Podcast
Questions and Answers
What is the approximate percentage of Transient Ischemic Attacks (TIAs) that last greater than 1 hour?
What is the approximate percentage of Transient Ischemic Attacks (TIAs) that last greater than 1 hour?
- 5%
- 25% (correct)
- 50%
- 10%
What is the percentage of strokes that are hemorrhagic?
What is the percentage of strokes that are hemorrhagic?
- 20%
- 15% (correct)
- 5%
- 10%
What is the time frame within which half of the strokes occur after a Transient Ischemic Attack (TIA)?
What is the time frame within which half of the strokes occur after a Transient Ischemic Attack (TIA)?
- 24 hours
- 1 week
- 48 hours (correct)
- 3 months
What is the site of Extracranial atherosclerosis?
What is the site of Extracranial atherosclerosis?
What is the reported prevalence of prior TIA among those who present with a stroke?
What is the reported prevalence of prior TIA among those who present with a stroke?
What is the time frame within which someone dies of a stroke in the United States?
What is the time frame within which someone dies of a stroke in the United States?
What is the definition of a Transient Ischemic Attack (TIA) based on tissue?
What is the definition of a Transient Ischemic Attack (TIA) based on tissue?
What percentage of TIAs will be followed by a stroke within 3 months?
What percentage of TIAs will be followed by a stroke within 3 months?
What percentage of individuals have a symmetrical Circle of Willis?
What percentage of individuals have a symmetrical Circle of Willis?
What is the primary mechanism responsible for episodes of TIA/STROKE in carotid artery disease?
What is the primary mechanism responsible for episodes of TIA/STROKE in carotid artery disease?
What is the recommended treatment for hypertension in carotid artery disease management?
What is the recommended treatment for hypertension in carotid artery disease management?
What is the goal of carotid interventions in carotid artery disease management?
What is the goal of carotid interventions in carotid artery disease management?
What is the recommended technique for carotid endarterectomy closure?
What is the recommended technique for carotid endarterectomy closure?
What is the purpose of embolic protection filters in carotid stenting?
What is the purpose of embolic protection filters in carotid stenting?
What is the difference between CEA and CAS in terms of 30-day stroke or death in symptomatic patients?
What is the difference between CEA and CAS in terms of 30-day stroke or death in symptomatic patients?
What is the role of transcranial doppler in carotid endarterectomy?
What is the role of transcranial doppler in carotid endarterectomy?
What is the most appropriate management strategy for a patient with a minor stroke and 70% stenosis of the left internal carotid artery, with a good 3-5 year life expectancy?
What is the most appropriate management strategy for a patient with a minor stroke and 70% stenosis of the left internal carotid artery, with a good 3-5 year life expectancy?
What is the significance of a 4/5 right-sided weakness in this patient?
What is the significance of a 4/5 right-sided weakness in this patient?
What is the benefit of statin therapy in this patient?
What is the benefit of statin therapy in this patient?
What is the role of biomarkers in carotid disease management?
What is the role of biomarkers in carotid disease management?
What is the indication for Carotid Endarterectomy in this patient?
What is the indication for Carotid Endarterectomy in this patient?
What is the significance of a Left Carotid bruit in this patient?
What is the significance of a Left Carotid bruit in this patient?
What is the role of aspirin in this patient's management?
What is the role of aspirin in this patient's management?
What is the benefit of Carotid Stenting in this patient?
What is the benefit of Carotid Stenting in this patient?
What is the consideration for patients with life expectancy exceeding 5 years?
What is the consideration for patients with life expectancy exceeding 5 years?
What is the average annual risk of ipsilateral stroke in Asx >50% stenosis?
What is the average annual risk of ipsilateral stroke in Asx >50% stenosis?
What is the 5-year risk of carotid territory ischaemic stroke in patients 75+ years old?
What is the 5-year risk of carotid territory ischaemic stroke in patients 75+ years old?
What is the difference in the 5-year risk of carotid territory ischaemic stroke between immediate and deferred treatment?
What is the difference in the 5-year risk of carotid territory ischaemic stroke between immediate and deferred treatment?
