Podcast
Questions and Answers
Which of the following best describes the relationship between tissue interface angle and ultrasound refraction?
Which of the following best describes the relationship between tissue interface angle and ultrasound refraction?
- Refraction effects are consistent regardless of the angle of the ultrasound transducer to the tissue interface.
- Refraction is minimized when the ultrasound transducer is perpendicular to the tissue interface. (correct)
- Refraction is maximized when the ultrasound transducer is perpendicular to the tissue interface.
- Refraction is eliminated when the ultrasound transducer is parallel to the tissue interface.
What is the primary purpose of using a thick liquid (jelly) between the ultrasound transducer and the patient's skin?
What is the primary purpose of using a thick liquid (jelly) between the ultrasound transducer and the patient's skin?
- To reduce the frequency of the ultrasound waves.
- To introduce controlled refraction for enhanced imaging.
- To increase acoustic impedance mismatch for better reflection.
- To eliminate air bubbles and facilitate ultrasound wave passage. (correct)
How does the roughness of a tissue surface affect ultrasound image quality?
How does the roughness of a tissue surface affect ultrasound image quality?
- A rough surface leads to low scattering and a good image.
- A rough surface leads to high scattering and a poor image. (correct)
- A rough surface has no impact on scattering or image quality.
- A rough surface leads to increased penetration and a clearer image.
What is the defining characteristic of A-Mode ultrasound imaging?
What is the defining characteristic of A-Mode ultrasound imaging?
What determines the quality of ultrasound images?
What determines the quality of ultrasound images?
What is the relationship between frequency/resolution and depth of penetration in ultrasound imaging, and how must it be balanced?
What is the relationship between frequency/resolution and depth of penetration in ultrasound imaging, and how must it be balanced?
What causes attenuation of an ultrasound beam as it travels through tissue?
What causes attenuation of an ultrasound beam as it travels through tissue?
What happens when an ultrasound wave encounters a boundary between two tissues with different acoustic impedance (Z) values?
What happens when an ultrasound wave encounters a boundary between two tissues with different acoustic impedance (Z) values?
In A-mode ultrasound, what is the primary relationship utilized to determine the depth of an interface between different tissues?
In A-mode ultrasound, what is the primary relationship utilized to determine the depth of an interface between different tissues?
What is the significance of using high-frequency ultrasound (up to 20 MHz) in ophthalmology with A-mode scans?
What is the significance of using high-frequency ultrasound (up to 20 MHz) in ophthalmology with A-mode scans?
In echoencephalography, which threshold of midline shift detected via A-mode ultrasound would typically indicate an abnormal finding in an adult patient?
In echoencephalography, which threshold of midline shift detected via A-mode ultrasound would typically indicate an abnormal finding in an adult patient?
Which of the following best describes the primary difference in how A-mode and B-mode ultrasound generate images?
Which of the following best describes the primary difference in how A-mode and B-mode ultrasound generate images?
What is the key characteristic that distinguishes M-mode ultrasound from both A-mode and B-mode?
What is the key characteristic that distinguishes M-mode ultrasound from both A-mode and B-mode?
What additional dimension does 4D ultrasound (D-Mode) add compared to traditional 3D ultrasound?
What additional dimension does 4D ultrasound (D-Mode) add compared to traditional 3D ultrasound?
A doctor needs to obtain an image showing the size and structure of a fetal heart as well as its movement. Which ultrasound mode would be most suitable?
A doctor needs to obtain an image showing the size and structure of a fetal heart as well as its movement. Which ultrasound mode would be most suitable?
A cardiologist is assessing the movement of the mitral valve to check for potential prolapse during a routine examination. Which ultrasound mode would be most appropriate for this specific evaluation?
A cardiologist is assessing the movement of the mitral valve to check for potential prolapse during a routine examination. Which ultrasound mode would be most appropriate for this specific evaluation?
In the context of medical imaging, what is the primary difference between A-mode and B-mode ultrasound?
In the context of medical imaging, what is the primary difference between A-mode and B-mode ultrasound?
Which ultrasound imaging mode is most suitable for precisely measuring the thickness of a specific tissue layer?
