Podcast
Questions and Answers
Which of the following physiological processes primarily contributes to an increased risk of fractures in individuals over the age of thirty?
Which of the following physiological processes primarily contributes to an increased risk of fractures in individuals over the age of thirty?
- Equal rates of bone remodeling maintaining bone density
- Decreased osteoclast activity, resulting in reduced calcium release from bone.
- Increased osteoblast activity, leading to denser bone formation.
- Osteoclast activity outpacing osteoblast activity, leading to decreased bone density. (correct)
What is the priority nursing intervention for a client who has sustained a fracture upon arrival to the emergency department?
What is the priority nursing intervention for a client who has sustained a fracture upon arrival to the emergency department?
- Immobilizing the affected extremity with a splint.
- Administering pain medication as prescribed.
- Maintaining airway, breathing, and circulation (ABCs). (correct)
- Assessing neurovascular status of the affected extremity.
When caring for a patient with a suspected bone fracture, which assessment finding would be considered a late sign?
When caring for a patient with a suspected bone fracture, which assessment finding would be considered a late sign?
- Muscle spasms near fracture.
- Edema at the injury site.
- Ecchymosis around the injury area.
- Subcutaneous emphysema. (correct)
A client with a fractured femur reports intense pain that is not relieved by opioid analgesics. Which complication should the nurse suspect?
A client with a fractured femur reports intense pain that is not relieved by opioid analgesics. Which complication should the nurse suspect?
What is the primary purpose of traction in the management of a fractured extremity?
What is the primary purpose of traction in the management of a fractured extremity?
Which laboratory finding indicates the highest risk for bleeding complications in a client with a fractured pelvis?
Which laboratory finding indicates the highest risk for bleeding complications in a client with a fractured pelvis?
A patient with a long bone fracture develops dyspnea, confusion, and a petechial rash. Which complication is most likely occurring?
A patient with a long bone fracture develops dyspnea, confusion, and a petechial rash. Which complication is most likely occurring?
Which nursing intervention is most important for preventing osteomyelitis in a client with an open fracture?
Which nursing intervention is most important for preventing osteomyelitis in a client with an open fracture?
A client with a fractured hip reports new-onset sharp pain with movement and stiffness in the affected joint months after the injury. What complication should the nurse suspect?
A client with a fractured hip reports new-onset sharp pain with movement and stiffness in the affected joint months after the injury. What complication should the nurse suspect?
A nurse is providing discharge instructions to a client with a lower extremity fracture who has been prescribed opioid analgesics for pain relief. Which statement is most important to include?
A nurse is providing discharge instructions to a client with a lower extremity fracture who has been prescribed opioid analgesics for pain relief. Which statement is most important to include?
Which type of fracture is most commonly associated with physical abuse, especially in children?
Which type of fracture is most commonly associated with physical abuse, especially in children?
What is the primary reason for performing neurovascular assessments on an extremity immobilized with a cast?
What is the primary reason for performing neurovascular assessments on an extremity immobilized with a cast?
A client with a fracture is prescribed a diet high in protein and calcium. What is the primary rationale?
A client with a fracture is prescribed a diet high in protein and calcium. What is the primary rationale?
Which diagnostic procedure is most effective for identifying hairline fractures and complications related to delayed healing?
Which diagnostic procedure is most effective for identifying hairline fractures and complications related to delayed healing?
Which health promotion activity is most beneficial for preventing fractures related to osteoporosis in a postmenopausal woman?
Which health promotion activity is most beneficial for preventing fractures related to osteoporosis in a postmenopausal woman?
What is the primary goal of using a splint or immobilizer on a fractured extremity before casting?
What is the primary goal of using a splint or immobilizer on a fractured extremity before casting?
What is the primary purpose of skin traction, such as Buck's traction, in the preoperative management of a client with a hip fracture?
What is the primary purpose of skin traction, such as Buck's traction, in the preoperative management of a client with a hip fracture?
