Podcast
Questions and Answers
Which tissue type is primarily responsible for detecting changes and generating electrical signals?
Which tissue type is primarily responsible for detecting changes and generating electrical signals?
- Nervous tissue (correct)
- Epithelial tissue
- Muscular tissue
- Connective tissue
Which type of tissue is characterized by cells specialized for contraction?
Which type of tissue is characterized by cells specialized for contraction?
- Nervous tissue
- Epithelial tissue
- Muscular tissue (correct)
- Connective tissue
Which tissue type is responsible for binding organs together and storing energy reserves as fat?
Which tissue type is responsible for binding organs together and storing energy reserves as fat?
- Nervous tissue
- Muscular tissue
- Connective tissue (correct)
- Epithelial tissue
A pathologist is examining a tissue sample and notes significant changes that indicate disease. Which of the following is the MOST likely role of this pathologist?
A pathologist is examining a tissue sample and notes significant changes that indicate disease. Which of the following is the MOST likely role of this pathologist?
Which cell junction type inhibits the passage of substances between cells, preventing leakage?
Which cell junction type inhibits the passage of substances between cells, preventing leakage?
Which type of cell junction allows for communication between adjacent cells through connexons?
Which type of cell junction allows for communication between adjacent cells through connexons?
In tissues subjected to tension and stretching, such as the epidermis, which cell junction is MOST important?
In tissues subjected to tension and stretching, such as the epidermis, which cell junction is MOST important?
Which of the following BEST describes the role of cadherins in cell junctions?
Which of the following BEST describes the role of cadherins in cell junctions?
How do hemidesmosomes differ functionally from desmosomes?
How do hemidesmosomes differ functionally from desmosomes?
What is the primary structural difference between epithelial and connective tissues regarding the extracellular matrix?
What is the primary structural difference between epithelial and connective tissues regarding the extracellular matrix?
What functional challenge arises from the fact that epithelial tissue is avascular?
What functional challenge arises from the fact that epithelial tissue is avascular?
What is the role of the reticular lamina in the basement membrane?
What is the role of the reticular lamina in the basement membrane?
How does the basement membrane support epithelial tissue during wound healing?
How does the basement membrane support epithelial tissue during wound healing?
What characteristic distinguishes pseudostratified epithelium from simple epithelium?
What characteristic distinguishes pseudostratified epithelium from simple epithelium?
Where is nonkeratinized stratified squamous epithelium typically found?
Where is nonkeratinized stratified squamous epithelium typically found?
What BEST describes the function of transitional epithelium (urothelium)?
What BEST describes the function of transitional epithelium (urothelium)?
How do endocrine glands differ structurally from exocrine glands?
How do endocrine glands differ structurally from exocrine glands?
How do multicellular exocrine glands with branched ducts differ from those with unbranched ducts?
How do multicellular exocrine glands with branched ducts differ from those with unbranched ducts?
What is the key difference between holocrine and merocrine glands in terms of secretion?
What is the key difference between holocrine and merocrine glands in terms of secretion?
What role do mesenchymal cells play in connective tissue?
What role do mesenchymal cells play in connective tissue?
What is the primary function of fibroblasts in connective tissue?
What is the primary function of fibroblasts in connective tissue?
What property of glycosaminoglycans (GAGs) contributes to the turgidity of ground substance?
What property of glycosaminoglycans (GAGs) contributes to the turgidity of ground substance?
What is the main function of collagen fibers in connective tissue?
What is the main function of collagen fibers in connective tissue?
How do elastic fibers contribute to the function of lung tissue?
How do elastic fibers contribute to the function of lung tissue?
What is the role of reticular fibers in the spleen and lymph nodes?
What is the role of reticular fibers in the spleen and lymph nodes?
How does dense regular connective tissue differ structurally from dense irregular connective tissue?
How does dense regular connective tissue differ structurally from dense irregular connective tissue?
What is the primary role of chondroitin sulfate in cartilage?
What is the primary role of chondroitin sulfate in cartilage?
How does cartilage receive nutrients, given that it is avascular?
How does cartilage receive nutrients, given that it is avascular?
