Podcast
Questions and Answers
Trigeminal neuralgia is characterized by brief attacks of excruciating pain. Which nerve branches are primarily involved in this condition?
Trigeminal neuralgia is characterized by brief attacks of excruciating pain. Which nerve branches are primarily involved in this condition?
- Trochlear and abducens branches
- Maxillary and mandibular branches (correct)
- Olfactory and optic branches
- Ophthalmic and auditory branches
Which of the following medications is commonly used in the treatment of trigeminal neuralgia to reduce the frequency of pain attacks?
Which of the following medications is commonly used in the treatment of trigeminal neuralgia to reduce the frequency of pain attacks?
- Oxycodone
- Acetaminophen
- Ibuprofen
- Carbamazepine (correct)
What is a primary nursing intervention for a patient experiencing an acute episode of trigeminal neuralgia?
What is a primary nursing intervention for a patient experiencing an acute episode of trigeminal neuralgia?
- Providing ice-cold liquids to soothe the affected area
- Encouraging frequent toothbrushing to maintain oral hygiene
- Avoiding touching the patient's face during care (correct)
- Applying a warm compress directly to the affected side of the face
Which cranial nerve is affected in Bell's palsy?
Which cranial nerve is affected in Bell's palsy?
What is an important nursing intervention for a patient with Bell's palsy, especially if the eyelid does not close completely?
What is an important nursing intervention for a patient with Bell's palsy, especially if the eyelid does not close completely?
In the majority of Bell's Palsy cases, what virus is suspected to be related to the cause of the inflammation
In the majority of Bell's Palsy cases, what virus is suspected to be related to the cause of the inflammation
Which of the following diagnostic findings is most indicative of bacterial meningitis?
Which of the following diagnostic findings is most indicative of bacterial meningitis?
A patient is suspected of having meningitis. What is the priority diagnostic test to perform after ruling out increased ICP?
A patient is suspected of having meningitis. What is the priority diagnostic test to perform after ruling out increased ICP?
Which of the following nursing interventions is most important for a patient with meningitis to prevent complications related to increased intracranial pressure (ICP)?
Which of the following nursing interventions is most important for a patient with meningitis to prevent complications related to increased intracranial pressure (ICP)?
Which of these is often the cause of encephalitis?
Which of these is often the cause of encephalitis?
What medication is primarily used to treat encephalitis caused by HSV (Herpes Simplex Virus)?
What medication is primarily used to treat encephalitis caused by HSV (Herpes Simplex Virus)?
What is a primary concern in the medical management of encephalitis?
What is a primary concern in the medical management of encephalitis?
What is the primary route of human infection with West Nile Virus (WNV)?
What is the primary route of human infection with West Nile Virus (WNV)?
Which measure is effective in reducing the risk of West Nile Virus (WNV) infection?
Which measure is effective in reducing the risk of West Nile Virus (WNV) infection?
What is the gold standard over-the-counter insect repellent recommended to reduce the risk of West Nile Virus (WNV)?
What is the gold standard over-the-counter insect repellent recommended to reduce the risk of West Nile Virus (WNV)?
What is the primary cause of a brain abscess?
What is the primary cause of a brain abscess?
Which organisms are most commonly implicated in causing brain abscesses?
Which organisms are most commonly implicated in causing brain abscesses?
What is the primary treatment for a brain abscess?
What is the primary treatment for a brain abscess?
Neurologic manifestations of HIV disease occur in what percentage of infected individuals?
Neurologic manifestations of HIV disease occur in what percentage of infected individuals?
Which condition is also known as subacute encephalitis and may occur in the advanced stage of HIV, AIDS?
Which condition is also known as subacute encephalitis and may occur in the advanced stage of HIV, AIDS?
What is a common nursing intervention for a patient with AIDS who is disoriented?
What is a common nursing intervention for a patient with AIDS who is disoriented?
What is the most common type of malignant brain tumor?
What is the most common type of malignant brain tumor?
Which surgical intervention involves removing part of the skull without immediate replacement?
Which surgical intervention involves removing part of the skull without immediate replacement?
A patient presents with unilateral facial weakness, inability to close the left eyelid, and drooping of the mouth. The patient reports a recent upper respiratory infection. Which of the following conditions is most likely?
A patient presents with unilateral facial weakness, inability to close the left eyelid, and drooping of the mouth. The patient reports a recent upper respiratory infection. Which of the following conditions is most likely?
A nurse is caring for a patient admitted with suspected bacterial meningitis. Which intervention is the highest priority?
A nurse is caring for a patient admitted with suspected bacterial meningitis. Which intervention is the highest priority?
A patient is diagnosed with West Nile Virus (WNV) encephalitis. Which symptom would the nurse expect to observe?
A patient is diagnosed with West Nile Virus (WNV) encephalitis. Which symptom would the nurse expect to observe?
The nurse is educating a community group about preventing West Nile virus. Which of the following instructions is most appropriate?
The nurse is educating a community group about preventing West Nile virus. Which of the following instructions is most appropriate?
A patient with Guillain-Barré Syndrome (GBS) is experiencing increasing paralysis and has a vital capacity of 18 mL/kg and is intubated. The normal vital capacity is 65 to 75 mL/kg. Which intervention is most critical?
