Podcast
Questions and Answers
Which statement accurately describes the physiological process of central perfusion?
Which statement accurately describes the physiological process of central perfusion?
- The flow of blood through arteries and capillaries, delivering nutrients and oxygen to cells.
- The volume of blood pumped by the heart in one minute. (correct)
- The exchange of gases between the alveoli and the pulmonary capillaries.
- The electrical activity that initiates myocardial contraction.
How does elevated serum lipids contribute to impaired perfusion?
How does elevated serum lipids contribute to impaired perfusion?
- By enhancing the elasticity of arterial walls.
- By causing vasodilation and increasing blood flow.
- By decreasing the viscosity of blood.
- By promoting the development of atherosclerosis. (correct)
A patient reports experiencing syncope and dizziness. Which assessment would be most relevant to evaluate perfusion?
A patient reports experiencing syncope and dizziness. Which assessment would be most relevant to evaluate perfusion?
- Evaluating range of motion and muscle strength.
- Checking for peripheral edema and auscultating heart sounds. (correct)
- Testing cranial nerve function and mental status.
- Assessing bowel sounds and abdominal tenderness.
Which diagnostic test is most specific for detecting myocardial muscle damage?
Which diagnostic test is most specific for detecting myocardial muscle damage?
What is the primary goal of primary prevention strategies related to perfusion?
What is the primary goal of primary prevention strategies related to perfusion?
What effect does nicotine have on blood vessels?
What effect does nicotine have on blood vessels?
Which assessment finding is most indicative of compromised perfusion?
Which assessment finding is most indicative of compromised perfusion?
How do cardiac enzymes and markers aid in diagnosing cardiovascular conditions?
How do cardiac enzymes and markers aid in diagnosing cardiovascular conditions?
What independent risk factor is suggested by elevated levels of homocysteine (Hcy)?
What independent risk factor is suggested by elevated levels of homocysteine (Hcy)?
For who is stress management/stress reduction most appropriate?
For who is stress management/stress reduction most appropriate?
Which diagnostic result confirms hypertension requiring no additional BP assessment?
Which diagnostic result confirms hypertension requiring no additional BP assessment?
A patient has a mean AOBP that is high during the first visit. According to guidelines, what is the next appropriate step?
A patient has a mean AOBP that is high during the first visit. According to guidelines, what is the next appropriate step?
Which of the following laboratory tests is part of the preliminary investigations for hypertension?
Which of the following laboratory tests is part of the preliminary investigations for hypertension?
A hypertensive patient without diabetes or renal disease asks about routine microalbuminuria testing. What information should the nurse provide?
A hypertensive patient without diabetes or renal disease asks about routine microalbuminuria testing. What information should the nurse provide?
Which of the following assessment findings is a clinical manifestation of hypertension?
Which of the following assessment findings is a clinical manifestation of hypertension?
What dietary recommendation is most appropriate for a patient with hypertension to reduce blood pressure?
What dietary recommendation is most appropriate for a patient with hypertension to reduce blood pressure?
In healthy adults, what is the recommended limit for alcohol consumption to prevent hypertension?
In healthy adults, what is the recommended limit for alcohol consumption to prevent hypertension?
What conditions must be assessed for, before advising patients to increase potassium intake?
What conditions must be assessed for, before advising patients to increase potassium intake?
What statement accurately describes primary or essential hypertension?
What statement accurately describes primary or essential hypertension?
CAD is caused by what?
CAD is caused by what?
When taking a history of a patient complaining of chest pain, what does the 'P' in PQRST mnemonic stand for?
When taking a history of a patient complaining of chest pain, what does the 'P' in PQRST mnemonic stand for?
What are possible clinical manifestations of CAD?
What are possible clinical manifestations of CAD?
According to Lewis, what can isometric exercises of the arms cause?
According to Lewis, what can isometric exercises of the arms cause?
According to presented material, what confirms unstable Angina?
According to presented material, what confirms unstable Angina?
What causes myocardial infarction?
What causes myocardial infarction?
A patient with chest pain is being assessed. After initial interventions, which ongoing monitoring activity is most crucial?
A patient with chest pain is being assessed. After initial interventions, which ongoing monitoring activity is most crucial?
Following percutaneous coronary intervention, what is essential for the nurse to implement?
Following percutaneous coronary intervention, what is essential for the nurse to implement?
What is a cause for Heart Failure?
What is a cause for Heart Failure?
Based of information from the slides, what makes up the pulmonary circuit?
Based of information from the slides, what makes up the pulmonary circuit?