What is the role of CAS in patients with Asx CAD >60%?
What is the role of CAS in patients with Asx CAD >60%?
What is the benefit of CAS in the elderly?
What is the benefit of CAS in the elderly?
What is the indication for considering CEA in patients with Asx CAD >60%?
What is the indication for considering CEA in patients with Asx CAD >60%?
What is the presentation of the 67-year-old male in the case scenario?
What is the presentation of the 67-year-old male in the case scenario?
What is the primary consideration for technique selection in revascularization?
What is the primary consideration for technique selection in revascularization?
What is the preferred choice of conduit in open surgery?
What is the preferred choice of conduit in open surgery?
In which patients is open surgery likely better?
In which patients is open surgery likely better?
What is the criterion for selecting endovascular techniques over open surgery?
What is the criterion for selecting endovascular techniques over open surgery?
What is the advantage of covered self-expanding stents?
What is the advantage of covered self-expanding stents?
What is the primary goal of risk factor control in PAD treatment?
What is the primary goal of risk factor control in PAD treatment?
What is the purpose of cilostazol in PAD treatment?
What is the purpose of cilostazol in PAD treatment?
What is the significance of Factor V Leiden in PAD treatment?
What is the significance of Factor V Leiden in PAD treatment?
Flashcards are hidden until you start studying
Study Notes
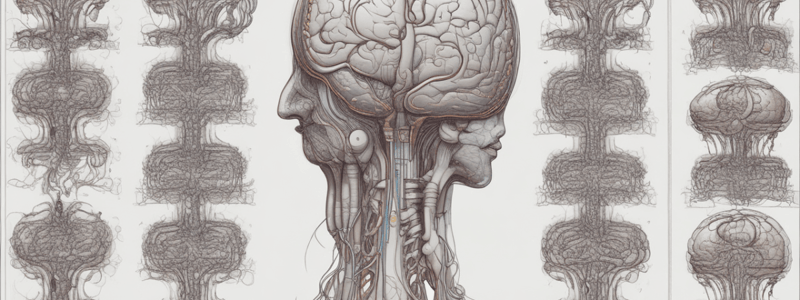
Cerebrovascular Event Classification
- Transient Ischemic Attack (TIA):
- No infarct (cell death)
- Time-based definition: sudden, focal neurologic deficit lasting less than 24 hours
- Tissue-based definition: brief episode of neurologic dysfunction caused by focal brain or retinal ischemia, without evidence of acute infarction
- Stroke (infarct = cell death)
Transient Ischemic Attack Facts
- 10-20% of TIAs will be followed by a stroke within 3 months, half of them within 48 hours
- Among those who present with a stroke, the prevalence of prior TIA is reported to be 7-40%
Stroke
- Infarction of the central nervous system tissue related to hypoperfusion, embolization, thrombosis, or intracranial hemorrhage
- Types:
- Ischemic (85%)
- Hemorrhagic (15%)
Extracranial Atherosclerosis
- Sites:
- Carotid/Vertebral/Aortic Arch
- Types:
- Lacunar (small vessel)
- Cardioembolic
- Miscellaneous (e.g. hypercoagulability, cryptogenic)
Carotid Artery Disease
- Degree/progression of atherosclerotic stenosis
- Plaque quality (stable vs unstable)
- Embolization: primary mechanism responsible for TIA/STROKE
- Vulnerable carotid plaque:
- Unstable plaques are mainly associated with TIA/STROKE
- Identifying vulnerable carotid plaque: clinical information, family history, genetics, imaging, and biological markers
Take Away Messages
- Amaurosis fugax, TIA, or minor stroke are typically a warning sign of a major stroke in the setting of carotid stenosis ≥50%
- Imaging techniques and biomarkers can identify carotid plaque vulnerability
- Risk of stroke with BMT is declining (statins, antiplatelets, antihypertensives, etc.)
- Sx patients with >50% stenosis will benefit from an intervention to prevent a new stroke
- Asx patients with >70% stenosis will benefit from an intervention (to prevent a stroke) provided they have a good 3-5 year life expectancy
- Risk of perioperative stroke with intervention is also declining
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.