How does interstitial growth occur in cartilage?
How does interstitial growth occur in cartilage?
What is the role of bone lamellae in compact bone?
What is the role of bone lamellae in compact bone?
What is the function of osteonic canals in bone tissue?
What is the function of osteonic canals in bone tissue?
What is the primary function of red blood cells?
What is the primary function of red blood cells?
What type of membrane lines a body cavity that opens directly to the exterior?
What type of membrane lines a body cavity that opens directly to the exterior?
Which type of membrane covers organs within a body cavity and is NOT open to the exterior?
Which type of membrane covers organs within a body cavity and is NOT open to the exterior?
What is the function of serous fluid secreted by serous membranes?
What is the function of serous fluid secreted by serous membranes?
What are the main tissue types composing the cutaneous membrane?
What are the main tissue types composing the cutaneous membrane?
What is a key characteristic of synovial membranes that distinguishes them from other types of membranes?
What is a key characteristic of synovial membranes that distinguishes them from other types of membranes?
Flashcards
What is a tissue?
What is a tissue?
A group of cells with a common origin and specialized function.
What is epithelial tissue?
What is epithelial tissue?
Covers body surfaces, lines organs/cavities, and forms glands.
What is connective tissue?
What is connective tissue?
Protects, supports, and binds organs together; provides immunity.
What is muscular tissue?
What is muscular tissue?
Signup and view all the flashcards
What is nervous tissue?
What is nervous tissue?
Signup and view all the flashcards
What are Cell Junctions?
What are Cell Junctions?
Signup and view all the flashcards
What are Tight Junctions?
What are Tight Junctions?
Signup and view all the flashcards
What are Adhering Junctions?
What are Adhering Junctions?
Signup and view all the flashcards
What are Desmosomes?
What are Desmosomes?
Signup and view all the flashcards
What are Hemidesmosomes?
What are Hemidesmosomes?
Signup and view all the flashcards
What are Gap Junctions?
What are Gap Junctions?
Signup and view all the flashcards
What is Epithelial Tissue?
What is Epithelial Tissue?
Signup and view all the flashcards
What is Connective Tissue?
What is Connective Tissue?
Signup and view all the flashcards
What are the two types of Epithelial Tissue?
What are the two types of Epithelial Tissue?
Signup and view all the flashcards
What is the Apical Surface?
What is the Apical Surface?
Signup and view all the flashcards
What is the Lateral Surface?
What is the Lateral Surface?
Signup and view all the flashcards
What is the Basal Surface?
What is the Basal Surface?
Signup and view all the flashcards
What is the Basement Membrane?
What is the Basement Membrane?
Signup and view all the flashcards
What is Simple Epithelium?
What is Simple Epithelium?
Signup and view all the flashcards
What is Pseudostratified Epithelium?
What is Pseudostratified Epithelium?
Signup and view all the flashcards
What is Stratified Epithelium?
What is Stratified Epithelium?
Signup and view all the flashcards
What are Squamous Cells?
What are Squamous Cells?
Signup and view all the flashcards
What are Cuboidal Cells?
What are Cuboidal Cells?
Signup and view all the flashcards
What are Columnar Cells?
What are Columnar Cells?
Signup and view all the flashcards
What are Transitional Cells?
What are Transitional Cells?
Signup and view all the flashcards
What is Endothelium?
What is Endothelium?
Signup and view all the flashcards
What is Mesothelium?
What is Mesothelium?
Signup and view all the flashcards
What is Keratinized Stratified Squamous Epithelium?
What is Keratinized Stratified Squamous Epithelium?
Signup and view all the flashcards
What is Nonkeratinized Stratified Squamous Epithelium?
What is Nonkeratinized Stratified Squamous Epithelium?
Signup and view all the flashcards
What are Endocrine Glands?
What are Endocrine Glands?
Signup and view all the flashcards
What are Exocrine Glands?
What are Exocrine Glands?
Signup and view all the flashcards
What are Unicellular Glands?
What are Unicellular Glands?
Signup and view all the flashcards
What are Multicellular Glands?
What are Multicellular Glands?
