Podcast
Questions and Answers
What is the primary cause of diverticulosis in the colon?
What is the primary cause of diverticulosis in the colon?
- Increased intraluminal pressure at the entry points of the small arteries (correct)
- Colonic wall resistance and edema
- Chronic constipation and laxative use
- Intermittent, low intensity colonic contractions
What is the typical age range for ischemic colitis?
What is the typical age range for ischemic colitis?
- After age 70
- After age 50
- After age 60 (correct)
- After age 40
What is the primary mechanism leading to angiodysplasias?
What is the primary mechanism leading to angiodysplasias?
- Decreased colonic wall resistance and bleeding
- Obstruction of venous drainage of the colonic mucosa (correct)
- Increased intraluminal pressure and edema
- Chronic inflammation and scarring
What is the common location of angiodysplasias?
What is the common location of angiodysplasias?
What is the effect of ischemia on the colonic wall?
What is the effect of ischemia on the colonic wall?
What is a risk factor for ischemic colitis?
What is a risk factor for ischemic colitis?
What is the relationship between colonic contractions and angiodysplasias?
What is the relationship between colonic contractions and angiodysplasias?
What is the primary consequence of decreased colonic wall resistance?
What is the primary consequence of decreased colonic wall resistance?
What is the effect of chronic constipation on the colonic wall?
What is the effect of chronic constipation on the colonic wall?
What is the common feature of angiodysplasias and diverticulosis?
What is the common feature of angiodysplasias and diverticulosis?
Flashcards are hidden until you start studying
Study Notes
Causes of Hemorrhagic Digestive Illness (HDI)
- Ischemic colitis: abdominal pain and bloody diarrhea, but most often blood loss is not significant
- Infectious colitis: manifested by bloody diarrhea
- Colon cancer: most often causes intermittent, occult bleeding due to ulcerations or mucosal erosions
- Hemorrhoidic hemorrhage: painless, manifested by the emission of red blood, over the stools or at the end of defecation, not mixed with the stools
- Hemorrhage from anal fissures: similar to hemorrhoids, but accompanied by ano-rectal pain
Paraclinical Examinations
- Laboratory tests:
- Include hemogram, serum electrolytes, coagulation tests (aPTT, TP, INR), serum platelets, bleeding time - coagulation time
- Colonoscopy:
- Gold-standard method of diagnosing HDI
- Allows for biopsy samples and differential diagnosis of BII, colon cancer, histological type of polyp, etc.
- Requires prior preparation with a 4-liter polyethylene glycol (Fortrans) substance
- Flexible sigmoidoscopy:
- Evaluates the rectum and the left side of the colon without standard training
- Inadequate for the evaluation of the anal canal
Other Conditions Responsible for HDI
- Anal fissures
- Ano-rectal fistulas
- Coagulopathies of any kind
- Vascular disorders (Enteral infarction)
- Accidental, iatrogenic trauma
- Bacterial infectious colitis (Campylobacter jejuni, Salmonella, Shigella, enterohemorrhagic E coli, Clostridium difficile)
- Viral infectious colitis (Cytomegalovirus)
Clinical Picture
- HDI can manifest in two ways:
- When the source of the bleeding is located on the right colon: melena or haematochesia
- When the source is located on the left colon or rectum: rectoragy
- Associated symptoms and signs range from mild, asymptomatic forms to signs of hemodynamic shock
- Clinical manifestations of shock include:
- Hypotension
- Tachycardia
- Cold extremities
- Intense sweating
- Obnubility
- Indirect manifestations of HDI include:
- Tegumental pallor
- Fatigue
- Dizziness
- Lipotemia
- Collapse
Specific Clinical Aspects
- Diverticular haemorrhage:
- Sudden onset by recoragy with fresh, red blood
- Pain-free
- In most patients, the bleeding stops spontaneously
- Inflammatory bowel disease:
- Ulcerative colitis causes bloody diarrhea in most patients
- HDI in Chron's Disease is rare
Etiology
- The most common causes of HDI are:
- Diverticulosis
- Hemorrhoids
- Ischemic lesions
- Inflammatory bowel disease
- Polypectomys
- Colon cancer / Colon polyps
- Rectal ulcer
- Angiodisplasias
- Colitis / irradiation processes
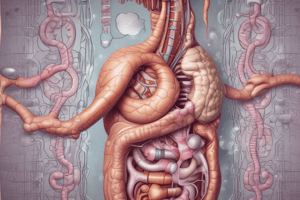
Diverticulosis
- Hernias of the mucosa and submucosa through the muscular layers of the colon
- Formed when the tissue is pushed due to the increased intraluminal pressure at the entry points of the small arteries (rectal vein) into the muscular layer of the colonic wall
- Weaknesses where the mucosa and submucosa herniate when the intraluminal pressure is increased
Ischemic Colitis
- Disorder most commonly seen after age 60
- Risk factors:
- Old-age
- Shock
- Cardio-vascular or abdominal surgery
- Heart failure
- Colon cancer
- Chronic constipation
- Long-term use of laxatives
- Ischemia causes decreased colonic wall resistance, edemas and bleedings
Angiodysplasias
- Arteriovenous malformations commonly located in the cecum or ascending colon
- Usually occur after the age of 60 years
- Occur due to chronic, intermittent, low-intensity colonic contractions that obstruct the venous drainage of the colonic mucosa
- Dilation of the capillaries in the colonic mucosa with time, leading to the occurrence of arteriovenous malformations
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.