Podcast
Questions and Answers
What are the two bones that form the lateral and anterior walls of the bony pelvis?
What are the two bones that form the lateral and anterior walls of the bony pelvis?
- Lumbar vertebrae
- Iliacus muscles
- Sacrum and coccyx
- Hip bones (correct)
What is the clinical importance of the false pelvis?
What is the clinical importance of the false pelvis?
- It helps guide the fetus into the true pelvis
- It is of little clinical importance (correct)
- It supports the abdominal cavity
- It supports the gravid uterus
What is the function of the bony pelvis during the early stages of labor?
What is the function of the bony pelvis during the early stages of labor?
- It forms a strong basin-shaped structure
- It helps guide the fetus into the true pelvis (correct)
- It supports the gravid uterus
- It supports the abdominal cavity
What is the function of the bony pelvis in supporting the abdominal contents?
What is the function of the bony pelvis in supporting the abdominal contents?
At what stage of pregnancy does the bony pelvis begin to support the gravid uterus?
At what stage of pregnancy does the bony pelvis begin to support the gravid uterus?
What is the function of the sacrum and coccyx in the bony pelvis?
What is the function of the sacrum and coccyx in the bony pelvis?
What is the name of the notch behind the acetabulum?
What is the name of the notch behind the acetabulum?
What is the function of the sacrotuberous and sacrospinous ligaments?
What is the function of the sacrotuberous and sacrospinous ligaments?
Which part of the hip bone possesses the iliac crest?
Which part of the hip bone possesses the iliac crest?
What is the purpose of the iliopectineal line?
What is the purpose of the iliopectineal line?
What is the region called where the auricular surface is located?
What is the region called where the auricular surface is located?
What is the lower and posterior part of the hip bone called?
What is the lower and posterior part of the hip bone called?
What is the name of the bony prominence on the posterior surface of the ilium?
What is the name of the bony prominence on the posterior surface of the ilium?
Which structure runs between the anterior and posterior superior iliac spines?
Which structure runs between the anterior and posterior superior iliac spines?
What forms the pelvic brim?
What forms the pelvic brim?
Why is the anatomy of the true pelvis important in females?
Why is the anatomy of the true pelvis important in females?
What is the shape of the pelvic outlet?
What is the shape of the pelvic outlet?
What forms the boundaries of the pelvic outlet?
What forms the boundaries of the pelvic outlet?
What is the posterior boundary of the pelvic inlet?
What is the posterior boundary of the pelvic inlet?
What is the function of the pelvic inlet?
What is the function of the pelvic inlet?
What are the boundaries of the pelvic inlet?
What are the boundaries of the pelvic inlet?
What is the main difference between the male and female pelvis?
What is the main difference between the male and female pelvis?
What is the primary function of the sacroiliac joints?
What is the primary function of the sacroiliac joints?
What is the main action of the levator ani muscles on the anorectal junction?
What is the main action of the levator ani muscles on the anorectal junction?
What is the function of the illolumbar ligament?
What is the function of the illolumbar ligament?
What is the characteristic of the sacroiliac joint in older people?
What is the characteristic of the sacroiliac joint in older people?
What is the function of the coccygeus muscle?
What is the function of the coccygeus muscle?
What is the nerve supply of the coccygeus muscle?
What is the nerve supply of the coccygeus muscle?
What type of joints are the sacroiliac joints?
What type of joints are the sacroiliac joints?
What is the type of joint that the symphysis pubis is?
What is the type of joint that the symphysis pubis is?
What is the primary function of the levator ani muscles in the female?
What is the primary function of the levator ani muscles in the female?
What is the main function of the posterior and interosseous ligaments in the sacroiliac joint?
What is the main function of the posterior and interosseous ligaments in the sacroiliac joint?
What type of disc connects the vertebral joints in the sacrum?
What type of disc connects the vertebral joints in the sacrum?
What is the result of hormonal changes on the symphysis pubis and ligaments during pregnancy?
What is the result of hormonal changes on the symphysis pubis and ligaments during pregnancy?
What is the nerve supply of the sacroiliac joint?
What is the nerve supply of the sacroiliac joint?
What is the joints between the bodies of the last sacral vertebra and the first coccygeal vertebra?
What is the joints between the bodies of the last sacral vertebra and the first coccygeal vertebra?
What is the movement possible at the sacrococcygeal joint?
What is the movement possible at the sacrococcygeal joint?
What is the possible symptom of sacroiliac joint disease?
What is the possible symptom of sacroiliac joint disease?
Where is the medial end of the inguinal ligament attached?
Where is the medial end of the inguinal ligament attached?
In which location is the sacral hiatus situated?
In which location is the sacral hiatus situated?
What is the name of the bony prominence that can be felt beneath the skin in the male?