Signup and view all the flashcards
What are Simple Glands?
What are Simple Glands?
Signup and view all the flashcards
What are Compound Glands?
What are Compound Glands?
Signup and view all the flashcards
What are Merocrine Glands?
What are Merocrine Glands?
Signup and view all the flashcards
What are Apocrine Glands?
What are Apocrine Glands?
Signup and view all the flashcards
What are Holocrine Glands?
What are Holocrine Glands?
Signup and view all the flashcards
What are the functions of Connective Tissue?
What are the functions of Connective Tissue?
Signup and view all the flashcards
What is Extracellular Matrix?
What is Extracellular Matrix?
Signup and view all the flashcards
Study Notes
- Cells rarely function in isolation but as part of tissues.
- Tissues are influenced by extracellular material and connections between cells.
- Tissue consistency varies from hard to semisolid to liquid, as seen in bone, fat, and blood.
- Tissues differ in cell types, cell arrangement, and extracellular material.
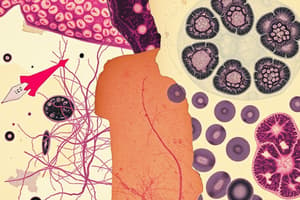
Types of Tissues
- A tissue is a group of cells with a common origin that work together for specialized activities.
- Histology is the study of tissues.
- A pathologist examines tissues for disease indicators.
- Body tissues are classified into four basic types based on structure and function.
- Epithelial tissue covers body surfaces, lines organs/cavities/ducts, and forms glands, enabling interaction with internal and external environments.
- Connective tissue protects, supports, binds organs, stores energy, and provides immunity.
- Muscular tissue is specialized for contraction, generating force and heat.
- Nervous tissue detects internal and external changes, responding with electrical signals (nerve impulses) for muscle contraction and glandular secretions.
- Epithelial tissue and most connective tissue types are widely distributed and have diverse structures and functions.
- Bone tissue and blood general features are introduced, with detailed discussion later.
- Muscular tissue and nervous tissue structure and function are introduced, with detailed discussion later.
- Tissue types differ in cell shape, structure, function, and distribution.
- Most cells remain anchored within a tissue, while some (e.g., phagocytes) move freely.
- Extensive cell migration occurs during growth and development before birth.
Biopsy
- Biopsy involves removing living tissue samples for microscopic examination.
- Used to diagnose disorders like cancer and unexplained infections/inflammations.
- Tissue samples are preserved, stained, and sectioned for observation.
- Biopsies can determine the appropriate treatment during surgery.
Cell Junctions
- Cell junctions are contact points between plasma membranes of tissue cells.
- Epithelial, muscle, and nerve cells are tightly joined into functional units.
- Five main types of cell junctions: tight junctions, adhering junctions, desmosomes, hemidesmosomes, and gap junctions.
Tight Junctions
- Tight junctions have transmembrane protein strands that fuse plasma membranes to seal off passageways between cells.
- Found in stomach, intestines, and urinary bladder epithelial tissue.
- Prevents substance passage between cells and leakage of organ contents.
Adhering Junctions
- Adhering junctions contain plaque, a protein layer attaching to membrane proteins and cytoskeleton microfilaments.
- Cadherins are transmembrane glycoproteins joining cells, inserting into plaque and connecting to adjacent cell cadherins.
- In epithelial cells, adhering junctions form adhesion belts that encircle cells.
- Helps epithelial surfaces resist separation during contractile activities.
Desmosomes
- Desmosomes contain plaque and cadherins that attach cells.
- Desmosome plaque attaches to intermediate filaments made of keratin, not microfilaments.
- Intermediate filaments extend from desmosomes across the cytosol.
- Provides stability to cells and tissues (spot-weld like).
- Common in epidermis and cardiac muscle, preventing separation under tension.
Hemidesmosomes
- Hemidesmosomes resemble half of a desmosome and do not link adjacent cells.
- Integrins are transmembrane glycoproteins that attach to intermediate filaments made of keratin inside the cell.
- Integrins attach to laminin in the basement membrane outside the cell.
- Anchors cells to the basement membrane.
