Podcast
Questions and Answers
What happens when tissues have the same acoustic impedance?
What happens when tissues have the same acoustic impedance?
- Almost all sound is reflected in an echo.
- Sound waves are scattered.
- Acoustic void or shadow is created.
- No echo is created. (correct)
What two properties of a medium most directly affect the velocity of sound?
What two properties of a medium most directly affect the velocity of sound?
- Viscosity and texture
- Pressure and volume
- Density and stiffness (correct)
- Temperature and color
Assuming a constant ultrasound frequency, how does an increase in the stiffness of a medium affect the resultant wavelength?
Assuming a constant ultrasound frequency, how does an increase in the stiffness of a medium affect the resultant wavelength?
- Wavelength increases. (correct)
- Wavelength fluctuates erratically.
- Wavelength decreases.
- Wavelength remains unchanged.
Which of the following is the dominant component of attenuation of sound in soft tissue?
Which of the following is the dominant component of attenuation of sound in soft tissue?
An ultrasound transducer utilizes which type of crystal to convert electrical energy into sound waves and vice versa?
An ultrasound transducer utilizes which type of crystal to convert electrical energy into sound waves and vice versa?
Spatial compounding enhances image quality by:
Spatial compounding enhances image quality by:
What does a broad spectral tracing in pulsed-wave Doppler typically indicate?
What does a broad spectral tracing in pulsed-wave Doppler typically indicate?
Assuming all other parameters remain constant, what adjustment would most effectively correct aliasing observed on a spectral Doppler display?
Assuming all other parameters remain constant, what adjustment would most effectively correct aliasing observed on a spectral Doppler display?
Which artifact is typically caused by secondary sound beams being emitted in a different direction than the primary beam?
Which artifact is typically caused by secondary sound beams being emitted in a different direction than the primary beam?
A large difference in acoustic impedance of two tissues results in a large amount of ______.
A large difference in acoustic impedance of two tissues results in a large amount of ______.
Which of the following occurs when sound waves encounter small, irregular surfaces?
Which of the following occurs when sound waves encounter small, irregular surfaces?
In typical ultrasound imaging, what percentage of time does the transducer receive sound waves as opposed to emitting them?
In typical ultrasound imaging, what percentage of time does the transducer receive sound waves as opposed to emitting them?
Creating a composite image by combining multiple frames from ultrasound beams that are angled in different directions is called ______________.
Creating a composite image by combining multiple frames from ultrasound beams that are angled in different directions is called ______________.
Which of the following methods can be used to resolve aliasing artifact?
Which of the following methods can be used to resolve aliasing artifact?
Which ultrasound artifact can occur when the Pulse Repetition Frequency (PRF) is too high?
Which ultrasound artifact can occur when the Pulse Repetition Frequency (PRF) is too high?
For pulsed-wave and color Doppler, when the velocity of blood flow exceeds the maximum velocity noted on the scale, the blood flow is recorded on the opposite end of the velocity scale. This artifact is called:
For pulsed-wave and color Doppler, when the velocity of blood flow exceeds the maximum velocity noted on the scale, the blood flow is recorded on the opposite end of the velocity scale. This artifact is called:
Flashcards
Color Doppler
Color Doppler
Indicates blood flow direction relative to the transducer. One color means flow toward, the other away.
Color Doppler Angle Limitation
Color Doppler Angle Limitation
A limitation of color Doppler that occurs when the angle between the sound beam and blood flow is too small reducing or eliminating the doppler shift obtained.
Power Doppler
Power Doppler
Displays the amplitude or power of the Doppler signal, not direction. May be less angle-dependent than color doppler.