Which ultrasound imaging mode is most suitable for precisely measuring the thickness of a specific tissue layer?
In M-mode ultrasound, what information is displayed along the x-axis and y-axis respectively?
In M-mode ultrasound, what information is displayed along the x-axis and y-axis respectively?
A cardiologist needs to assess the motion of a heart valve over several cardiac cycles. Which ultrasound mode would be MOST appropriate?
A cardiologist needs to assess the motion of a heart valve over several cardiac cycles. Which ultrasound mode would be MOST appropriate?
What type of information does Doppler mode primarily provide in ultrasound imaging that A-mode, B-mode, and M-mode do not?
What type of information does Doppler mode primarily provide in ultrasound imaging that A-mode, B-mode, and M-mode do not?
You are using ultrasound to assess blood flow in a patient's carotid artery and want to determine if there is any stenosis (narrowing). Which ultrasound mode would be most helpful?
You are using ultrasound to assess blood flow in a patient's carotid artery and want to determine if there is any stenosis (narrowing). Which ultrasound mode would be most helpful?
A physician requires real-time anatomical imaging. What is the accepted term that describes real-time anatomical imaging?
A physician requires real-time anatomical imaging. What is the accepted term that describes real-time anatomical imaging?
Which of the following is an advantage of pulse wave doppler over continuous wave doppler?
Which of the following is an advantage of pulse wave doppler over continuous wave doppler?
Flashcards
A-Mode Ultrasound
A-Mode Ultrasound
Ultrasound waves are sent into the body, and the time for echoes to return from tissue interfaces is measured. Depth is proportional to echo return time.
A-Mode Echo Time
A-Mode Echo Time
Using an average soft tissue velocity of 1540 m/s, an echo returns in 13 µsec at a depth of 1 cm.
Echo Encephalography
Echo Encephalography
Detects brain tumors by sending ultrasound pulses through the skull and comparing echoes from the left and right sides of the head. A shift indicates abnormality.
Abnormal Shift (Echo)
Abnormal Shift (Echo)
Signup and view all the flashcards
Opthalmology A-Scan
Opthalmology A-Scan
Signup and view all the flashcards
B-Mode Ultrasound
B-Mode Ultrasound
Signup and view all the flashcards
M-Mode Ultrasound
M-Mode Ultrasound
Signup and view all the flashcards
D-Mode Ultrasound
D-Mode Ultrasound
Signup and view all the flashcards
Refraction (Ultrasound)
Refraction (Ultrasound)
Signup and view all the flashcards
Focal Zone
Focal Zone
Signup and view all the flashcards
Acoustic Impedance (Z)
Acoustic Impedance (Z)
Signup and view all the flashcards
Ultrasound Backscattering
Ultrasound Backscattering
Signup and view all the flashcards
Attenuation (Ultrasound)
Attenuation (Ultrasound)
Signup and view all the flashcards
Quality of Ultrasound Imaging
Quality of Ultrasound Imaging
Signup and view all the flashcards
Reflection in Ultrasound
Reflection in Ultrasound
Signup and view all the flashcards
A-Mode (1D)
A-Mode (1D)
Signup and view all the flashcards
Sound Wave
Sound Wave
Signup and view all the flashcards
Sound Propagation
Sound Propagation
Signup and view all the flashcards
Frequency (f) Definition
Frequency (f) Definition
Signup and view all the flashcards
Wavelength (λ)
Wavelength (λ)
Signup and view all the flashcards
Sonic Spectrum Divisions
Sonic Spectrum Divisions
Signup and view all the flashcards
Infrasound
Infrasound
Signup and view all the flashcards
Human Hearing Range
Human Hearing Range
Signup and view all the flashcards
Infrasound Effects
Infrasound Effects
Signup and view all the flashcards
Study Notes
Sound in Medicine 2024
- Sound in medicine will be explored
Topics of the Lecture
- Characteristics of sound waves will be discussed
- Reflection and transmission of sound will be discussed
- Intensity level ratio will be examined
- Applications of sound in medicine will be reviewed
- Percussion and Stethoscope as medical tools
- Sonar US generation principles will be explained
- US Generation will be explained
- Production of US images will be explained
- Image quality factors will be examined
- US imaging modes will be outlined
- Physiological effects of US will be covered
General Properties of Sound
- A sound wave is a pattern of disturbance from energy traveling from a sound source (waves transfer energy without transferring matter).