What causes fluid to back up in the body tissues resulting in swelling and edema?
What causes fluid to back up in the body tissues resulting in swelling and edema?
What is a clinical manifestation of the systemic venous congestion form of heart failure?
What is a clinical manifestation of the systemic venous congestion form of heart failure?
Following a heart failure diagnosis, patients will be put on diuretics. Why?
Following a heart failure diagnosis, patients will be put on diuretics. Why?
What is the treatment of varicose veins?
What is the treatment of varicose veins?
Which statement best describes the pathophysiology of deep vein thrombosis (DVT)?
Which statement best describes the pathophysiology of deep vein thrombosis (DVT)?
What is a diagnostic test that can be performed to determine peripheral vascular disease?
What is a diagnostic test that can be performed to determine peripheral vascular disease?
What is important to assess post lower extremity vascular surgery?
What is important to assess post lower extremity vascular surgery?
What are open sores that are inflamed with potential discharge, swelling, heaviness, aching, exhaustion, edema, and pigmentation surrounding the ulcer?
What are open sores that are inflamed with potential discharge, swelling, heaviness, aching, exhaustion, edema, and pigmentation surrounding the ulcer?
What bedside management is appropriate for wound care?
What bedside management is appropriate for wound care?
Flashcards
Perfusion
Perfusion
The flow of blood through arteries and capillaries delivering nutrients and oxygen to cells.
Smoking (Risk Factor)
Smoking (Risk Factor)
Nicotine constricts blood vessels, reducing blood flow.
Elevated Serum Lipids
Elevated Serum Lipids
These contribute to atherosclerosis, hardening arteries.
Sedentary Lifestyle
Sedentary Lifestyle
Signup and view all the flashcards
Obesity (Risk Factor)
Obesity (Risk Factor)
Signup and view all the flashcards
Diabetes (Risk Factor)
Diabetes (Risk Factor)
Signup and view all the flashcards
Hypertension (Risk Factor)
Hypertension (Risk Factor)
Signup and view all the flashcards
Age (Risk Factor)
Age (Risk Factor)
Signup and view all the flashcards
Gender (Risk Factor)
Gender (Risk Factor)
Signup and view all the flashcards
Cardiac Enzymes/Markers
Cardiac Enzymes/Markers
Signup and view all the flashcards
Serum Lipids Test
Serum Lipids Test
Signup and view all the flashcards
Complete Blood Count (CBC)
Complete Blood Count (CBC)
Signup and view all the flashcards
B-type Natriuretic Peptide (BNP)
B-type Natriuretic Peptide (BNP)
Signup and view all the flashcards
ECG (Electrocardiogram)
ECG (Electrocardiogram)
Signup and view all the flashcards
Cardiac Stress Test
Cardiac Stress Test
Signup and view all the flashcards
CXR (Chest X-Ray)
CXR (Chest X-Ray)
Signup and view all the flashcards
Ultrasound (Cardiac)
Ultrasound (Cardiac)
Signup and view all the flashcards
Arteriogram
Arteriogram
Signup and view all the flashcards
Creatine Kinase (CK)
Creatine Kinase (CK)
Signup and view all the flashcards
Cardiac troponins
Cardiac troponins
Signup and view all the flashcards
Myoglobin
Myoglobin
Signup and view all the flashcards
Homocysteine (Hcy)
Homocysteine (Hcy)
Signup and view all the flashcards
Stress Management/Reduction
Stress Management/Reduction
Signup and view all the flashcards
Coronary Artery Disease (CAD)
Coronary Artery Disease (CAD)
Signup and view all the flashcards
Pathogenesis of Atherosclerosis
Pathogenesis of Atherosclerosis
Signup and view all the flashcards
Angina Pectoris
Angina Pectoris
Signup and view all the flashcards
Angina pectoris - Sensation
Angina pectoris - Sensation
Signup and view all the flashcards
"PQRST" ASSESSMENT OF ANGINA
"PQRST" ASSESSMENT OF ANGINA
Signup and view all the flashcards
Factors Precipitating Angina: Physical Exertion
Factors Precipitating Angina: Physical Exertion
Signup and view all the flashcards
Factors Precipitating Angina: Temperature Extremes
Factors Precipitating Angina: Temperature Extremes
Signup and view all the flashcards
Factors Precipitating Angina: Tobacco
Factors Precipitating Angina: Tobacco
Signup and view all the flashcards
Unstable Angina (Preinfarction)
Unstable Angina (Preinfarction)
Signup and view all the flashcards
Myocardial Infarction (MI)
Myocardial Infarction (MI)
Signup and view all the flashcards
Chronic Stable Angina
Chronic Stable Angina
Signup and view all the flashcards
Heart Failure: Treatment
Heart Failure: Treatment
Signup and view all the flashcards
Varicose veins
Varicose veins
Signup and view all the flashcards
Deep Vein Thrombosis (DVT)
Deep Vein Thrombosis (DVT)
Signup and view all the flashcards
Varicose Veins And DVT diagnostic
Varicose Veins And DVT diagnostic
Signup and view all the flashcards
Vaicose veins and DVT treament
Vaicose veins and DVT treament
Signup and view all the flashcards
Stasis Ulcers
Stasis Ulcers
Signup and view all the flashcards
Study Notes
Perfusion
- Perfusion refers to the flow of blood through arteries and capillaries, delivering nutrients and oxygen to cells.