Artifact
Artifact
Signup and view all the flashcards
Acoustic Shadowing
Acoustic Shadowing
Signup and view all the flashcards
Diagnostic Ultrasound
Diagnostic Ultrasound
Signup and view all the flashcards
Sound Waves
Sound Waves
Signup and view all the flashcards
Frequency
Frequency
Signup and view all the flashcards
Ultrasound
Ultrasound
Signup and view all the flashcards
Wavelength
Wavelength
Signup and view all the flashcards
Velocity
Velocity
Signup and view all the flashcards
Acoustic Impedance
Acoustic Impedance
Signup and view all the flashcards
Acoustic Impedance Changes
Acoustic Impedance Changes
Signup and view all the flashcards
No Echo
No Echo
Signup and view all the flashcards
Large Impedance Difference
Large Impedance Difference
Signup and view all the flashcards
Soft Tissue/Gas or Bone Interface
Soft Tissue/Gas or Bone Interface
Signup and view all the flashcards
Angle of Incidence
Angle of Incidence
Signup and view all the flashcards
Attenuation
Attenuation
Signup and view all the flashcards
Frequency & Attenuation
Frequency & Attenuation
Signup and view all the flashcards
Absorption (Ultrasound)
Absorption (Ultrasound)
Signup and view all the flashcards
Piezoelectric Crystals
Piezoelectric Crystals
Signup and view all the flashcards
Spatial Compounding
Spatial Compounding
Signup and view all the flashcards
Shadowing Artifact Reduction
Shadowing Artifact Reduction
Signup and view all the flashcards
Brightness Mode (B-mode)
Brightness Mode (B-mode)
Signup and view all the flashcards
Motion Mode (M-mode)
Motion Mode (M-mode)
Signup and view all the flashcards
M-mode Axis Orientation
M-mode Axis Orientation
Signup and view all the flashcards
Gain
Gain
Signup and view all the flashcards
General Gain
General Gain
Signup and view all the flashcards
Time Gain Compensation (TGC)
Time Gain Compensation (TGC)
Signup and view all the flashcards
Ultrasound Frequency vs. Depth
Ultrasound Frequency vs. Depth
Signup and view all the flashcards
B-Mode Ultrasound Imaging
B-Mode Ultrasound Imaging
Signup and view all the flashcards
M-Mode Ultrasound Imaging
M-Mode Ultrasound Imaging
Signup and view all the flashcards
Broadband Ultrasound Technology
Broadband Ultrasound Technology
Signup and view all the flashcards
Benefits of Broadband Frequency
Benefits of Broadband Frequency
Signup and view all the flashcards
Harmonic Frequencies
Harmonic Frequencies
Signup and view all the flashcards
Harmonic Imaging
Harmonic Imaging
Signup and view all the flashcards
Doppler Equation with Angle Correction
Doppler Equation with Angle Correction
Signup and view all the flashcards
Continuous-Wave Doppler
Continuous-Wave Doppler
Signup and view all the flashcards
Doppler Spectral Tracing
Doppler Spectral Tracing
Signup and view all the flashcards
Pulsed-Wave Doppler
Pulsed-Wave Doppler
Signup and view all the flashcards
Pulsed Wave
Pulsed Wave
Signup and view all the flashcards
Homogenous area spectral
Homogenous area spectral
Signup and view all the flashcards
Aliasing
Aliasing
Signup and view all the flashcards
Slice thickness artifact
Slice thickness artifact
Signup and view all the flashcards
Study Notes
- Diagnostic ultrasound (US) is a widely used imaging method, relying on sound waves rather than electromagnetic radiation.
- Understanding US physics clarifies the modality's limitations and potential artifacts.
- This chapter covers basic principles, wave interactions with matter, transducers, Doppler techniques, and artifacts.
Physical Principles of Ultrasound Waves
- Sound transmits energy via alternating regions of low (rarefaction) and high (compression) pressure.
- Sound waves require a medium to travel through, unlike light or radio waves.
- Frequency, wavelength, and velocity describe sound waves.
- Frequency measures wave repetition per second, expressed in hertz (Hz).
- 1 Hz is one cycle per second.
- Ultrasound is sound above 20,000 Hz (0.02 MHz).
- Diagnostic US uses frequencies between 2 MHz and 15 MHz (1 MHz = 1,000,000 Hz).
- Wavelength is the distance a sound wave travels in one cycle, measured in millimeters (mm).
- Wavelength affects image resolution.
- Velocity is the rate sound travels in a medium, based on density and stiffness.
- Sound velocity is highest in solids, lower in liquids, and lowest in gases.
- Average sound velocity in soft tissue is 1.54 mm/µs (1540 m/s).
- US machines rely on this constant velocity for calculations.
- Velocity relates to frequency and wavelength: Velocity (mm/µs) = Frequency (MHz) × Wavelength (mm).
Ultrasound Wave Interaction with Matter
- Acoustic impedance is tissue density multiplied by sound velocity.
- Acoustic impedance differences between tissues affect sound reflection and transmission.
- Echo amplitude for imaging depends on acoustic impedance differences in adjacent tissues.
- No echo forms if tissues share acoustic impedance.
- Large acoustic impedance differences reflect almost all sound.
- Soft tissue/gas and soft tissue/bone interfaces almost totally reflect sound.
- Acoustic coupling gel prevents reflection of all sound waves caused by gas trapped between skin and transducer to allow imaging.
- Incident angle is the angle at which a sound wave encounters a medium.
- Perpendicular incidence (90 degrees) reflects sound back to the transducer, transmits the remaining sound.
- Non-perpendicular incidence reflects sound at an equal angle, but away from the transducer.
- Amount of reflection and transmission depends on acoustic impedance differences.
- Attenuation weakens an ultrasound beam as it travels, based and frequency.
- High-frequency sound waves attenuate more.
- Attenuation involves absorption, reflection, and scattering.
- Absorption converts sound wave energy to heat, but causes insignificant temperature change in soft tissue.