Gap Junctions
- Gap junctions have connexin proteins that form fluid-filled tunnels (connexons) connecting cells.
- Plasma membranes are separated by a narrow intercellular gap.
- Ions and small molecules diffuse through connexons, but large molecules are prevented from passing.
- Nutrient and waste transfer occurs in avascular tissues like the lens and cornea.
- Allows cell communication and rapid spread of nerve or muscle impulses.
Epithelial vs. Connective Tissues
- Epithelial tissue has tightly packed cells with little extracellular matrix, while connective tissue has abundant extracellular material separating cells.
- Epithelial tissue lacks blood vessels; connective tissue has networks of blood vessels.
- Epithelial tissue forms surface layers without another tissue covering it, except in blood vessel linings.
- Epithelial tissue is adjacent to blood vessel-rich connective tissue for oxygen, nutrient, and waste exchange.
Epithelial Tissue
- Epithelial tissue consists of cells in continuous sheets, single or multiple layers.
- Cells are closely packed with minimal intercellular space.
- Types: surface epithelium (outer covering/inner lining) and glandular epithelium (secreting portion of glands).
- Functions: protection, secretion, absorption, and excretion.
Epithelial Cell Surfaces
- Apical surface faces the body surface, cavity, lumen, or duct and may contain cilia or microvilli.
- Lateral surfaces face adjacent cells and contain cell junctions.
- Basal surface adheres to extracellular materials like the basement membrane, anchoring the epithelium.
- Apical layer is the most superficial in multiple layers, and the basal layer is the deepest.
Basement Membrane
- Basement membrane is a thin extracellular layer with two layers: basal lamina and reticular lamina.
- Basal lamina is secreted by epithelial cells and contains proteins, glycoproteins, and proteoglycans.
- Laminin molecules attach epithelial cells to the basement membrane.
- Reticular lamina is closer to connective tissue and contains collagen produced by fibroblasts.
- Functions: anchors epithelium, facilitates cell migration during growth/healing, restricts molecule passage, and participates in blood filtration in kidneys.
- Epithelial tissue has a nerve supply but is avascular, relying on adjacent connective tissue for nutrient/waste exchange via diffusion.
- High cell division rate enables constant renewal and repair of the tissue.
- Roles: protection, filtration, secretion, absorption, and excretion with nervous tissue for special sensory organs.
Cell Layer Arrangements
- Simple epithelium is a single layer for diffusion, osmosis, filtration, secretion, or absorption.
- Secretion is the production and release of substances like mucus, sweat, or enzymes.
- Absorption is the intake of fluids or other substances.
- Pseudostratified epithelium appears multi-layered but is simple, with nuclei at different levels.
- Some cells have cilia; others (goblet cells) secrete mucus.
- Stratified epithelium has multiple layers for protection in areas of wear and tear.
Cell Shapes
- Squamous cells are thin, allowing rapid substance passage.
- Cuboidal cells are cube-shaped, functioning in secretion or absorption, sometimes with microvilli.
- Columnar cells are tall, protecting underlying tissues, often specialized for secretion and absorption, and may have cilia or microvilli.
- Transitional cells change shape, (squamous to cuboidal and back), as organs stretch/collapse.
Types of Epithelial Tissues
- Simple epithelium
- Simple squamous epithelium
- Endothelium lines heart, blood vessels, lymphatic vessels.
- Mesothelium forms the serous membrane epithelial layer.
- Simple cuboidal epithelium
- Simple columnar epithelium
- Nonciliated (lacks cilia)
- Ciliated (contains cilia)
- Pseudostratified columnar epithelium
- Nonciliated (lacks cilia)
- Ciliated (contains cilia)
- Stratified epithelium
- Stratified squamous epithelium
- Nonkeratinized (lacks keratin) Keratinized (contains keratin)
- Stratified cuboidal epithelium
- Stratified columnar epithelium
- Urothelium or transitional epithelium (lines most of the urinary tract)
- Stratified classification is based on the shape of the cells at the apical surface.
Surface Epithelium
- Forms outer covering of skin and some internal organs.