A client with a fractured tibia reports increased pain, numbness, and pallor in the toes. Which action should the nurse take first?
A client with a fractured tibia reports increased pain, numbness, and pallor in the toes. Which action should the nurse take first?
A patient with a long bone fracture is at risk for fat embolism. What early signs should the nurse monitor for?
A patient with a long bone fracture is at risk for fat embolism. What early signs should the nurse monitor for?
What is the best approach to provide pin site care for a client in skeletal traction?
What is the best approach to provide pin site care for a client in skeletal traction?
A client who had a long leg cast applied 2 days ago for a tibia fracture reports itching under the cast. What is the best recommendation the nurse can offer?
A client who had a long leg cast applied 2 days ago for a tibia fracture reports itching under the cast. What is the best recommendation the nurse can offer?
Which manifestation differentiates a fat embolism from a pulmonary embolism following a fracture?
Which manifestation differentiates a fat embolism from a pulmonary embolism following a fracture?
A nurse is caring for an older adult client with a hip fracture. Which risk factor would be most important to address to prevent future fractures?
A nurse is caring for an older adult client with a hip fracture. Which risk factor would be most important to address to prevent future fractures?
Which nursing intervention is most important for a client following a fasciotomy to treat compartment syndrome?
Which nursing intervention is most important for a client following a fasciotomy to treat compartment syndrome?
A nurse is educating a client about the use of NSAIDs for pain management after a fracture. Which statement is most important to include?
A nurse is educating a client about the use of NSAIDs for pain management after a fracture. Which statement is most important to include?
Which intervention is most important for a client experiencing complex regional pain syndrome (CRPS) following a fracture?
Which intervention is most important for a client experiencing complex regional pain syndrome (CRPS) following a fracture?
After removal of a cast, a client experiences decreased range of motion and stiffness in the affected joint. Which intervention should the nurse recommend?
After removal of a cast, a client experiences decreased range of motion and stiffness in the affected joint. Which intervention should the nurse recommend?
A client with a fractured femur is prescribed balanced suspension traction. What is the primary benefit of this type of traction?
A client with a fractured femur is prescribed balanced suspension traction. What is the primary benefit of this type of traction?
What is the most common cause of hip fractures in older adults?
What is the most common cause of hip fractures in older adults?
Which assessment finding is indicative of a late stage of compartment syndrome?
Which assessment finding is indicative of a late stage of compartment syndrome?
What is the primary goal of closed reduction in the management of a fracture?
What is the primary goal of closed reduction in the management of a fracture?
Which type of pathological fracture is most commonly associated with metastatic cancer?
Which type of pathological fracture is most commonly associated with metastatic cancer?
A client is being discharged after undergoing open reduction and internal fixation (ORIF) for a fractured ankle. What is most important for the nurse to teach the client regarding wound care?
A client is being discharged after undergoing open reduction and internal fixation (ORIF) for a fractured ankle. What is most important for the nurse to teach the client regarding wound care?
What is a malunion fracture?
What is a malunion fracture?
What is the primary reason for elevating a fractured extremity?
What is the primary reason for elevating a fractured extremity?
An older adult client is admitted with a hip fracture following a fall. Which of the following interventions is most important to prevent venous thromboembolism?
An older adult client is admitted with a hip fracture following a fall. Which of the following interventions is most important to prevent venous thromboembolism?
A client with a fractured femur develops petechiae on the chest and neck, along with dyspnea and confusion, 24 hours post-injury. Which of the following conditions should the nurse suspect?
A client with a fractured femur develops petechiae on the chest and neck, along with dyspnea and confusion, 24 hours post-injury. Which of the following conditions should the nurse suspect?
A client who sustained a tibia fracture is being discharged home with a cast. Which statement indicates the client understands important cast care instructions?
A client who sustained a tibia fracture is being discharged home with a cast. Which statement indicates the client understands important cast care instructions?