Perfusion Scope
- Optimal Perfusion
- Impaired Perfusion
- No Perfusion
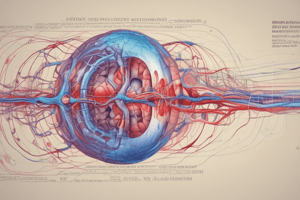
Giddens Concept of Perfusion: Normal Physiologic Process
- Central Perfusion involves:
- Conduction
- Cardiac cycle
- Cardiac output
- Tissue Perfusion also vital for overall perfusion
- Age Related Differences in perfusion as patient ages
Giddens Concept of Perfusion: Variation & Context
- Impaired Central Perfusion can disrupt the entire system
- Impaired Local /Tissue Perfusion affects specific areas
Giddens Concept of Perfusion
- There are Physiological Consequences to impaired Perfusion
- Several Risk Factors contribute to perfusion issues
- There are Populations at Risk, needing special attention
- Individual Risk Factors vary from person to person
Giddens Concept of Perfusion: Individual Risk Factors for Impaired Perfusion
- Modifiable risk factors include:
- Smoking: nicotine vasoconstricts
- Elevated serum lipids: contribute to atherosclerosis
- Sedentary lifestyle: contributes to obesity
- Obesity: increases risk for type 2 diabetes and atherosclerosis
- Diabetes: increases risk of atherosclerosis
- Hypertension: increases work of myocardium
- Unmodifiable risk factors include:
- Age: increases with age
- Gender: men > women
- Genetics: family history
Giddens Concept of Perfusion: Assessment
- Requires a thorough History
- Baseline hx
- Problem based hx:
- Pain
- Syncope
- Dizziness
- Dyspnea
- Edema
- Fatigue
- Incorporates Examination Findings:
- Vital Signs (VS)
- Inspection
- Palpation (chest, extremities)
- Auscultation
Giddens Concept of Perfusion: Diagnostic Tests
- Key Diagnostic Tests:
- Cardiac Enzymes/Markers
- Serum Lipids
- Complete Blood Count
- B-type Natriuretic Peptide (BNP)
- ECG (Electrocardiogram)
- Cardiac Stress Test
- Key Radiologic Studies:
- CXR (Chest X-Ray)
- Ultrasound
- Arteriogram: allows visualization of coronary arteries and heart chambers, involving catheter insertion and contrast injection for visualizing patency
- Venogram
Cardiac Enzymes/Markers
- Enzymes released from damaged cells circulate in the blood
- Can be measured to confirm number of cardiovascular conditions.
- Creatine kinase (CK) is an enzyme present in myocardium (CK-MB), muscle (CK-MM), and brain (CK-BB) tissues, with elevated CK-MB levels 3-6 hours after myocardial infarction.
- Cardiac troponins are myocardial muscle proteins released after myocardial injury, important for their high specificity for cardiac damage and used in evaluating patients with suspected acute coronary syndromes.
- Myoglobin is an oxygen-binding protein in cardiac and skeletal muscles, with increased levels indicating cardiac injury or death about 3 hours after infarction.
- Homocysteine (Hcy) is an amino acid, where elevated levels may act as an independent risk factor for ischemic heart disease, cerebrovascular disease, and peripheral arterial disease.
