels.
- The false lumen can also lead to weakening of the aortic wall, potentially causing rupture if the diameter is larger than 22mm.
Classification and Diagnosis
- Aortic dissections can be classified into two main types: Type A (ascending aorta) and Type B (descending aorta).
- The SVS-STS classification system divides the aorta into zones from 0 (proximally) to 12 (distally in the mid-SFA).
- CT angiography can detect intramural hematomas, penetrating aortic ulcers, and other signs of aortic dissection.
Complications and Prognosis
- High-risk features for early complication or continued growth include a false lumen diameter greater than 22mm.
- Early mortality for untreated Type A dissections is 1-2% per hour, with 20% mortality within 6 hours, 50% within 24 hours, and 70% within the first week.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.