A client with an open fracture of the radius is scheduled for surgical repair. Which intervention is most important to include in the client’s plan of care to prevent osteomyelitis?
A client with an open fracture of the radius is scheduled for surgical repair. Which intervention is most important to include in the client’s plan of care to prevent osteomyelitis?
A client with a femur fracture is in balanced suspension traction. Which nursing action is essential to ensure effective traction?
A client with a femur fracture is in balanced suspension traction. Which nursing action is essential to ensure effective traction?
Flashcards
Fracture
Fracture
A break in a bone, usually due to trauma or a pathological condition.
Traumatic Fracture
Traumatic Fracture
Fractures caused by a physical impact or injury.
Pathological Fracture
Pathological Fracture
Fractures caused by underlying disease (e.g., cancer, osteoporosis).
Osteoclasts
Osteoclasts
Signup and view all the flashcards
Osteoblasts
Osteoblasts
Signup and view all the flashcards
Comminuted Fracture
Comminuted Fracture
Signup and view all the flashcards
Oblique Fracture
Oblique Fracture
Signup and view all the flashcards
Spiral Fracture
Spiral Fracture
Signup and view all the flashcards
Impacted Fracture
Impacted Fracture
Signup and view all the flashcards
Greenstick Fracture
Greenstick Fracture
Signup and view all the flashcards
ABCs of emergency care
ABCs of emergency care
Signup and view all the flashcards
Crepitus
Crepitus
Signup and view all the flashcards
Ecchymosis
Ecchymosis
Signup and view all the flashcards
Subcutaneous Emphysema
Subcutaneous Emphysema
Signup and view all the flashcards
Neurovascular Assessment
Neurovascular Assessment
Signup and view all the flashcards
Five P's
Five P's
Signup and view all the flashcards
Fasciotomy
Fasciotomy
Signup and view all the flashcards
Fat Embolism
Fat Embolism
Signup and view all the flashcards
Petechiae
Petechiae
Signup and view all the flashcards
Osteomyelitis
Osteomyelitis
Signup and view all the flashcards
Osteomyelitis Pain
Osteomyelitis Pain
Signup and view all the flashcards
Avascular Necrosis
Avascular Necrosis
Signup and view all the flashcards
Delayed Union
Delayed Union
Signup and view all the flashcards
Malunion
Malunion
Signup and view all the flashcards
Nonunion
Nonunion
Signup and view all the flashcards
Complex Regional Pain Syndrome (CRPS)
Complex Regional Pain Syndrome (CRPS)
Signup and view all the flashcards
Heterotopic Ossification
Heterotopic Ossification
Signup and view all the flashcards
Closed Reduction
Closed Reduction
Signup and view all the flashcards
Splint/Immobilizer
Splint/Immobilizer
Signup and view all the flashcards
Traction
Traction
Signup and view all the flashcards
Straight/Running Traction
Straight/Running Traction
Signup and view all the flashcards
Balanced Suspension Traction
Balanced Suspension Traction
Signup and view all the flashcards
Skeletal Traction
Skeletal Traction
Signup and view all the flashcards
Pressure compromises circulation.
Pressure compromises circulation.
Signup and view all the flashcards
What is a spiral fracture?
What is a spiral fracture?
Signup and view all the flashcards
What is an impacted fracture?
What is an impacted fracture?
Signup and view all the flashcards
What is a greenstick fracture?
What is a greenstick fracture?
Signup and view all the flashcards
What is immediate fracture care?
What is immediate fracture care?
Signup and view all the flashcards
What are the 5 P's of neurovascular compromise?
What are the 5 P's of neurovascular compromise?
Signup and view all the flashcards
What is the treatment for compartment syndrome?
What is the treatment for compartment syndrome?
Signup and view all the flashcards
What is osteomyelitis?
What is osteomyelitis?
Signup and view all the flashcards
What can circulatory compromise after a fracture result in?