What is the name of the bony prominence that can be felt beneath the skin in the male?
In which direction does the examining finger move to palpate the tubercle in the male?
In which direction does the examining finger move to palpate the tubercle in the male?
What is the location of the anterior superior iliac spine?
What is the location of the anterior superior iliac spine?
What is the relation of the sacral hiatus to the extradural space?
What is the relation of the sacral hiatus to the extradural space?
Where is the pubic tubercle located?
Where is the pubic tubercle located?
What is the level of the posterior superior iliac spine in relation to the sacral spine?
What is the level of the posterior superior iliac spine in relation to the sacral spine?
What is the characteristic of the iliac crest?
What is the characteristic of the iliac crest?
What is the location of the anterior superior iliac spine?
What is the location of the anterior superior iliac spine?
What is the characteristic of the symphysis pubis?
What is the characteristic of the symphysis pubis?
What is the location of the sacroiliac joint in relation to the sacrum and coccyx?
What is the location of the sacroiliac joint in relation to the sacrum and coccyx?
What is the relation between the pubic crest and the pubic tubercle?
What is the relation between the pubic crest and the pubic tubercle?
What is the level of the pubic tubercle in relation to the pubic bone?
What is the level of the pubic tubercle in relation to the pubic bone?
What is the location of the sacral plexus?
What is the location of the sacral plexus?
What is the origin of the lumbosacral trunk?
What is the origin of the lumbosacral trunk?
What is the direction of the obturator nerve?
What is the direction of the obturator nerve?
What is the path of the obturator nerve?
What is the path of the obturator nerve?
What is the distribution of the obturator nerve?
What is the distribution of the obturator nerve?
What is the function of the sensory branches of the pelvic nerves?
What is the function of the sensory branches of the pelvic nerves?
What is the relation of the lumbar plexus to the posterior abdominal wall?
What is the relation of the lumbar plexus to the posterior abdominal wall?
What is the formation of the lumbosacral trunk?
What is the formation of the lumbosacral trunk?
What is the primary function of the pelvic splanchnic nerves?
What is the primary function of the pelvic splanchnic nerves?
Where do the preganglionic fibers of the pelvic splanchnic nerves arise from?
Where do the preganglionic fibers of the pelvic splanchnic nerves arise from?
What is the destination of the superior rectal artery?
What is the destination of the superior rectal artery?
Where do the external iliac arteries terminate?
Where do the external iliac arteries terminate?
What is the distribution of parasympathetic fibers through the hypogastric plexuses and the aortic plexus?
What is the distribution of parasympathetic fibers through the hypogastric plexuses and the aortic plexus?
What is the course of the external iliac artery?
What is the course of the external iliac artery?
What is the origin of the internal iliac artery?
What is the origin of the internal iliac artery?
What is the characteristic of the arteries related to the pelvic walls?
What is the characteristic of the arteries related to the pelvic walls?
What is the significance of the lilac crest in relation to the peritoneum?
What is the significance of the lilac crest in relation to the peritoneum?
What is the main difference between the false pelvis and the true pelvis in terms of their contents?
What is the main difference between the false pelvis and the true pelvis in terms of their contents?
What is the function of the pelvic diaphragm in the pelvic cavity?
What is the function of the pelvic diaphragm in the pelvic cavity?
What is the significance of the sacroiliac joints in terms of childbirth?
What is the significance of the sacroiliac joints in terms of childbirth?
What is the name of the ligaments that help form the greater and lesser sciatic foramina?
What is the name of the ligaments that help form the greater and lesser sciatic foramina?
What is the purpose of the levator ani muscles in the pelvic cavity?
What is the purpose of the levator ani muscles in the pelvic cavity?
What is the significance of the pelvic brim in the pelvic cavity?
What is the significance of the pelvic brim in the pelvic cavity?
What is the characteristic of the pelvis in terms of sexual dimorphism?
What is the characteristic of the pelvis in terms of sexual dimorphism?
What is the primary function of the pelvic cavity?
What is the primary function of the pelvic cavity?
What is the significance of the pelvic cavity in emergency situations?
What is the significance of the pelvic cavity in emergency situations?
What is the relationship between the pelvic diaphragm and the pelvic cavity?
What is the relationship between the pelvic diaphragm and the pelvic cavity?
What is the significance of the perineum in relation to the pelvic cavity?
What is the significance of the perineum in relation to the pelvic cavity?
What is the relationship between the pelvic cavity and the intestinal tract?
What is the relationship between the pelvic cavity and the intestinal tract?
What is the significance of the pelvic cavity in males?
What is the significance of the pelvic cavity in males?
What is the relationship between the pelvic cavity and the lymphatic system?
What is the relationship between the pelvic cavity and the lymphatic system?