- Forms inner lining of blood vessels, ducts, body cavities, and interiors of respiratory, digestive, urinary, and reproductive systems.
- Simple squamous epithelium single layer of flat cells; lines the cardiovascular and lymphatic systems (endothelium) and forms the serous membranes (mesothelium); filtration and diffusion processes.
- Simple cuboidal epithelium single layer of cube-shaped cells; covers the surface of the ovary; secretion and absorption.
- Nonciliated simple columnar epithelium single layer of nonciliated column-like cells with oval nuclei near the base; lines digestive canal, ducts of glands, and gallbladder; secretion and absorption.
- Ciliated simple columnar epithelium single layer of ciliated column-like cells with oval nuclei near the base, interspersed goblet cells; lines some bronchioles of respiratory tract, uterine tubes, uterus, some paranasal sinuses, central canal of spinal cord, and ventricles of the brain; moves mucus and foreign particles toward the throat.
- Nonciliated pseudostratified columnar epithelium appears to have several layers of cells because the nuclei of the cells are located at different levels. contains cells without cilia and also lacks globlet cells, lines epididymis, larger ducts of many glands, and parts of male urethra; absorption and secretion.
- Ciliated pseudostratified columnar epithelium appears to have several layers because cell nuclei are at various levels. contains cells that extend to surface and secrete mucus (globlet cells) or bear cilia. lines airways of most of upper respiratory tract; secretes mucus that traps foreign particles, and cilia sweep away mucus for elimination from the body.
- Stratified squamous epithelium has two or more layers of cells; surface layer and underlying cells are squamous; located on the superficial layer of skin & mouth lining; Protection against abrasion, water loss, ultraviolet radiation, and foreign invasion
- Stratified cuboidal epithelium has two or more layers of cells; the cells in the surface layer are cube-shaped. located on the ducts of adult sweat glands and esophageal glands, part of male urethra; protection; limited secretion and absorption.
- Stratified columnar epithelium has irregular basal layers; only the apical layer has columnar cells. located on part of urethra, large excretory ducts of glands; protection and secretion
- Urothelium (Transitional Epithelium) Has a variable appearance unique to the urinary system, located on the lines urinary organs; allows organs to stretch while holding fluid.
Papanicolaou Test
- A Pap test involves a collection of epithelial cells from a tissue being scraped and examined.
- Used to detect early changes in cells indicating a precancerous condition in the female reproductive system.
- Pap tests recommended every three years starting at the age of 21 and females aged 30 to 65 should have Pap testing and HPV every five years or a Pap test alone every three years.
Glandular Epithelium
- Function is secretion accomplished by glandular cells.
Endocrine Glands
- Endocrine (ductless) glands secrete hormones into interstitial fluid, diffusing into bloodstream. Examples: pituitary, pineal, thyroid, adrenal glands, pancreas, ovaries, testes.
- Hormones regulate metabolic/physiological activities.
Exocrine Glands
- Exocrine glands secrete products into ducts emptying onto surfaces or linings.
- Examples: sweat, oil, earwax, salivary glands, and pancreas.
- Produces substances such as sweat to help lower body temperature, oil, saliva, and digestive enzymes.
Structural Classification of Exocrine Glands
- Can be unicellular (single-celled) or multicellular.
- Unicellular glands (e.g., goblet cells) secrete mucus directly onto the apical surface of lining epithelium.
- Multicellular glands have many cells with distinctive structures (e.g., sweat, oil, and salivary glands).
- Multicellular glands are categorized by duct branching (simple or compound) and secretory portion shape (tubular, acinar, or tubuloacinar).
- Simple unbranched duct, compound - branched duct
- Tubular - glands with tubular secretory parts, Acinar (alveolar) glands - those with rounded secretory portions & Tubuloacinar – both tubular and rounded
Structural classification scheme
- Simple Tubular: tubular, straight secretory part attaches to single unbranched duct.
- Simple Branched Tubular: branched tubular secretory part attaches to a single unbranched duct.
- Simple Coiled Tubular: coiled tubular secretory part attaches to a single unbranched duct.
- Simple Acinar: a rounded secretory portion that attaches to a single unbranched duct.