A patient with Guillain-Barré Syndrome (GBS) is experiencing increasing paralysis and has a vital capacity of 18 mL/kg and is intubated. The normal vital capacity is 65 to 75 mL/kg. Which intervention is most critical?
A patient is diagnosed with trigeminal neuralgia and reports severe, debilitating pain. The patient is prescribed carbamazepine to manage the pain. What nursing action is most important for this patient?
A patient is diagnosed with trigeminal neuralgia and reports severe, debilitating pain. The patient is prescribed carbamazepine to manage the pain. What nursing action is most important for this patient?
During a physical examination, a nurse assesses for Brudzinski’s sign. Which technique should the nurse use to elicit this sign?
During a physical examination, a nurse assesses for Brudzinski’s sign. Which technique should the nurse use to elicit this sign?
Flashcards
Trigeminal Neuralgia
Trigeminal Neuralgia
A specific type of peripheral nerve problem causing intense facial pain.
Trigeminal Neuralgia Pain
Trigeminal Neuralgia Pain
Excruciating, sharp, shock-like pain in the lips, gums, cheek, forehead, or side of the nose.
Trigger Points
Trigger Points
Areas along a nerve where the slightest touch can trigger pain.
Carbamazepine
Carbamazepine
Signup and view all the flashcards
Bell's Palsy
Bell's Palsy
Signup and view all the flashcards
Herpes Simplex Virus (HSV)
Herpes Simplex Virus (HSV)
Signup and view all the flashcards
Recovery of Taste
Recovery of Taste
Signup and view all the flashcards
Meningitis
Meningitis
Signup and view all the flashcards
Meningitis causes
Meningitis causes
Signup and view all the flashcards
Kernig's Sign
Kernig's Sign
Signup and view all the flashcards
Brudzinski's Sign
Brudzinski's Sign
Signup and view all the flashcards
Encephalitis
Encephalitis
Signup and view all the flashcards
Encephalitis Manifestations
Encephalitis Manifestations
Signup and view all the flashcards
West Nile Virus (WNV)
West Nile Virus (WNV)
Signup and view all the flashcards
West Nile Fever
West Nile Fever
Signup and view all the flashcards
Brain Abscess
Brain Abscess
Signup and view all the flashcards
direct extension
direct extension
Signup and view all the flashcards
AIDS Dementia Complex (ADC)
AIDS Dementia Complex (ADC)
Signup and view all the flashcards
Brain Tumor
Brain Tumor
Signup and view all the flashcards
Brain Tumor Symptom
Brain Tumor Symptom
Signup and view all the flashcards
Aphasia
Aphasia
Signup and view all the flashcards
Craniectomy
Craniectomy
Signup and view all the flashcards
Craniotomy
Craniotomy
Signup and view all the flashcards
Guillain-Barré Syndrome (GBS)
Guillain-Barré Syndrome (GBS)
Signup and view all the flashcards
GBS progression
GBS progression
Signup and view all the flashcards
Study Notes
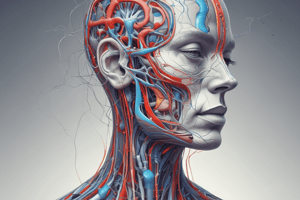
Trigeminal Neuralgia
- This is a specific type of peripheral nerve disorder
- The exact cause is unknown however degeneration or pressure on the trigeminal nerve (cranial nerve V) could be a cause
- Trigeminal Neuralgia is also known as Tic douloureux
- Affects individuals in middle or late adulthood, slightly more in women, but the pathophysiology is not fully understood
Clinical Manifestations of Trigeminal Neuralgia
- Excruciating, knifelike, or lightning-like shock in the lips, gums, cheek, forehead, or side of the nose are all symptoms
- Pain radiates along one or more of the three divisions of the fifth cranial nerve, a nerve that contains both motor and sensory branches
- The sensory (afferent) branches, mainly the maxillary and mandibular branches, are usually involved in trigeminal neuralgia
- Typically, pain only extends to the midline of the face and head where the tissue is supplied by the affected nerve
- Attacks are generally brief, lasting seconds to minutes and are typically unilateral
- One can expect Recurrences several times a day, or weeks or months apart
Trigger points
- Areas along the nerve's path are known as trigger points
- Pain can be initiated with even the slightest stimulation of these areas
- People with trigeminal neuralgia are desperate to avoid triggers
- Chewing, toothbrushing, hot or cold air, face washing, yawning, or even speaking can trigger this type on pain
Medical Management of Trigeminal Neuralgia
- Certain antiseizure medications can be administered: Carbamazepine, Phenytoin, Valproate, Gabapentin, Oxcarbazepine, Lamotrigine, and Topiramate
- Muscle relaxants such as baclofen, either alone or with antiseizure drugs can be used
- Absolute alcohol can be injected into the trigeminal nerve’s peripheral branches to damage the nerves and block pain signals, providing relief for weeks or months
- Biofeedback, acupuncture, and megavitamins have also been reported as other helpful therapies
- Surgery can result in permanent relief for pain, although other options are available
- Surgical treatments include sensory root resection, microvascular decompression, and gammaknife radiosurgery
Nursing Interventions for Trigeminal Neuralgia
- Those with Trigeminal Neuralgia may have not eaten properly and be undernourished and dehydrated
- Patients may not have been able to do self care activities such as washing, shaving, or combing their hair for hygiene purposes