What is the boundary between the pelvic cavity and the perineum?
What is the boundary between the pelvic cavity and the perineum?
What is the role of abdominal muscles in assisting micturition?
What is the role of abdominal muscles in assisting micturition?
In young children, micturition is a
In young children, micturition is a
Which nerve carries most afferent impulses during micturition?
Which nerve carries most afferent impulses during micturition?
What is the function of the sphincter vesicae?
What is the function of the sphincter vesicae?
Which segments of the spinal cord receive afferent impulses from the urethra?
Which segments of the spinal cord receive afferent impulses from the urethra?
What is the role of the cerebral cortex in micturition?
What is the role of the cerebral cortex in micturition?
Which muscle helps to close the urethra?
Which muscle helps to close the urethra?
What is the function of the sympathetic fibers in relation to micturition?
What is the function of the sympathetic fibers in relation to micturition?
Which spinal cord segments receive afferent impulses from the urinary tract?
Which spinal cord segments receive afferent impulses from the urinary tract?
What is the function of the postganglionic neurons in the bladder wall?
What is the function of the postganglionic neurons in the bladder wall?
Which nerve carries efferent parasympathetic impulses from the spinal cord to the bladder wall?
Which nerve carries efferent parasympathetic impulses from the spinal cord to the bladder wall?
Which type of impulses pass through the pudendal nerve to the external urethral sphincter?
Which type of impulses pass through the pudendal nerve to the external urethral sphincter?
What is the location of the hypogastric plexus?
What is the location of the hypogastric plexus?
What is the effect of postganglionic neurons on the sphincter vesicae?
What is the effect of postganglionic neurons on the sphincter vesicae?
Which spinal cord segments give rise to efferent parasympathetic impulses that innervate the bladder?
Which spinal cord segments give rise to efferent parasympathetic impulses that innervate the bladder?
What is the function of the somatic efferent impulses that pass through the pudendal nerve?
What is the function of the somatic efferent impulses that pass through the pudendal nerve?
Where is the bladder typically located in children?
Where is the bladder typically located in children?
What is the normal capacity of the adult bladder?
What is the normal capacity of the adult bladder?
Where is the pain often referred to when a calculus enters the lower pelvic part of the ureter in the male?
Where is the pain often referred to when a calculus enters the lower pelvic part of the ureter in the male?
What is the result of urinary obstruction in males?
What is the result of urinary obstruction in males?
Where can the full bladder in the adult be palpated through?
Where can the full bladder in the adult be palpated through?
What is the significance of the narrowed anatomical sites of the ureter?
What is the significance of the narrowed anatomical sites of the ureter?
What is the age range when voluntary control of micturition normally develops?
What is the age range when voluntary control of micturition normally develops?
In which segment of the spinal cord is the voluntary control of micturition located?
In which segment of the spinal cord is the voluntary control of micturition located?
What is the primary cause of urinary retention in adult males?
What is the primary cause of urinary retention in adult males?
What is the method of examining the bladder in males?
What is the method of examining the bladder in males?
Where does the sympathetic outflow that inhibits contraction of the detrusor muscle originate?
Where does the sympathetic outflow that inhibits contraction of the detrusor muscle originate?
What is the primary innervation of the bladder?
What is the primary innervation of the bladder?
What is the anatomic cause of urinary retention in females?
What is the anatomic cause of urinary retention in females?
What is the purpose of suprapubic aspiration?
What is the purpose of suprapubic aspiration?
What is the effect of sympathetic innervation on the bladder?
What is the effect of sympathetic innervation on the bladder?
What is the origin of parasympathetic outflow to the bladder?
What is the origin of parasympathetic outflow to the bladder?
What is the result of the destruction of the sacral segments of the spinal cord?
What is the result of the destruction of the sacral segments of the spinal cord?
What is the location of the sacral segments of the spinal cord?
What is the location of the sacral segments of the spinal cord?
What is the normal type of bladder control found in infancy?
What is the normal type of bladder control found in infancy?
What is the function of the afferent fibers from the bladder?
What is the function of the afferent fibers from the bladder?
What is the result of the cord lesion lying above the level of the parasympathetic outflow?
What is the result of the cord lesion lying above the level of the parasympathetic outflow?
What is the purpose of manual compression of the lower part of the anterior abdominal wall?
What is the purpose of manual compression of the lower part of the anterior abdominal wall?
What is the characteristic of the bladder in the autonomous bladder condition?
What is the characteristic of the bladder in the autonomous bladder condition?
What is the consequence of the cord lesion lying above the level of the parasympathetic outflow?
What is the consequence of the cord lesion lying above the level of the parasympathetic outflow?
What is the shape of the cavity of the uterine body in coronal section?
What is the shape of the cavity of the uterine body in coronal section?