- Reflection contributes to attenuation as the sound wave encounters tissue interfaces.
- Only reflections returning to the transducer form images.
- Scattering, frequency-independent, occurs at small, irregular surfaces within organ parenchyma, creating echotexture.
Transducers
- Transducers contain piezoelectric crystals, converting electric current into sound waves and vice versa.
- Applying electric charge to a piezoelectric crystal causes deformation and sound wave creation.
- Sound waves applied to piezoelectric crystals generate an electric signal.
- Transducer emits sound less than 1% of the time, receives sound over 99% of the time.
- Pulse repetition frequency (PRF) is the number of send/receive cycles per second.
- Spatial pulse length (SPL) measures the length of a single ultrasound pulse.
- Shorter SPL improves axial resolution.
- Transducer selection is based on properties and the region being imaged.
- Electronic (array) transducers consist of multiple small elements.
- Elements are arranged linearly, curved or in rings.
- The elements are electronically fired to shape field of view and focus sound beams.
- Sector transducers create pie-shaped images, used intercostally for thoracic imaging.
- Linear transducers create rectangular images, used according to target anatomy and patient size.
- Footprint is the contact area between the transducer and the patient.
- Linear transducers have larger footprints.
- Resolution describes the ability to distinguish echoes based on space, time, and strength.
- Axial resolution distinguishes reflectors along the beam, equals half the SPL.
- Higher frequency transducers improve axial resolution via shorter SPL.
- Lateral resolution distinguishes reflectors perpendicular to the beam, based on beam width.
- Narrower beams improve lateral resolution.
- Lateral resolution is optimal at the beam's focal point.
- Penetration depth is inversely related to frequency.
- Higher frequencies are best for superficial structures.
- Lower frequencies are best for deeper structures.
- Scanning typically begins with higher frequencies for better resolution.
New Technologies in Ultrasound
- Newer ultrasound improves image quality.
- It is important to understand basics and adjustments to improve lesion conspicuity.
- Broad bandwidth allows transducers to emit range of frequencies.
- It allows selection of various frequencies from one transducer.
- Modern broadband transducers improve near-field and far-field resolution, and axial resolution.
- Harmonic imaging improves normal organ and lesion conspicuity.
- Harmonics are multiples of transmitted pulse frequency ie; 4 MHz (F), then the second harmonic is 8 MHz (2F).
- Tissue interactions generate weak harmonic echoes.
- The returning echoes are filtered, improving image quality.
- The primary beam is narrower, improving lateral resolution.
- Artifacts are reduced as extra beams lack the strength to generate harmonics.
- Harmonic beam originates beyond artifactual problems, reducing image degradation and noise.
- Spatial compounding combines frames from different angles.
- Sound waves are steered without moving the transducer.
- Multiple angles increase sound wave encountering a reflector close to 90 degrees.
- Frames are combined into a compound image thought to improve contrast resolution, border definition, and signal-to-noise ratio.
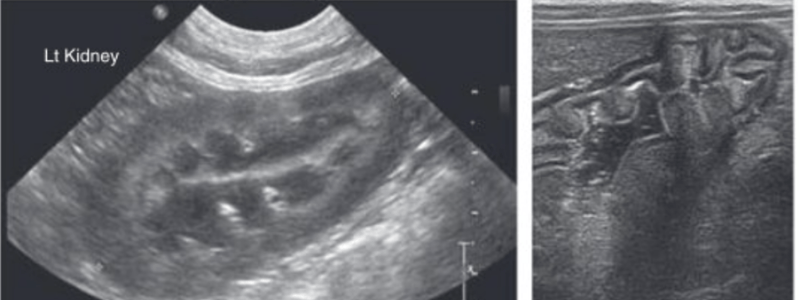
- Spatial compounding reduces shadowing, and is used to find renal calculi.
Display
- Image formation is based on the pulse echo principle where electrical signals from returning echoes are amplified into final image.
- A timer measures how long echoes take and determines distance.
- Constant velocity of sound is required for above.
- Brightness mode (B-mode or grayscale) and motion mode (M-mode) are 2 echo display modes commonly used in ultrasonography.
- B-mode is typically used for cardiac and abdominal imaging.
- M-mode is used for echocardiography.
- B-mode images are formed of dots with varying brightness.
- The dots relate to the returning echos.
- Brightness and grayscale depends on the strength of echos.
- Structures returning the echos determine position.
- Multiple thin scan lines made up a complete image and look similar to a slice of tissue.
- M-mode records thin selection of ultrasound image over time.
- It is selected using B-mode image and shown as a line on the screen.
- M-mode cursor is placed in desired location.
- On M-mode image depth of image shown on the vertical axis and time is displayed on the horizontal axis.
- Brightness of dots is proportional to strength of Returning echos, similar to B-mode.
- When holding transducer stationary, examiner can evaluate structure movements over time.