Giddens Concept of Perfusion: Clinical Management
- Focuses on Primary Prevention through:
- Baseline hx
- Problem based hx:
- Pain
- Syncope
- Dizziness
- Dyspnea
- Edema
- Fatigue
- Secondary Prevention (Screening) includes:
- BP screening
- Lipid Screening
Giddens Concept of Perfusion: Collaborative Interventions
- Crucial Collaborative Interventions:
- Stress Management/Stress Reduction
- Nutrition Therapy
- Smoking Cessation
- Activity & Exercise
- Pharmacotherapy
Perfusion and Interrelated Concepts
- Perfusion is linked with
- Pain
- Stress and Coping
- Cognition
- Intracranial Regulation
- Elimination
- Inflammation
- Gas Exchange
- Patient Education
- Clotting
- Nutrition
- Mobility
Cardiovascular Health Challenges: Hypertension
- Hypertension Diagnostic Algorithm for Adults includes:
- Elevated BP Suspected (office, home or pharmacy)
- Office Visit Assessment of BP
- Mean Office BP > 180/110 leads to probable HTN.
- If Mean Office BP is is not Greater than/equal to 180/110:
- Check for diabetes
- If present measure OBPM
- If diabetes not present check AOBP
- Follow decision tree in diagram
- Check for diabetes
Hypertension Diagnosis Algorithm Notes
- AOBP stands for Automated Office Blood Pressure, performed with the patient unattended in a private room. OBPM: Office Blood Pressure Measurement and performed in office using electronic upper arm device with a provider in the room.
- ABPM: Ambulatory Blood Pressure Monitoring
- HBPM: Home Blood Pressure Monitoring
- WCH: White Coat Hypertension
- HTN: Hypertension
Hypertension: Mean Office BP ≥ 180/110 mmHg
- If Mean office BP ≥ 180/110 mmHg, the diagnosis is hypertensive emergency
- There is no need for additional BP assessment to make the hypertension diagnosis
- Diagnose with hypertension and initiate treatment
Patient Evaluation: Assessment
- BP should be assessed in all adult patients at all appropriate visits to determine cardiovascular risk and monitor antihypertensive treatment.
- Routine Lab Testing: Preliminary investigations of patients with hypertension
- Urinalysis
- Blood chemistry (potassium, sodium and creatinine)
- Fasting blood glucose and/or glycated hemoglobin (A1c)
- Serum total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), non-HDL cholesterol, and triglycerides; lipids may be drawn fasting or non-fasting
- Standard 12-lead ECG
- Follow-up investigations of patients with hypertension are necessary
Follow-up Investigations & Target Organ Damage
- Tests, including electrolytes, creatinine, fasting lipids, and pregnancy tests, should be repeated with a frequency reflecting the clinical situation during the maintenance phase of hypertension management.
- Consider pregnancy testing when initiating health changes or drug therapy.
- Target Organ Damage (TOD) should be assessed in patients with hypertension.
- Presence of any of the following would put a patient into the moderate-to-high or high-risk categories for therapy
- Cardiovascular Disease, Cerebrovascular Disease, Hypertensive Retinopathy
Target Organ Damage: Continued
- Peripheral Arterial Disease
- Renal Disease
- Global Cardiovascular Risk Assessment
- Multifactorial risk assessment models can be used to more accurately predict global cardiovascular risk and antihypertensive therapy.
- Assessments can be done through risk calculators such as:
- Improve Risk Factor Modification; Inform patients of their global risk and consider using analogies that describe comparative risks like "cardiovascular age", "vascular age", or "heart age”.
Hypertension: Assess CV Risk Factors
- History of clinically overt ASCVD (eg, PAD, stroke, TIA)
- Nonmodifiable:
- Age ≥ 55 years
- Male sex
- Family history of premature CVD (age < 55 in men and < 65 in women)
- Modifiable:
- Sedentary lifestyle
- Poor dietary habits
- Abdominal obesity
- Dysglycemia
- Smoking
- Dyslipidemia
- Stress
- Nonadherence
Hypertension: Clinical Manifestations
- Usually asymptomatic-"The Silent Killer”.
- May cause headache, dizziness, blurred vision when greatly elevated.
Hypertension: Routine and Optional Lab Testing
- Routine Tests:
- Urinalysis
- Blood chemistry (potassium, sodium, and creatinine)
- Fasting blood glucose and/or A1C
- Serum total cholesterol, LDL-C, HDL-C, non-HDL-C and triglycerides
- Standard 12-lead electrocardiography
- Optional tests (clinical circumstance):
- Patients with diabetes (ACR, and according to Diabetes Canada guidelines)
- Pregnancy test
- Echocardiogram (when clinically relevant)
- Left ventricular ejection fraction assessment (when evidence of heart failure)
Hypertension: Thresholds and Targets
- Hypertension Canada stratifies patients by cardiovascular risk and, based on that risk, there are different thresholds and targets for treatment.