What can circulatory compromise after a fracture result in?
Signup and view all the flashcards
What occurs when a bone doesn't heal correctly?
What occurs when a bone doesn't heal correctly?
Signup and view all the flashcards
What can poorly managed acute pain lead to?
What can poorly managed acute pain lead to?
Signup and view all the flashcards
What is the growth of bone in soft tissues?
What is the growth of bone in soft tissues?
Signup and view all the flashcards
Study Notes
-
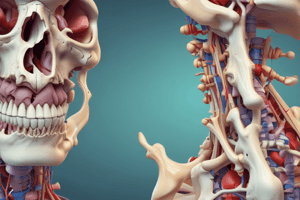
A fracture is a bone break caused by trauma or a pathological condition. Trauma-induced fractures are the most common. Pathological fractures result from metastatic cancer, osteoporosis, or Paget’s disease.
-
Bone remodeling involves osteoclasts (cells that dissolve bone) releasing calcium and osteoblasts (cells that form new bone). Bone remodeling rates are equal until the age of thirty when osteoclast activity surpasses osteoblast activity, increasing the risk of osteoporosis and subsequent fractures, especially after menopause.
Common Types of Fractures
- Comminuted: The bone is fragmented.
- Oblique: The fracture occurs at an oblique angle across the bone.
- Spiral: The fracture results from a twisting motion and is common in physical abuse cases.
- Impacted: The fractured bone is wedged inside the opposite fractured fragment.
- Greenstick: The fracture occurs on one side (cortex) but doesn't extend completely through the bone; it's most common in children.
- Hip fractures are common in older adults, usually from falls.
Nursing Care
- Provide immediate emergency care, focusing on maintaining ABCs (Airway, Breathing, Circulation).
- Monitor vital signs and neurological status to detect injuries to vital organs from bone fragments, especially in pelvis or rib fractures.
- Check urine for blood.
- Stabilize the injured area, including joints above and below the fracture, using a splint to avoid unnecessary movement.
- Ask about the cause of injury to assess for other potential internal injuries.
- Properly align the affected extremity.
- Elevate the limb above the heart and apply ice.
- Assess for bleeding, applying pressure if needed.
- Cover open wounds with a sterile dressing.
- Remove clothing and jewelry near the injury or on the affected extremity.
- Keep the client warm.
- Assess pain frequently and follow pain management protocols, both pharmacological and non-pharmacological.
- Conduct neurovascular checks at least every hour, reporting any changes immediately.
- Prepare the client for appropriate immobilization procedures.
- Utilize nonpharmacological pain control methods such as ice or heat packs, electrical stimulation, or iontophoresis.
Patient-Centered Care
- Neurovascular assessment should be performed hourly for the first 24 hours and then every 1 to 4 hours.
- Assess pain level, location, and frequency using a 0 to 10 pain scale.
- Assess for numbness or tingling, as loss of sensation can indicate nerve damage.
- Check the temperature of the affected extremity, ensuring it's warm to the touch to indicate adequate arterial perfusion. Cool skin suggests decreased arterial perfusion.
- Check Capillary refill by pressing nail beds, with blood return expected within 3 seconds. Prolonged refill suggests decreased arterial perfusion, and cyanotic nail beds indicate venous congestion.
- Ensure pulses are palpable and strong, equal to the unaffected extremity. Doppler ultrasonography may be required if edema makes palpation difficult.
- Ensure the client can actively move the affected extremity.
Nutrition
- Provide a diet high in protein and calcium to facilitate bone healing.
- Encourage iron-rich foods if blood loss occurred.
- Vitamin and mineral supplements promote healing.
Diagnostic procedures
- Standard radiographs, CT scans, or MRI can identify the fracture type and location.
- CT scans are used to detect fractures of the hip and pelvis.
- MRI determines soft tissue damage around the fracture.