- Simple Branched Acinar: rounded, branched secretory part attaches to a single unbranched duct.
- Compound Tubular: tubular secretory portion that attaches to a branched duct.
- Compound Acinar: a rounded secretory portion that attaches to a branched duct.
- Compound Tubuloacinar: The secretory portion has both tubular and rounded and attaches to a branched duct.
Functional Classification of Exocrine Glands
- Classified by secretion release.
- All begin w/ endoplasmic reticulum & Golgi forming intracellular secretory vesicles.
- Merocrine glands secrete products is released from the cell in secretory vesicles via exocytosis, like salivary glands and pancreas.
- Apocrine glands accumulate secretions at the apical surface, which pinches off, like mammary glands.
- Holocrine glands accumulate secretions in cytosol until cell ruptures, like sebaceous glands.
Connective Tissue
- Abundant throughout the body.
- Functions: binding/supporting tissues, protecting/insulating organs, transporting substances (blood), storing energy (fat), and providing immune responses.
General Features of Connective Tissue
- Consists of extracellular matrix and cells.
- Extracellular matrix is material between cells, made of protein fibers and ground substance.
- Structure determines tissue qualities.
- Unlike epithelial tissue, connective tissue doesn't occur on body surfaces, is highly vascular, and is supplied with nerves.
Connective Tissue Cells
- Mesenchymal cells give rise to connective tissue cells.
- Immature cells end in -blast (e.g., fibroblasts, chondroblasts, osteoblasts); retain division capacity and secrete the extracellular matrix.
- Mature cells end in -cyte (e.g., fibrocytes, chondrocytes, osteocytes); have reduced division capacity and maintain the extracellular matrix.
- Macrophages are eaters, Mast cells = inflammatory, Adipocytes = Fat, Leukocytes = white blood cells fight disease.
Connective Tissue Extracellular Matrix
- Unique properties based on extracellular materials between the cells.
- Composed of ground substance and fibers.
Ground Substance
- Ground substance is a component of a connective tissue between the cells and fibers.
- Supports cells, binds them, stores water, and provides a medium for substance exchange between blood and cells.
- It contains water and large organic molecules, many of which are complex combinations of polysaccharides and proteins, which includes hyaluronic acid
- Is viscous, slippery binds cells together, lubricates joints, maintains shape
- Contains adhesion proteins like fibronectin, which links components of ground substance and attaches cells.
Fibers
- Three types embedded in the extracellular matrix: collagen, elastic, and reticular fibers.
- Function to strengthen and support connective tissues
- Collagen fibers: Very strong and resist stretching
- Elastic fibers: strong but can be stretched up to 150%
- Reticular fibers: Provides support in the walls of blood vessels form a network around cells in some tissues
Sprain
- Stretched or torn ligaments.
- Ankle joint is most frequently sprained.
- Poor blood supply results in slow healing or surgical repair.
Areolar
- Small space
Classification of Connective Tissue
- Classified as embryonic (present in embryo/fetus) or mature (present after birth).
- Embryonic CT types: mesenchyme and mucoid connective tissue.
- Mature CT categorized as connective tissue proper (flexible, viscous ground substance), supporting connective tissue (protects and supports), and liquid connective tissue (liquid extracellular matrix).
Embryonic Connective Tissue
- Mesenchyme has irregularly shaped mesenchymal cells embedded in semifluid ground substance with reticular fibers; forms other connective tissues.
- Mucoid connective tissue has scattered fibroblasts in viscous ground substance with collagen fibers; supports the umbilical cord.
Mature Connective Tissue
- Includes connective tissue proper, supporting connective tissue, and liquid connective tissue.
Connective Tissue Proper
- Flexible with a viscous ground substance with abundant fibers.
Loose Connective Tissue
- Fibers are loosely arranged between cells.
- Includes areolar, adipose, and reticular connective tissues.
- Areolar connective tissue is most widely distributed; arranged randomly and several kinds of cells embedded in gel-like ground substance; strength, elasticity and support
- Adipose Tissue (fat) cells; specialized for storage of triglycerides in large droplet; reduces heat loss through skin
- Reticular Connective: Intricate intertwining network of reticular fibers and reticular; Forms tissues of organs binds muscle filters
Liposuction
- A type of body-contouring technique to remove fat and sculpt the body.