- Hypertension Canada
High-Risk Patient for intensive BP management:
- Individuals ≥50y AND with SBP 130-180 mmHg AND
- With one or more of the following CV risk factors
- Should be considered for intensive BP management:
- Clinical or sub-clinical cardiovascular disease
- Chronic kidney disease
- (non-diabetic nephropathy, proteinuria <1g/d, *estimated glomerular filtration rate 20-59 mL/min/1.73m²)
- OR
- Estimated 10-year global cardiovascular risk ≥15%
Populations and Stratification
- Age ≥75 years
- OR
- Four variable Modification of Diet in Renal Disease (MDRD) equation
- Framingham Risk Score
- Attaining blood pressure targets is vital to prevent cardiovascular and cerebrovascular complications in patients with documented hypertension.
Population Blood Pressure Thresholds
- Blood pressure thresholds for initiation of antihypertensive therapy and treatment targets in adults:
- Hypertension Canada High-Risk Patient: if SBP is equal to or greater than 130, target SBP is less than 120
- Diabetes mellitus: if SBP is equal to or greater than 130 and DBP greater than 80, target SBP is less than 130 and DBP less than 80
- Moderate-to-high Risk (TOD or CV risk factors): if SBP is equal to or greater than 140 and DBP greater than 90, target SBP is less than 140 and DBP less than 90
- Low Risk (No TOD or CV risk factors): if SBP is equal to or greater than 160 and DBP greater than 100, target SBP is less than 140 and DBP less than 90
Hypertension Therapy: Health Behaviour Recommendations
- Health Behaviour Recommendations include:
- Being More Physically Active
- Weight Reduction
- Moderation in Alcohol Intake
- Eating Healthier
- Relaxation Therapies
- Smoking Cessation
- Objective recommendation summary in slide
Health Behaviours
- Physical Exercise:
- 30-60 minutes of moderate-intensity dynamic exercise (eg, walking, jogging, cycling, or swimming) 4-7 days per week
- Higher intensities of exercise are not effective
- Use of resistance or weight training exercise (such as free-weight lifting, fixed-weight lifting, or handgrip exercise) does not adversely influence BP
- Weight Reduction:
- Assess height, weight and waist circumference and calculate BMI
- Maintenance of a healthy weight is recommended
- All hypertensive patients with a BMI > 25 kg/m² should be advised to lose weight
- Alcohol:
- In healthy adults, abstaining from alcohol or reducing alcohol intake to 2 drinks per day or less to prevent hypertension
Health Behaviours Continued
- Diet:
- High in fruit, vegetables, low-fat dairy products, whole grain foods rich in dietary fibre and protein from plant sources that is reduced in saturated fat and cholesterol (DASH)
- Sodium:
- ↓intake to 2000 mg/day
- Calcium and magnesium:
- Not recommended
- Potassium
- If not at risk of hyperkalemia, ↑to reduce BP
- Stress management
- Individualized cognitive-behavioural interventions are more likely to be effective when relaxation techniques are used
Risk Factors of Hyperkalemia
- Assess for those at high risk of hyperkalemia before advising increased potassium intake:
- Patients taking renin-angiotensin-aldosterone inhibitors
- Patients taking other drugs that can cause hyperkalemia (eg, trimethoprim and sulfamethoxazole, amiloride, triamterene)
- Chronic kidney disease (glomerular filtration rate < 45 mL/min/1.73 m²)
- Baseline serum potassium > 4.5 mmol/L
BP Thresholds for Initiation and Targets by Patient Population
- Low risk (no target organ damage or CV risk factors)
- BP Initiation > SBP 160 or DBP 100
- BP Target < SBP 140 or DBP 90
- High risk of CVD*:
- BP Initiation > SBP 130
- BP Target < SBP 120
- Diabetes mellitus:
- BP Initiation > SBP 130 or DBP 80
- BP Target < SBP 130 or DBP 80
- All others:
- BP Initiation > SBP 140 or DBP 90
- BP Target < SBP 140 or DBP 90
- **Measured by automated office blood pressure measurement
Hypertension: Dx Key Messages
- Hypertension remains the most prevalent risk factor for cardiovascular disease in Canada
- Standardized BP measurement, using validated protocols and devices, continues to be recommended to screen for cases of hypertension
- Frequency and timing of screening can be tailored to each patient's risk of hypertension.