- M-mode is most common for echocardiography to measure function of ventricles and heart valves.
- In B-mode imaging displayed organs vary with the orientation of the structure being imaged and position of the transducer.
- Point transducer cranial with left of the screen representing cranial in both sagittal and longitudinal orientation and towards the right side of the patient is a transverse one.
- Right side of the screen is cranial when conducting cardiac imaging
- Near field is portion of image closest to the transducer (top of screen) and opposite is far field.
Basic Scanner Controls
- Gain impacts amplification of returning echos within the receiver.
- General gain and time gain compensation are two types of adjustable gain:
- General gain: can increase brightness, needs adjustment at start of each scan where brightness is increased or decreased.
- Subtle parenchymal detail is lost at too low gain and at too high the contrast resolution is lost because of bright image.
- Time gain compensation - TGC- helps to amplify echos better due to sound waves losing intensity as they move through tissue.
- TGC controls allow user to adjust gain in selected regions/depths of the image.
- Ultrasound machine typically has slider bars that control gain to echos from varying depths.
- Top slider controls pain for structures and near field and bottomsliders are for for field.
- Frequency: penetration depth and image resolution.
- Higher frequencies are best to increase axial resolution of the image.
- Linear transducer with higher frequency should be used for superficial structures.
Principles of Interpretation
- Reflects the relation of one structures relative brightness.
- Anechoic structres are echoes that appear black when the echogenicity compared darker structures are hypoechoic and brighter is hyperechoic.
- If the image has the same degree of brightness they are isoechoic.
- Detectable diffuse changes in whole organ is difficult as accurate detection is related to the sonographer.
- Machine settings and transduce selection can alter the echogenicity of the organ.
- Organ echogenicity may be determine by the internal auto referencing or multiple abdominal organs.
- Focal changes are easier to see as adjacent parenchyma is contrasted.
Doppler Techniques
- Asseses the blood flow direction as well as velocity.
Doppler Principle
- As the sound approaches the listener or moves away the change in sounds change the pitch and frequency.
- Medical sonography has applied this to allow imaging of bloodflow and velocity.
- The affect is named after Johann Christian Andreas Doppler a mathematician around 1842 to propsed the effect.
- The frequency difference between incident sound waves and the relfected sounds is described by fo = (2x fox URBC)/C.
- fp is frequency of doppler shift, fo is orginal frequency, URBC is bloodcells elocity whereas c os speed sonds.
- US machines have to emit sounds the Doppler shift recorded using frequency should be audible.
- Realistically the sounds need to be parallel to the direction of blood flow.
- Doppler angle need to consider the angle betwene blood-flow and sound wave direction.
- Doppler underestimate is the Doppler shift that account for this angle is important.
- URBC (fDxC)/(2x fox cos 0)
- Where frequency of Doppler shift is FD speed tissue is C, cosine is cos and doppler angle is @.
- Doppler cannot be measured when the Dopple angle is 90 and should be less than 60 for accuracy and angles between 30 and 60 are considered easisest.
Doppler Modes
The following modes are considered: a wave is continuous, pulse, color and power.
- Continuous uses 2 separate crystals in transducer where waves come from 1 and are received on the other because of the higher sampling accuarcy and rate.
- Accuracy is great to measureDoppler shift much higher velocities recorded.
- There are limitation as crystal omits sound and cannot receive because of ehco receiving task and the differentiation of the measured bloodflow occurs along path of the insonated sounpath.
- Pulse wave is typically done using Crystal where waves echos pulse and the used in combine Bmode known duplex Doppler where electonic region, vessel is selected by the ultrasound as needed.
- Spectral tracing is product both ways.
- The tracking records the direction of velocity of blood flow with the baseline where recording above denotes towards transducer and vice vera.
- Is Homogenous the spectral is thin and area inside the curve is non
- Turbulence caused by width of the spectral tracing can be attributed when large of velocity is inside can be caused when transudcer proximity.
Doppler artifacts
- Most common artecfact when PRF is too low where part wrap on spectral trading of dople signal the sample must be 2 times hightest from the blood flow
- Ways to solve increasing sampling PRF rate which will not create aliasing, decreasing gates
Artifacts
- Are the ultrasound imaging not undiserable and not always provide regarding composition.
Types of Artifacts
Assumption
Sound must travel ina straight like Comes objects location beam axis, Echoes return to tranducer and reflection Speed of sound need to contstant in tissue Amplitude relates to scattering types.
- Acoustic shadowing is echogenicity like bones or calculi.
- Primary sound mostly related in the given situation mostly the reflected or absroded.
- Returning inssiffent amounnt or returns makes look black shadow useful indicator shadowing minimized in spacing improves composition analysis
- Enhancement Areas of increase is for structure that attenuated usually the fluids. The sounds need to travel with low intensity causing strong adjacent tissue
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.