- Sound is a mechanical disturbance propagating through an elastic material medium with a definite velocity.
- In air, sound manifests as local increases (compression) or decreases (rarefaction) of pressure relative to atmospheric pressure.
- Sound is a vibration that propagates through a medium as a mechanical wave, with the medium being solid, liquid, or gas.
- Sound travels fastest in solids, slower in liquids, and slowest in gases.
- Sound speed is determined by: frequency; wavelength.
Frequency
- Frequency of a sound wave is the number of rarefactions and compressions per unit time, denoted as f=1/T
- Wavelength is the distance between successive compressions and rarefactions.
Sonic Spectrum
- The sonic spectrum is classified into three frequency ranges based on wave frequency: infrasound, audible sound, and ultrasound.
- The human ear can hear sounds roughly in the range of 20 Hz to 20 kHz.
- Infrasound refers to sound frequencies below 20Hz, produced by natural phenomena like earthquakes and atmospheric pressure changes.
- Infrasonic effects can travel long distances without losing power due to low absorption and can affect other media.
- Intense infrasonic noise can produce symptoms like respiratory impairment, aural pain, fear, visual hallucinations, and chills.
- Infrasound may also be used in the study of heart mechanical function, revealed by the seismocardiogram. The seismocardiogram measures micro-vibrations produced by heart contraction and blood ejection.
- Ultrasound is the frequency range above 20kHz and used clinically in a number of specialties.
- Ultrasound provides more information than X-rays and is less hazardous for the fetus.
Intensity of a Sound Wave
- The intensity I of a sound wave is the energy carried by the wave per unit area per unit time measured in W/.
Sound Intensity Level
- The absolute value of sound intensity cannot be directly measured, so use reference intensity; (I.)
- Intensity ratio= The intensity of audible sound ranges between Imin = 10-12 (W/m²) [Hearing threshold] and Imax = 1 (W/m²) [Pain threshold].
Sound Characteristics
- The human ear can distinguish two characteristics of sound: loudness and pitch.
- Loudness (volume) is the sensation of sound in the ear, dependent on it's intensity.
- Pitch is whether a sound is high (sharp).
Sound Reflection and Transmission
- When a sound wave is applied perpendicularly to the interface between two media with different acoustic impedance (Z1 and Z2).
- A portion of the wave passes through, while another portion reflects. Large difference in Z results in high reflection.
- The ratio of reflected; Iref (or transmitted; Itran) and the incident waves (Iin) can be measured
Percussion
- Sounds are produced by striking a body surface to detect underlying structures, with three types identified being resonant, hyper-resonant, and dull.
Stethoscope
- Stethoscopes that amplify sounds from the heart, lungs, or other body sites.
- Modern stethoscopes have a bell (closed by a thin diaphragm), tubing, and earpieces.
- The bell serves as an impedance matcher between the body & air, requiring the vibration to resonate in the bell membrane.
- Fres the natural frequency of the bell, depends on the diameter (d) and the tension ( T) of the diaphragm.
- To selectively pick up frequency ranges (like heart murmurs and lung sounds), choose the appropriate bell size and diaphragm tension.
Ultrasound Waves
- Ultrasound is sound with a frequency of 20kHz to 1GHZ.
- Frequencies are above the upper limit of human hearing.
Sonography
- SONAR is a device that uses US waves to generate an image of soft tissue.
- Transducers convert electrical energy to mechanical (ultrasound) energy and vice versa.
- Many types of transducers exist with different frequencies and footprints.
US Generation
- Ultrasound signal is generated and detected by a sensor.
- Transducers are based on peizoelectric principles.
- Many crystals can be used so that AC voltage (electrical energy) across the crystal will produce a vibration of the crystal (mechanical energy) and produce ultrasound.
- In clinical application the piston in the transducer represents the part where an electric potential difference is applied and responds with vibrations. The push-pull action of the transducer causes a compression and rarefaction.