- Common risk factors for hypertension include:
- Diabetes mellitus
- Chronic kidney disease
- Low level of consumption of fresh fruits and vegetables
- Sedentary behaviour
Hypertension Measurement Key Messages
- Use of out-of-office measurement (24-hour ambulatory BP monitoring [ABPM] or home BP monitoring [HBPM]) is recommended for all adults with:
- High in-office BP to rule out white coat hypertension
- Suspected hypertension (including adults with diabetes) to rule out masked hypertension
- Adults with confirmed diagnosis of hypertension should have a baseline assessment of:
- Cardiovascular risk factors (including screening for diabetes, hyperlipidemia, and renal disease)
- Target organ damage
- Routine lab testing.
- The possibility of pregnancy should be considered in all women of reproductive age with a new diagnosis of hypertension, and during follow-up visits
Types of Hypertension
- Primary or Essential Hypertension:
- Causes of hypertension are absent and accounts for Approximately 90-95% of clients
- Secondary Hypertension:
- Causative factors are present and account for Approximately 5% of clients
Hypertension: Untreated
- Untreated chronic high blood pressure (hypertension) can lead to:
- Stroke
- Eye damage
- Blood vessel damage (arteriosclerosis)
- Heart attack or heart failure
- Kidney failure
Cardiovascular Health Challenges: Coronary Artery Disease
- CAD is caused by Atherosclerosis-a buildup of plaque in the arteries to the heart.
Atherosclerosis
- Involves the progression of arterial plaque:
- From fatty streaks to fibrous plaques,
- Can result in complicated lesions with hemorrhage, ulceration, calcification, and thrombosis.
- range of effects from stroke, infarct and gangrene
Pathogenesis of Atherosclerosis
- Chronic Endothelial Injury, involving:
- Hypertension
- Tobacco use
- Hyperlipidemia
- Hyperhomocysteinemia
- Diabetes
- Infections
- Toxins
- Damaged endothelium, progresses to Fatty Streak
- Lipids accumulate and migrate into smooth muscle cells.
- Fibrous Plaque results from:
- Collagen covers the fatty streak
- Vessel lumen is narrowed
- Blood flow is reduced
- Fissures can develop
- Compliated Lesion results from:
- Plaque rupture
- Thrombus formation
- Further narrowing or total occlusion of vessel
Risk Factors for Coronary Artery Disease
- Nonmodifiable Risk Factors:
- Increasing age
- Sex (men > women until 65 yr of age)
- Ethnicity (Black people > White people)
- Genetic predisposition and family history of heart disease
- Modifiable Risk Factors:
- Serum lipid alterations: elevated triglyceride and LDL cholesterol levels, decreased HDL levels
- Blood pressure ≥140/90 mm Hg
- Tobacco use
- Physical inactivity
- Obesity: waist circumference ≥102 cm (40 inches) in men and ≥88 cm (35 inches) in women
- Contributing Factors:
- Diabetes mellitus
- Elevated fasting blood glucose level
- Psychosocial risk factors (e.g., depression, hostility and anger, stress)
- Elevated homocysteine levels
- Substance use
CAD Clinical Manifestations
- Chest pain (Angina pectoris), causing inadequate blood flow to the heart; resulting in:
- Sensation of heaviness, choking or suffocation
- Frequently retrosternal & may radiate to neck, jaw, shoulders, back or arms
- Dyspnea, diaphoresis, tachycardia, and high blood pressure.
- Heart attack (Myocardial infarction), resulting in sudden total blockage of a coronary artery.
- Sudden death: fatal rhythm disturbance.
Angina Pectoris
- Angina:
- Type of chest pain, pressure or discomfort.
- Causes:
- Pain in the chest radiating up to the jaw (or down the left (or, less often, right) arm) signals a heart attack
- Reversible angina from increased demand on heart.
- Progressive angina associated with heart attack.
Angina Assessment
- PQRST mnemonic is used to assess and ask questions about angina:
- P: What events or activities precipitated the pain/discomfort (e.g., argument, exercise, resting)?
- Q: What does the pain/discomfort feel like (e.g., pressure, dull, aching, tight, squeezing)?
- R: Where is the pain/discomfort located? Does the pain radiate to other areas (e.g., back, arms, jaw, teeth, shoulder, elbow)?
- S: On a scale of 0 to 10, with 10 being the most severe pain you could imagine, how would you rate the pain/discomfort?
- T: When did the pain/discomfort begin? Has the pain/discomfort changed since this time? Have you had pain like this before?