What is the position of the uterus in the erect position and with the bladder empty?
What is the position of the uterus in the erect position and with the bladder empty?
What is the part of the uterus that pierces the anterior wall of the vagina?
What is the part of the uterus that pierces the anterior wall of the vagina?
What is the term for the position of the uterus when the body of the uterus is bent backward on the cervix?
What is the term for the position of the uterus when the body of the uterus is bent backward on the cervix?
What is the name of the pouch formed when the uterus is retroverted?
What is the name of the pouch formed when the uterus is retroverted?
What is the term for the position of the uterus when the fundus and body of the uterus are bent backward on the vagina?
What is the term for the position of the uterus when the fundus and body of the uterus are bent backward on the vagina?
What is the name of the canal that communicates with the cavity of the vagina?
What is the name of the canal that communicates with the cavity of the vagina?
What is the thickness of the uterus in the young nulliparous adult?
What is the thickness of the uterus in the young nulliparous adult?
What is the primary function of a bimanual uterine palpation examination?
What is the primary function of a bimanual uterine palpation examination?
What is the typical consistency of the cervix in a pregnant uterus?
What is the typical consistency of the cervix in a pregnant uterus?
What is the probable cause of varicose veins and hemorrhoids in pregnancy?
What is the probable cause of varicose veins and hemorrhoids in pregnancy?
What is the position of the uterus in most women?
What is the position of the uterus in most women?
What is the shape of the external os in a nulliparous woman?
What is the shape of the external os in a nulliparous woman?
What is the purpose of the left hand during a bimanual uterine palpation examination?
What is the purpose of the left hand during a bimanual uterine palpation examination?
What is the typical position of the uterus in a retroverted and retroflexed uterus?
What is the typical position of the uterus in a retroverted and retroflexed uterus?
What is the role of increased progesterone levels in the blood during pregnancy?
What is the role of increased progesterone levels in the blood during pregnancy?
What is the primary factor that contributes to the development of the contractility of the uterus by the end of pregnancy?
What is the primary factor that contributes to the development of the contractility of the uterus by the end of pregnancy?
What is the possible trigger for the onset of labor?
What is the possible trigger for the onset of labor?
What is the role of the round ligament of the uterus during pregnancy?
What is the role of the round ligament of the uterus during pregnancy?
What is the effect of spinal anesthesia on the uterine contractions in women in labor?
What is the effect of spinal anesthesia on the uterine contractions in women in labor?
What is the cause of the onset of labor?
What is the cause of the onset of labor?
What is the structure that represents the remains of the lower half of the gubernaculum?
What is the structure that represents the remains of the lower half of the gubernaculum?
What is the response of the uterine body to the actions of oxytocin at the end of pregnancy?
What is the response of the uterine body to the actions of oxytocin at the end of pregnancy?
What is the characteristic of the uterine muscular activity during labor?
What is the characteristic of the uterine muscular activity during labor?
What is the origin of the lymph vessels that drain into the superficial inguinal lymph nodes?
What is the origin of the lymph vessels that drain into the superficial inguinal lymph nodes?
What is the location of the uterine artery in relation to the ureter?
What is the location of the uterine artery in relation to the ureter?
What is the function of the visceral pelvic fascia surrounding the supravaginal part of the cervix?
What is the function of the visceral pelvic fascia surrounding the supravaginal part of the cervix?
What is the location of the endometrium in relation to the ovarian hormones?
What is the location of the endometrium in relation to the ovarian hormones?
What is the relation of the uterine vein to the internal iliac vein?
What is the relation of the uterine vein to the internal iliac vein?
What is the relation of the supravaginal cervix to the bladder?
What is the relation of the supravaginal cervix to the bladder?
What is the origin of the sympathetic and parasympathetic nerves that innervate the uterus?
What is the origin of the sympathetic and parasympathetic nerves that innervate the uterus?
What is the relation of the body of the uterus to the rectouterine pouch?
What is the relation of the body of the uterus to the rectouterine pouch?
What is the name of the vestigial structure located in the broad ligament, just lateral to the uterus?
What is the name of the vestigial structure located in the broad ligament, just lateral to the uterus?
What is the risk of pelvic peritonitis during a surgical procedure involving the posterior fornix?
What is the risk of pelvic peritonitis during a surgical procedure involving the posterior fornix?
What is the purpose of slightly tilting the x-ray tube during a routine anteroposterior (AP) view of the pelvis?
What is the purpose of slightly tilting the x-ray tube during a routine anteroposterior (AP) view of the pelvis?
What is the advantage of using an endoscope to view the female pelvic peritoneal cavity?
What is the advantage of using an endoscope to view the female pelvic peritoneal cavity?
What is the purpose of systematically examining an AP radiograph of the pelvis?