- Suctioning fat from specific areas of the body utilizing a cannula, which removes the fat with the assistance of a powerful vacuum-pressure.
Dense Connective Tissue
- More fibers, thicker, and densely packed, but have considerably fewer cells.
- Types: dense regular, dense irregular, and elastic connective tissues.
- Dense regular CT: shiny white matrix with collagen fibers regularly arranged in bundles with fibroblasts in rows between them; provides strong attachment between structures and withstands tension.
- Dense irregular CT: collagen fibers irregularly arranged with few fibroblasts; fasciae (tissue beneath the skin) and provides tensile (pulling) strength in many directions.
- Elastic tissues predominantly elastic fibers with fibroblasts between them; walls of elastic arteries and trachea,is strong can recoil to original shape
Supporting Connective Tissue
- Includes cartilage and bone.
Cartilage
- Has network of collagen or elastic fibers embedded in chondroitin sulfate.
- Endures more strain
- Is avascular
- Chondrocytes in cartilage lacunae.
- Is metabolically inactive
- Types: hyaline, fibrous, and elastic cartilage.
- Perichondrium surrounds cartilage, contains blood vessels, nerves, and is the source of new cartilage cells.
- Antiangiogenesis factor prevents blood vessel growth.
- Slows/halts cell growth.
Elastic Cartilage
- Strength elasticity, maintains shape.
Hyaline Cartilage
- Provides surfaces for joint, flexibility support.
Osseous tissue
- Support protection (bone)
Fibrous Cartilage
- Support joins structures, strong rigidity, and has no perichondrium.
Bone Tissue
- Supports soft tissues
- Bones store calcium and phosphorus, house red bone marrow (produces blood cells), and contain yellow bone marrow (stores triglycerides).
- Compact or spongy organization.
Bone Lamellae
- (little plates) mineral salts that give bone its hardness compressive strength and collagen fibers
- Lacunae small spaces between bone lamellae that contain cells
- Canicule little canals containing processes of osteocytes provide nutrients to bone waste out.
- Osteonic canal Contains blood vessels nerve.
- spongy contains columns of bone with trabeculae that lack osteons
Interstitial growth
- Growth from within that increases the cartilage due to division of existing chondrocytes
Appositional growth:
- Growth at the outer surface of the tissue
- Cells in the inner cellular layer of the perichondrium differentiate into chondroblasts
Liquid Connective Tissue
-Has liquid as its extracellular matrix.
Blood Tissue
- Liquid extracellular matrix is called blood plasma and contains formed elements (red and white blood cells, platelets).
- Red blood cells transport oxygen,
- White blood cells involved in immunity,
- Platelets for blood clotting.
Lymph Plasma
- Extracellular matrix similar to blood.
Membranes
- Flat sheets of pliable tissue that cover or line body parts.
- Most consist of an epithelial layer and connective tissue (epithelial membranes).
- Types: mucous, serous, cutaneous (skin), and synovial membranes.
Epithelial Membranes
- Mucous membranes (mucosa) line cavities opening to the exterior (digestive canal, respiratory, genital, urinary tracts).
- Consist of epithelium and underlying connective tissue (lamina propria).
- Barrier against pathogens that secretes mucus.
- Serous membranes line cavities not open to the exterior (thoracic, abdominal cavities).
- Consist of areolar connective tissue covered by mesothelium (simple squamous epithelium).
- Parietal layer lines cavity wall; visceral layer covers organs.
- Includes pleura (lungs), pericardium (heart), and peritoneum (abdominal organs).
- Cutaneous membrane (skin) covers the body surface.
- Consists of epidermis (keratinized stratified squamous epithelium) and dermis (connective tissue).
Synovial Membranes
- Line joint cavities.
- Lack epithelium and are not epithelial membranes.
- Consist of connective tissue with or without a layer of flattened cells.
- Secrete synovial fluid for joint lubrication.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.