- Bone scans using radioactive material determine hairline fractures and complications/delayed healing:
Lab tests
- CBC (complete blood count) detects bleeding (decreased hemoglobin, hematocrit) or infection (increased WBC).
- ESR (erythrocyte sedimentation rate) can be elevated if inflammation is present.
Expected findings
- History of trauma, metabolic bone disorders, chronic conditions, and possible use of corticosteroid therapy are all key findings.
- Pain and reduced movement at or distal to the fracture site are expected.
Physical Assessment Findings
- Examine upper extremities with the client standing or sitting, and lower extremities and pelvis with the client lying down.
- Crepitus is a grating sound from rubbing bone fragments.
- Deformity involves internal or external rotation, shortened extremity, visible bone in open fractures, or asymmetrical limb appearance.
- Muscle spasms are due to pulling forces on misaligned bones.
- Edema (swelling) results from trauma.
- Ecchymosis (bleeding into soft tissues) results from trauma.
- Subcutaneous emphysema, or air bubbles under the skin, is a late finding.
Risk factors
- Risk factors include osteoporosis, falls, motor vehicle crashes, substance use disorder, bone cancer, Paget’s disease, contact sports, hazardous recreational activities, physical abuse, lactose intolerance, malnutrition, and advanced age.
Health promotion
- Ensure adequate calcium intake for the appropriate developmental stage.
- Ensure adequate vitamin D intake and/or sunlight exposure.
- Monitor for osteoporosis, especially in postmenopausal clients and those with thyroid disorders.
- Engage in regular weight-bearing exercises.
- Take bisphosphonates if prescribed to slow bone resorption and treat osteoporosis.
- Use caution to prevent falls or accidents.
- Prevent injury by using seat belts and helmets.
Medications
- Opioid and non-opioid analgesics control pain.
- NSAIDs decrease tissue inflammation, but long-term use can delay bone healing.
- Muscle relaxants relieve muscle spasms.
- Stool softeners prevent constipation.
- Prophylactic antibiotics decrease infection risk in open fractures.
Immobilizing interventions
- Immobilization prevents further injury, promotes healing/circulation, reduces pain, and corrects deformity.
- Types of immobilization devices include braces, casts, splints/immobilizers, traction, external fixation, internal fixation, and orthopedic shoes and boots.
- Closed reduction involves manual traction to realign bone fragments, followed by immobilization for healing.
Splint and immobilizer use
- Splints and immobilizers support, control movement, reduce pain, correct deformity, and prevent additional injury.
- Splints are removable for monitoring skin swelling or integrity and can support injured areas until casting occurs.
- Casting is used for post-paralysis injuries to avoid joint contracture.
- Immobilizers are prefabricated and fasten with hook-and-loop straps.
Traction
- Traction uses pulling force to promote and maintain alignment.
- Traction prescriptions should specify the type of traction, amount of weight, and whether it can be removed for nursing care.
- Goals of traction include preventing soft tissue injury, realigning bone fragments, decreasing muscle spasms and pain, and correcting or preventing deformities.
Types of Traction
- Manual: A pulling force is applied by the hands of the provider for temporary immobilization, usually with sedation or anesthesia, in conjunction with the application of an immobilizing device.
- Straight or running: The counter traction is provided by the client’s body by applying a pulling force in a straight line. Movement of the client’s body can alter the traction provided.
- Skin: Used to decrease muscle spasms and immobilize the extremity prior to surgery, using light (5 to 10 lb) weights. The pulling force is applied by weights attached by rope to the client’s skin with tape, straps, boots, or cuffs. Examples include Bryant’s traction (for congenital hip dislocation in children) and Buck’s traction (preoperatively for hip fractures in adults).
- Balanced suspension produces counter traction using devices like slings or splints to support the fractured extremity off the bed while pulling with ropes and weights.