What is the purpose of systematically examining an AP radiograph of the pelvis?
What is the benefit of using multiple imaging modalities, such as x-rays, CT, MRI, and ultrasound, in evaluating the pelvic contents?
What is the benefit of using multiple imaging modalities, such as x-rays, CT, MRI, and ultrasound, in evaluating the pelvic contents?
What is the risk of violating the paroophoron during a surgical procedure involving the posterior fornix?
What is the risk of violating the paroophoron during a surgical procedure involving the posterior fornix?
What is the location of the uterovesical pouch in relation to the bladder?
What is the location of the uterovesical pouch in relation to the bladder?
What is the name of the cavity filled with amniotic fluid in a pregnant uterus?
What is the name of the cavity filled with amniotic fluid in a pregnant uterus?
What is the name of the pouch located posterior to the uterus and anterior to the rectum?
What is the name of the pouch located posterior to the uterus and anterior to the rectum?
What is the name of the radiopaque compound used in the hysterosalpingogram?
What is the name of the radiopaque compound used in the hysterosalpingogram?
What is the name of the structure that connects the uterus to the vagina?
What is the name of the structure that connects the uterus to the vagina?
What is the function of parasympathetic nerves in micturition?
What is the function of parasympathetic nerves in micturition?
Where does fertilization usually occur in the female reproductive system?
Where does fertilization usually occur in the female reproductive system?
What is the direction of the long axis of the uterus in relation to the vagina?
What is the direction of the long axis of the uterus in relation to the vagina?
What is the consequence of spinal cord injuries on the bladder?
What is the consequence of spinal cord injuries on the bladder?
What is the path of the vas deferens in the male reproductive system?
What is the path of the vas deferens in the male reproductive system?
What is the support of the uterus in the female reproductive system?
What is the support of the uterus in the female reproductive system?
What is the location of the ovary in the female reproductive system?
What is the location of the ovary in the female reproductive system?
What is the shape of the uterus in the female reproductive system?
What is the shape of the uterus in the female reproductive system?
What is the purpose of taking lateral and oblique views of the pelvis?
What is the purpose of taking lateral and oblique views of the pelvis?
What is visualized in a radiograph of the pelvis, in addition to the bones?
What is visualized in a radiograph of the pelvis, in addition to the bones?
What is the purpose of administering a barium enema?
What is the purpose of administering a barium enema?
What is the primary purpose of hysterochalpingography?
What is the primary purpose of hysterochalpingography?
What is the characteristic of the sigmoid colon in a barium enema?
What is the characteristic of the sigmoid colon in a barium enema?
What is the purpose of instilling viscous iodine preparations through the external os of the uterus?
What is the purpose of instilling viscous iodine preparations through the external os of the uterus?
What is the advantage of a contrast enema in examining the sigmoid colon?
What is the advantage of a contrast enema in examining the sigmoid colon?
What is the significance of the opaque medium entering the peritoneal cavity in hysterochalpingography?
What is the significance of the opaque medium entering the peritoneal cavity in hysterochalpingography?
What is the order of examination of the pelvis in a radiograph?
What is the order of examination of the pelvis in a radiograph?
What is the primary use of CT scans in pelvic imaging?
What is the primary use of CT scans in pelvic imaging?
What is the relationship between the rectum and colon in terms of caliber?
What is the relationship between the rectum and colon in terms of caliber?
What is the significance of the sections of the pelvis being photographed on their inferior surfaces?
What is the significance of the sections of the pelvis being photographed on their inferior surfaces?
What is the purpose of a sonogram of the female pelvis?
What is the purpose of a sonogram of the female pelvis?
What is the significance of air injection into the sigmoid colon after a barium enema?
What is the significance of air injection into the sigmoid colon after a barium enema?
Where does the upper half of the vagina lie?
Where does the upper half of the vagina lie?
What does the duct of the seminal vesicle form when it joins the vas deferens?
What does the duct of the seminal vesicle form when it joins the vas deferens?
Where does the parietal peritoneum continue down from?
Where does the parietal peritoneum continue down from?
What is the prostate gland situated below?
What is the prostate gland situated below?
What does the prostate gland have?
What does the prostate gland have?
What is the prostatic urethra?
What is the prostatic urethra?
What forms the shallow uterovesical pouch?
What forms the shallow uterovesical pouch?
What is the rectouterine pouch?
What is the rectouterine pouch?