Basic Principle of SONAR
- In medical diagnosis, ultrasound pulses are placed on the body to eliminate presence of air and establish an impedance match.
- Echoes detected as weak signal amplified on oscilloscope.
US Image Production
- Affecting concepts of US image include the below
- Focal zone
- Acoustic impedance
- Refraction
Focal Zone
- For best US image, the object should be at the focal zone (or near field) of the probe.
Acoustic Impedance
- When an ultrasound wave encounters a boundary between two tissues with different values of Z, a fraction the wave energy is backscattered (or reflected) toward the transducer. The boundary is deeper in the body. There is liquid (jelly) between the transducer and the patients skin, this keeps away air bubbles and allows the waves through (small Az).
Refraction
- Refraction is a change in direction of sound wave as it passes to tissue of higher or lower velocity.
Quality of Ultrasound Imaging
- Determined by the interaction of the acoustic wave with the body tissue, interactions include: spatial resolution, attenuation and reflection and transmission.
- Sound is limited by wavelength.
- Attenuation is when an ultrasound beam as it propagates through tissue is summed via absorption and scattering. Characterized by that beams propagation and distance.
Image Quality
- The choice of the ultrasound is a compromise between good resolution, deep penetration, and frequency.
- A higher frequencies have better resolution but high attenuation and low deep penetration.
- Low frequencies have bad solution but low attenuation and deep penetration.
Keynote on Reflection
- Perpendicular reflection originates the echo signal, non-perpendicular reflection causes intensity loss in echo signal.
- On smooth surfaces there is low scattering with rough surfaces there is high scattering.
US Image Modes
- There are multiple types of US image modes
- A-Mode (1D): diagnostic information about the depth of a structure (image with 1-dimension).
- US waves are sent into the body, and uses the time to receive reflected echoes.
- The depth of the interface recorded is proportional to the timing of return.
- The formula is Depth = Velocity x Time
- Sound with a velocity of 1540 m/sec averages soft tissue. The echo takes 13 µsec at a depth of 1 cm. A-modes are used to detect brain tumors and eye diseases.
- Echo encephalography. Ultrasounds are sent into the skull displayed on the oscilloscope. The echoes are compared to ones on the left and right side to find any shifts. 3mm is abnormal.
Opthalmology
- Application of The A scan is used in opthalmology can be divided into two areas: one in concern with obtaining information for eyes. The other is used in biometry.
- Ultrasounds are used from 20MHZ.
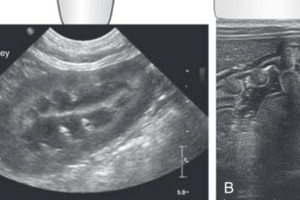
US Image Modes: B-Mode
- The B-Mode 2D obtains two-dimensional images of the body.
- The principle is the same as in the A-mode except transducer is moving, using the storage oscilloscope to produce images.
- The B-mode provides information about the internal structure size location (liver, breast, heart, etc)
US Image Modes: M-Mode
- The M-Mode 2D assesses hearts and heart valves: Combines between features of a and b mode. Traseducer is held stationary compared to a with echoes of different b-modes
- Used in diagnostic information such as mitril valve and pericordia
US Image
- D-mode (3D + motion or 4D) takes 3-dimensionanl US images and adds elements of time to that process.
Physiological Effects of Ultrasound
- Various physiological effects occur when ultrasonic waves pass through the body.
- This magnitude is often dependent on the frequency and amplitude of the sound.
- Examples listed below:
- Low intensity US (~ 0.01 W/cm²) demonstrates no harmful effects and can used in diagnostic work.
- Continuous US (~1 W/cm²) has a deep heating affect towards acoustic and energy tissue.
- Continuous US (1-10 W/cm²) moves sound through compressions, tensions, and pressure zones.
- Continuous US (~ 35 W/cm²) has an effect that destroys tissue that disrupts molecules.
- Continues and focused US (~ 103 W/cm²) specifically destroys deepness with a set up beam.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Related Documents
Description
Explore ultrasound physics: tissue interface angles, refraction, and attenuation. Understand acoustic impedance, image resolution, and A-mode imaging. Learn about high-frequency ultrasound in ophthalmology and optimizing image quality.