Angina Considerations
- Common locations of pain during angina or myocardial infarction:
- Midsternal
- Left shoulder and down both arms
- Neck and arms
- Substernal radiating to neck and jaw
- Substernal radiating down left arm
- Epigastric
- Epigastric radiating to neck, jaw, and arms
- Intrascapular
Factors Precipitating Angina
- Physical Exertion:
- Causing an increase in myocardial oxygen demand.
- Isometric exercise of the arms (e.g., raking, lifting heavy objects, or shovelling snow) can cause exertional angina.
- Temperature Extremes:
- Blood vessels constrict in response to a cold stimulus.
- Blood vessels dilate and blood pools in the skin in response to a hot stimulus.
- Strong Emotions:
- The sympathetic nervous system is stimulated.
- The workload of the heart is increased.
- Consumption of Heavy Meal
- Blood is diverted to the GI system, which reduces blood flow in the coronary arteries
- Tobacco Use:
- Nicotine stimulates catecholamine release, causing vasoconstriction and an increase in HR.
- Tobacco diminishes available oxygen by increasing the level of carbon monoxide.
Factors Precipitating Angina Continued
- Sexual Activity: increase of cardiac workload
- Stimulants: HR and subsequent myocardial oxygen demand are increased.
- Circadian Rhythm Patterns:
- Related to the occurrence of chronic stable angina, Prinzmetal's angina, myocardial infarction, and sudden cardiac death.
- Manifestations of CAD tend to occur in the early morning after the patient awakens.
Types of Angina
- Stable Angina:
- Provoked by exertion or emotional stress.
- Lasts for 5 to 15 minutes after stopping activity.
- Relieved by rest and (NTG) nitroglycerin (within 1 minute).
- Unstable Angina (Preinfarction):
- Occurs at rest or with little physical exertion and is CP new in onset
- No increase in oxygen demand and acute lack of blood flow to the heart due to presence of plaque.
- Pain increases in frequency and severity in Worsening pattern
- Women often have prodrome symptoms such as fatigue, SOB, indigestion, and anxiety
- Not relieved by rest and NTG and is a sign of a heart attack for MI
Myocardial Infarction
- An area of the myocardium is permanently destroyed due to:
- Atherosclerosis
- Thrombus
CAD Diagnostic Tests
- Diagnostic tests and relevant visuals are indicated in the slide
CAD Collaborative Therapy
- Chronic Stable Angina
- Drug therapy includes:
- Antiplatelet therapy (e.g., ASA Aspirin], clopidogrel [Plavix])
- Nitroglycerin
- ACE inhibitors, ARBs
- β-adrenergic blockers
- Calcium channel blockers
- Lipid-lowering drugs
- Management of Risk Factors:
- Management of risk factors for coronary artery disease
- Coronary Revascularization
- PCI or CABG surgery
- Drug therapy includes:
- Acute Coronary Syndrome:
- Involves 12-lead and continuous ECG monitoring
- IV access and O2 therapy
- Drug therapy includes:
- Nitroglycerin, Morphine sulfate, ASA
- β-adrenergic blockers - ACE inhibitors and ARBs
- Unstable Angina/ Non-ST-Segment-Elevation MI (NSTEMI):
- Involves Acute intensive drug therapy and Nitroglycerin
- Involves Antiplatelet therapy for example: ASA, clopidogrel, glycoprotein IIb/IIla inhibitors
- Also calls for Anticoagulation therapy such as Heparin, direct thrombin inhibitors
- Requires Coronary Angiography as well as PCI
- STI segment Elevation
- Emergent reperfusion therapy through PCI or Thrombolytic therapy
- CABG surgery
- Concurrent drug therapy includes Antiplatelet therapy
Emergency Management: Chest Pain
- The key elements to assessing and managing chest pain:
- Cardiovascular
- Etiology includes angina, myocardial infarction, dysrhythmia pericarditis, aortic aneurism and aortic valve disease
- Assessment findings:Pain in chest, neck, arm, or shoulder, Cold, clammy skin,Diaphoresis, Nausea and vomiting, Epigastric pain, Indigestion or heartburn, Dyspnea, Weakness Anxiety, Feeling of impending doom, Tachycardia and Irregular HR as well as murmurs -Palpitations and dysrhythmias result in Decreased blood pressure and Narrowed pulse pressure as well as unequal BP readings in upper extremities, Syncope, loss of consciousness, andDecreased O₂ saturation.