Flashcards are hidden until you start studying
Study Notes
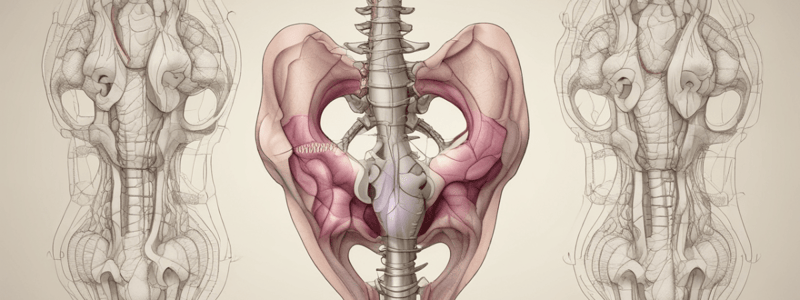
Bony Pelvis
- The bony pelvis consists of four bones: two hip bones (innominate bones), sacrum, and coccyx.
- The two hip bones form the lateral and anterior walls, and the sacrum and coccyx form the posterior wall.
False Pelvis
- The false pelvis is of little clinical importance.
- It is bounded by the lumbar vertebrae behind, iliac fossae and iliacus muscles laterally, and the lower part of the anterior abdominal wall in front.
- The false pelvis flares out at its upper end and is considered part of the abdominal cavity.
- It supports the abdominal contents and, after the 3rd month of pregnancy, helps support the gravid uterus.
- During the early stages of labor, it helps guide the fetus into the true pelvis.
True Pelvis
- The true pelvis is the lower part of the pelvis, which is important for obstetrics.
- It forms a strong basin-shaped structure.
- It is divided into an inlet, outlet, and a cavity.
- The inlet is bounded by the sacral promontory posteriorly, the iliopectineal lines laterally, and the symphysis pubis anteriorly.
Pelvic Brim
- The pelvic brim divides the pelvis into two parts: the false pelvis and the true pelvis.
- The pelvic brim is formed by the sacral promontory, iliopectineal lines, and the symphysis pubis.
Pelvic Joints
- The four major joints in the adult pelvis include paired sacroiliac joints, the symphysis pubis, and the sacrococcygeal joint.
- The sacroiliac joints are strong synovial joints between the auricular surfaces of the sacrum and the iliac bones.
- The symphysis pubis is a cartilaginous joint between the two pubic bones.
- The sacrococcygeal joint is a cartilaginous joint between the bodies of the last sacral vertebra and the first coccygeal vertebra.
Muscles and Ligaments
- The levator ani muscles of the two sides form an efficient muscular sling that supports and maintains the pelvic viscera in position.
- The coccygeus muscle forms the smaller, more posterior portion of the pelvic diaphragm.
- The nerve supply to the pelvic floor muscles is from branches of the sacral spinal nerves.
- Ligaments surround the pelvic joints, providing support and stability.
Movements
- A small amount of movement is possible at the sacroiliac joints.
- Almost no movement is possible at the symphysis pubis.
- Extensive flexion and extension are possible at the sacrococcygeal joint.
Clinical Notes
- Joint changes occur during pregnancy, with softening of the symphysis pubis and sacroiliac joints.
- Sacroiliac joint disease can produce low back pain and pain referred along the sciatic nerve (sciatica).
Pelvic Nerves
- Pelvic nerves cross the front of the sacroiliac joint and run forward on the lateral pelvic wall in the angle between the internal and external iliac vessels.
- These branches supply the pelvis and perineum, as well as the lower abdomen and lower limb.
Lumbar Plexus
- The lumbar plexus lies in the posterior abdominal wall (see Chapter 7).
- Two branches, the lumbosacral trunk and the obturator nerve, have notable relations to the pelvis.
Obturator Nerve
- The obturator nerve reaches the obturator canal (i.e., the upper part of the obturator foramen, which is devoid of the obturator membrane), and then splits into anterior and posterior divisions.
- The distribution of the obturator nerve in the thigh is considered in Chapter 11.
Lumbosacral Trunk
- Part of the anterior ramus of the fourth lumbar nerve emerges from the medial border of the psoas muscle and joins the anterior ramus of the fifth lumbar nerve to form the lumbosacral trunk.
Sacral Plexus
- The sacral plexus lies on the posterior pelvic wall in front of the piriformis muscle (see Fig. 8.18).
- It is formed from the lumbosacral trunk (see above) and the anterior rami of the first to third sacral nerves.
Pelvic Branches
- Sensory branches supply the parietal peritoneum on the lateral wall of the pelvis.
- The internal iliac, superior rectal, ovarian, and median sacral arteries run into the pelvic cavity.
Pelvic Splanchnic Nerves
- The pelvic splanchnic nerves form the parasympathetic part of the autonomic nervous system in the pelvis.
- The preganglionic fibers arise from the second, third, and fourth sacral nerves and synapse in ganglia in the inferior hypogastric plexus or in the walls of the viscera.
Arteries
- The common iliac artery ends at the pelvic inlet in front of the sacroiliac joint by dividing into the external and internal iliac arteries (see Figs. 8.10 and 8.18).