- Skeletal Uses screws inserted into the bone (such as halo traction), allowing heavier weights (15 to 30 lb) and longer traction time to realign the bone. Frequent pin site care is necessary to prevent infection.
Education
- Report pain not relieved by analgesics or increasing in intensity.
- Report numbness, tingling, or changes in extremity color.
Complications
Compartment syndrome
- Compartment syndrome occurs when pressure within muscle compartments compromises circulation, causing an ischemia-edema cycle.
- Increased edema causes pressure on nerve endings, leading to pain and reduced blood flow, compromising neurovascular status.
- Pressure sources can be external (tight cast) or internal (blood or fluid accumulation).
Manifestations
- Compartment syndrome is assessed using the five P's: pain, paralysis, paresthesia, pallor, and pulselessness.
- Increased pain is unrelieved by elevation or pain medication, with intense pain upon passive movement.
- Paresthesia (numbness, burning, tingling) is an early sign.
- Paralysis, motor weakness, or inability to move the extremity are late signs of nerve damage.
- Pallor affects the tissue, and nail beds become cyanotic.
- Pulselessness is a late sign.
- Palpated muscles are hard and swollen due to edema.
- Untreated tissue necrosis can result. Neuromuscular damage occurs within 4 to 6 hours.
Treatment
- Surgical treatment involves a fasciotomy to relieve pressure and restore circulation.
- The open wounds require sterile packings and dressings until secondary closure, possibly needing skin grafts.
- Negative pressure wound therapy can be used to reduce edema.
Fat embolism
- Adults aged 70 to 80 and assigned male at birth between 20 and 40 years are at increased risk, commonly following hip fractures or within 72 hours after pelvic fracture or surgery.
- Fat globules released into vasculature travel to small blood vessels, especially in the lungs, causing acute respiratory insufficiency and impaired organ perfusion. A cardiac diagnosis should differentiate between fat embolism and pulmonary embolism.
Manifestations
- Early signs include dyspnea, increased respiratory rate, decreased oxygen saturation, headache, decreased mental acuity, respiratory distress, tachycardia, confusion, and chest pain.
- Late signs include cutaneous petechiae (pinpoint-sized subdermal hemorrhages) on the neck, chest, upper arms, and abdomen, a discriminating finding from pulmonary embolism.
Venous thromboembolism
- Deep-vein thrombosis (DVT) and pulmonary embolism are common after trauma.
Osteomyelitis
- Osteomyelitis is a bone infection from infectious organisms following trauma or surgical repair.
Manifestations
- Manifestations include constant, pulsating, localized bone pain worsened by movement; erythema and edema at the infection site; fever (though older adults might not have elevated temperature); leukocytosis; and possible elevated sedimentation rate.
- Many manifestations will disappear when the infection becomes chronic.
Avascular Necrosis
- Avascular necrosis results from circulatory compromise after a fracture.
- Disrupted blood flow leads to ischemia and bone necrosis.
- Commonly found in hip fractures or fractures with bone displacement.
- Risk factors include long-term corticosteroid use, radiation therapy, rheumatoid arthritis, and sickle cell disease.
- Bone graft or prosthetic replacement could be necessary.
Failure of fracture to heal
- Delayed union: A fracture that hasn't healed within 6 months of injury.
- Malunion: Fracture heals incorrectly.
- Nonunion: Fracture never heals.
- Electrical bone stimulation and bone grafting can treat nonunion.
- Low-intensity pulse ultrasound can promote healing.
- Occurs more frequently in older adults.
Hemorrhage
- Due to bones being highly vascular, bleeding is a risk following fracture and can lead to hypovolemic shock.
Complex regional pain syndrome (CRPS)
- Severe chronic pain typically follows musculoskeletal trauma with motor, autonomic nervous system, and sensory changes and can progress to osteoporosis.
Heterotopic ossification
- Growth of bone in soft tissue areas, causing pain and joint stiffness.
- Surgery can be indicated if ROM is significantly decreased.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.