- Respiratory: Etiology includes:
- Costochondritis, Pleurisy
- Pneumonia
- Pneumothorax
- Pulmonary edema
- Pulmonary embolus
- Assessment Findings:Decreased or absent breath sounds, Crackles, wheezes
- Chest Trauma:
- Etiology includes: Rib or sternal fracture,Flail chest,Cardiac tamponade
- Assessment Findings: Pericardial friction rub
- Etiology includes: Rib or sternal fracture,Flail chest,Cardiac tamponade
- Initial Assessment:
- Maintain the patient airway
- Ensure vitals, administer oxygen
- Obtain a 12 lead ECG
- Insert two IV catheters.
- Assess pain using PQRST method.
- Provide scheduled medication to ease pain.
- Continuous ECG monitoring.
- Portable chest radiograph.
- Baseline test. - Asses CPR protocol, administer aspirin, B-adrenergic blockers or antidysrhythmic meds
Chest Pain Ongoing Monitoring
- Monitoring includes:
- Maintaining vitals, oxygen saturation
- Monitoring patient response to their meds and pain management
- Provide family and patient support, explaining procedures simply
- Prepare for intubation and possible CPR or cardioversion if needed.
Percutaneous Coronary Interventions
- Involves the insertion of a guiding cather and use of Balloon Angioplasty
Percutaneous Coronary Interventions with Stent
- Stent implantation involves multiple steps to clear blockages.
CAD Nursing Interventions
- Oxygen therapy with O2 at 2 to 4 L/min via nasal cannula or as ordered.
- Administer medications as needed.
- Manage pain with morphine, positioning and a Diet-low cholesterol, low sodium.
- Restrict activities and promote sleep
- Monitor ECG, vital signs, mental status, I.O., weight, treatments.
- Educate client and family on lifestyle changes and pain managment
Heart Failure (HF)
- Inability of the heart to pump sufficient blood to meet the needs of the tissues for oxygen and nutrients; commonly found in those 65+
Heart Failure Pathophysiology
- Complex in nature and described in slide example
Types of Heart Failure
- Right Heart Failure:
- Inability of the right side of the heart to adequately pump venous blood into the pulmonary circulation.
- The condition Causes systemic edema
- Left Heart Failure:
- Inability of the left side of the heart to pump into systemic circulation.
- Causes fluid into lungs
Heart Failure Clinical Manifestations
- Right-Sided Failure caused by Systemic Venous Congestion:
- Weight gain from fluid accumulation and Edema in the ankle or sacral region. -Gl symptoms
- Distended jugular (neck) veins.
- Left-Sided Failure caused by Pulmonary Congestion:
- Dyspnea with an anxiety
- Nonproductive cough with crackles in the lungs
- Fatigue
Heart Failure: Dx and Tx
- Diagnostic tests include:
- CXR, ECG, ABG, and blood tests (renal function tests, electrolytes).
- Symptomatic can be releived though: -Symptomatic relieve and medications as well as nursing intervention, such has with CAD patients
Peripheral Vascular Diseases
- Varicose Veins and DVT (Deep Vein Thrombosis)
Varicose veins and DVT: Types
- Varicose veins involve:
- Swollen, twisted, and painful veins filled with abnormal collection of blood.
- DVT involves: -Formation of a blood clot (thrombus) in a deep vein.
Varicose veins and DVT: Risks
- Varicose Viens:
- Family history, Pregnancy and Obesity
- Aging, Prolonged bed rest and Smoking
- DVT:
- Pathophysiology
- Manifest via normal vessel clots
Varicose veins and DVT: Manifestions
- Varicose Veins:
- Characterized clinicaly by:
- Leg fatigue and aching with leg cramping, as well as pain, Swollen legs, Dilated veins, and Ankle edema.
- DVT:
- Diagnostic Tests include: Client history and Physical Examination, as well as venography andD oppler ultrasound on legs
Varicose veins and DVT: Diagnostics
- Venous anatomy and indications show a normal and deep vein thrombosis comparison
Varicose veins and DVT: Treatments
- Treatments include:Rest with elevation of legs; exercise, anti-embolic stocking;
- Avoid prolong standing,sitting and crossing the legs; manage weight; surgical vein stripping (varicose veins) and anticoagulant therapy (DVT).
- Nursing Interventions include:
- Ensure Post surgery assessment of legs (color, movement, temperature and sensation); encourage leg exercises and client education.
Stasis Ulcers
- Stasis ulcers or venous ulcers are wounds that occur due to improper functioning of venous valves, commonly found in the lower extremities.
- Manifest Open sore that is inflamed and causes swelling, heaviness, fatigue with pigmention
- Results from inadequate oxygen and other nutrients to the tissues.
- Diagnostics can be through venous doppler showings of wound cultures Treatments include compression dressings. Also skin graphs
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.