- The external iliac artery runs along the medial border of the psoas muscle, following the pelvic brim (see Fig. 6.61).
Pelvis
- The bony pelvis consists of the paired hip bones (os coxae), the sacrum, and the coccyx.
- The pelvic brim divides the pelvis into an upper false pelvis and a lower true pelvis.
- The true pelvis has an inlet (pelvic brim) above and an outlet below.
Sacrum and Coccyx
- The sacrum and coccyx have apical processes of the sacrum (see Fig. 8.22) that are fused with each other in the midline to form the median sacral crest.
- The sacral hiatus is situated on the posterior aspect of the lower end of the sacrum, where the extradural space ends.
Surface Anatomy
- The pubic tubercle can be felt on the upper border of the pubis (see Figs. 8.20 to 8.22).
- The iliac crest can be felt through the skin along its entire length (Figs. 8.20 to 8.22).
- The symphysis pubis lies in the midline between the bodies of the pubic bones and can be palpated as a solid structure through the fat in this region.
Pelvis, Part II: Pelvic Cavity
- The pelvic cavity (cavity of the true pelvis) is the area between the pelvic inlet and the pelvic outlet.
- The pelvic diaphragm subdivides the pelvic cavity into the main pelvic cavity above and the perineum below.
Components of the Pelvic Cavity
- The pelvic cavity contains the lower ends of the intestinal and urinary tracts and the internal organs of reproduction.
- It also contains the nerve supply, blood supply, and lymphatic drainage of these organs.
Gastrointestinal Tract
- The sigmoid colon is part of the pelvic cavity.
Importance of the Pelvic Cavity in Medicine
- The physician often encounters problems involving infections, injuries, and prolapses of the rectum, uterus, and vagina.
- Emergency situations involving the bladder, the pregnant uterus, ectopic pregnancy, spontaneous abortion, and acute pelvic inflammatory disease are examples of problems found in the female.
- The urinary bladder and the prostate in the male are frequent sites of disease.
Urinary Tract Nervous Control
- Nerves that control the urinary tract originate from the hypogastric plexuses and enter the spinal cord at the first and second lumbar segments
- Efferent parasympathetic impulses leave the cord from the second, third, and fourth sacral segments and pass through the pelvic splanchnic nerve and the inferior hypogastric plexus to the bladder wall
- These impulses cause the detrusor muscle to contract and the sphincter vesicae to relax
- Somatic efferent impulses also pass to the external urethral sphincter via the pudendal nerve, causing relaxation
- Afferent impulses pass up the pelvic splanchnic nerve and enter the second, third, and fourth sacral segments of the spinal cord
Micturition
- In young children, micturition is a simple reflex action that occurs whenever the bladder becomes distended
- In adults, this reflex is inhibited by the cerebral cortex until the time and place for micturition are favorable
- Voluntary control of micturition is accomplished by contracting the sphincter urethrae, which closes the urethra
- This is assisted by the sphincter vesicae, which compresses the bladder neck
- Voluntary control of micturition normally develops during the 2nd or 3rd year of life
Ureteric Calculi
- Ureteric calculi are more likely to be arrested at anatomically narrowed areas, such as the junction of the renal pelvis and ureter, and where the ureter bends down into the pelvis
- When a calculus enters the lower pelvic part of the ureter, pain is often referred to the testis and the tip of the penis in males and the labium majus in females
Bladder Distention
- The normal adult bladder has a capacity of about 500 mL
- In the presence of urinary obstruction in males, the bladder may become greatly distended without permanent damage to the bladder wall
- In such cases, it is routinely possible to drain 1000 to 1200 mL of urine through a catheter
Urinary Retention
- In adult males, urinary retention is commonly caused by obstruction to the urethra by a benign or malignant enlargement of the prostate
- Acute urethritis or prostatitis can also be responsible
- In females, acute inflammation around the urethra (e.g., from herpes) is the only anatomic cause of urinary retention
Uterus
- The uterus is a hollow, pear-shaped organ with thick muscular walls, measuring approximately 3 inches (8 cm) long, 2 inches (5 cm) wide, and 1 inch (2.5 cm) thick.
- Divided into three parts: fundus, body, and cervix.
- The fundus is the part of the uterus above the entrance of the uterine tubes.
- The body is the part of the uterus below the entrance of the uterine tubes.
- The cervix is the lower, narrow part of the uterus that pierces the anterior wall of the vagina.
Uterine Positions
- In most women, the long axis of the uterus is bent forward at a 90-degree angle to the long axis of the vagina (anteversion).
- The body of the uterus is bent forward at the level of the internal os with the long axis of the cervix (anteflexion).
- In some women, the fundus and body of the uterus are bent backward on the vagina, lying in the rectouterine pouch (retroversion).
- If the body of the uterus is bent backward on the cervix, it is said to be retroflexed.
Uterine Wall and Cavity
- The cavity of the uterine body is triangular in coronal section, but merely a cleft in the sagittal plane.
- The cavity of the cervix, the cervical canal, communicates with the cavity of the body through the internal os and with the vagina through the external os.
Blood Supply and Lymph Drainage
- The uterine artery crosses the ureter on each side of the cervix.
- The uterine vein follows the artery and drains into the internal iliac vein.
- Lymph vessels from the fundus of the uterus accompany the ovarian artery and drain into the paraaortic nodes at the level of the first lumbar vertebra.
- Vessels from the body and cervix drain into the internal and external iliac lymph nodes.
Nerve Supply
- Sympathetic and parasympathetic nerves from branches of the inferior hypogastric plexuses innervate the uterus.
Relations
- Anteriorly: The body of the uterus is related to the uterovesical pouch and the superior surface of the bladder.
- Posteriorly: The body of the uterus is related to the rectouterine pouch (pouch of Douglas) with coils of ileum or sigmoid colon within it.
Broad and Round Ligaments
- The broad ligaments and the round ligaments of the uterus are lax structures and can be pulled up or pushed down for a considerable distance before they become taut.
- The round ligament of the uterus extends between the superolateral angle of the uterus and the subcutaneous tissue of the labium majus.
Development of the Uterus
- The fundus and body of the uterus remain small until puberty, when they enlarge greatly in response to estrogens secreted by the ovaries.
Clinical Notes
- In most women, the uterus is anteverted and anteflexed.
- A retroverted, retroflexed uterus can be palpated through the posterior vaginal fornix.
- Varicose veins and hemorrhoids are common conditions in pregnancy, caused by pressure of the gravid uterus on the inferior vena cava and inferior mesenteric vein, and increased progesterone levels in the blood.
Radiographic Anatomy of the Pelvis
- The sacrum, sacroiliac joints, hip bones, and upper ends of the femurs are visible in a radiograph of the pelvis.
- Gas and fecal material may be seen in the large bowel, and soft tissue shadows of the skin and subcutaneous tissues may also be visualized.
Cross-Sectional Anatomy of the Pelvis
- Study of labeled cross-sections of the pelvis (Figs. 9.34 and 9.35) assists in interpreting computed tomography (CT) scans of the pelvis (Fig. 9.36).
- Sections are photographed on their inferior surfaces.
Gastrointestinal Tract
- The pelvic colon and rectum can be demonstrated effectively following a barium enema.
- A distended sigmoid colon usually shows no haustral-like sacculations.
- The rectum has a wider caliber than the colon.
- A contrast enema is sometimes useful for examining the mucous membrane of the sigmoid colon.
Female Genital Tract
- Instillation of viscous iodine preparations through the external os of the uterus allows visualization of the lumen of the cervical canal, the uterine cavity, and the uterine tubes (Fig. 9.37).
- Hysterosalpingography demonstrates the patency of these structures by some of the opaque medium entering the peritoneal cavity.
- Sonography can be used to visualize the pelvic organs and the developing fetus (Figs. 9.38 to 9.40).
Urinary System
- The urinary bladder lies in the pelvic cavity and is surrounded by the peritoneum.
- Micturition involves the relaxation of the internal urethral sphincter and the contraction of the detrusor muscle.
- Spinal cord injuries may disrupt the process of micturition and produce an atonic bladder, an automatic reflex bladder, or an autonomous bladder.
Male Internal Genital Organs
- The male internal genital organs are the vas deferens, seminal vesicles, ejaculatory ducts, prostate, prostatic urethra, and membranous urethra.
- The vas deferens arises from the tail of the epididymis, passes through the inguinal canal, and joins the duct of the seminal vesicle to form the ejaculatory duct.
Female Internal Genital Organs
- The uterus is a hollow, pear-shaped organ divided into the fundus, body, and cervix.
- The cervix pierces and enters the upper end of the vagina.
- The long axis of the uterus is typically bent forward at about a 90-degree angle to the long axis of the vagina, in anteversion of the uterus.
- The uterus is supported by pelvic floor muscles (elevators) and pelvic fascia ligaments (transverse cervical, pubocervical, and sacrocervical ligaments).
Pelvic Cavity
- The pelvic cavity is a region of interest in a digital vaginal examination.
- The parietal peritoneum continues down from the anterior abdominal wall onto the upper surface of the urinary bladder and then turns back onto the anterior surface of the uterus, creating the shallow uterovesical pouch.
- The peritoneum also runs over the uterus onto the upper part of the posterior surface of the vagina, and then onto the front of the rectum, creating the rectouterine pouch.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.