- Oral hygiene is often neglected
Promoting Comfort
- Keeping the room free of drafts and at a moderate temperature, combined with non-touching of the patient's face is optimal
- Do not urge washing, shaving, or combing the hair during an acute attack
- Stress importance of hygiene, nutrition, and oral care while understanding if neglect is apparent
- Use lukewarm water and soft cloths, or cotton saturated with non-water cleaning solutions
- Use a warm mouthwash or small, soft-bristled toothbrush assists
- Peak analgesia is the optimum condition for instructing hygiene
- Refrain from the use of hot or cold liquids which can be triggers
- Puree food and ensure it is lukewarm, taking suggested through a straw is helpful
Trigeminal Neuralgia Prognosis
- The acute pain is excruciating, although it seldom lasts more than a few seconds or 2 to 3 minutes
- The onset of pain can occur at any time of the day or night and may recur several times daily and constantly for weeks
- Permanent relief from surgery is possible
Bell’s Palsy
- Also known as Peripheral Facial Paralysis
- It is an inflammatory process involving the facial nerve (cranial nerve VII)
- Evidence suggests HSV may be involved in the majority of cases, however, the exact etiology is not known
Bell’s Palsy Pathophysiology
- HSV reactivation causes inflammation, edema, ischemia, with disturbances in sensory and motor function
- One or more of the three branches of the facial nerve may be affected
Clinical Manifestations of Bell’s Palsy
- There is usually an abrupt onset of numbness, stiffness, or drawing sensation of the face
- Unilateral weakness results in flaccidity
- Inability to wrinkle the forehead, close the eyelid, pucker the lips, smile, frown, whistle, or retract the mouth on the affected side
- Asymmetric face with mouth and cheek drooping, patients often endure loss of taste, altered chewing ability, reduced salivation, pain behind the ear, and ringing in the ear
Bell’s Palsy Medical Management
- There is no specific therapy to treat Bell's Palsy
- Electrical stimulation or warm moist heat along the nerve course may help maintain muscle tone and prevent atrophy
- Corticosteroids, such as prednisone, are often started immediately, preferably before paralysis is complete
- Corticosteroids should be tapered off over two weeks when the patient improves
- Due to the implication of HSV in approximately 70% of cases acyclovir alone or in conjunction with prednisone is used
Bell’s Palsy Nursing Interventions
- Preventing excessive drying and damage to the cornea is important, eye shields should be a part of the nightly routine when the eyelid does not close
- Massage of the affected areas is sometimes recommended, as well as artificial tears
- Active facial exercises, such as wrinkling brow, forehead, closing the eyelids, and puffing out the cheeks, may be prescribed three times a day for 5 minutes
Bell’s Palsy Prognosis
- Full recovery is expected in 3 to 6 months, although it could take up to a year
- The extent of nerve damage is an indicator of time to recovery
- When there is recovery of taste within the first week this is a sign of improvement and full motor function recovery is a green light
- Another good sign- the paralysis remains incomplete in the first 5 to 7 days, with permanent paralysis being very rare
Infection and Inflammation
- Infection or inflammation can interfere with function
- Some diseases associated with infection: meningitis, encephalitis, brain abscess, GBS, herpes zoster, neuro-syphilis, poliomyelitis, and AIDS
- The skull and vertebral column, meninges, and blood-brain barrier protect the the brain and spinal cord from infective agents
- Air sinuses, middle ear, or blood can allow Infective agents to spread into the CNS
- Injuries and treatments that disrupt the dura increase infection risk: skull fractures, missile injuries, and neurosurgical procedures
Meningitis
- Meningitis (infection of the meninges) may be caused by bacteria, viruses, fungi, parasites, or other toxins -Meningitis infections are classified as acute, subacute, or chronic
- Every microorganism has different pathophysiology, presentation, and management
- The nervous system can be affected by toxins of many organisms
- Toxins can reach nervous system from sources like adjacent bones, blood, or lymph
- There can be meningitis as a result of an invasive procedure such as surgery
Assessment for Infections and Inflammation
- Subjective data includes infection history, discomfort, headache, stiff neck, sudden onset of symptoms, difficulty thinking, and weakness
- Objective data includes behavioral signs (discomfort or disorientation), inability to do ADLs, fever, vomiting, seizures, altered respiratory patterns, tachycardia, meningeal irritation, LOC, and orientation
Diagnostic Tests, Nursing Interventions, and Patient Teaching for Infections and Inflammation
- Infections of the nervous system can be diagnosed by examining the cerebral spinal fluid
- CAT scans and EECs may be used
- Patient problems and interventions for infection and inflammation are similar to patients that had a stroke
- Elevated Body Temperature, related to inflammatory response to CNS infection
- Recent Onset of Confusion, related to neurophysiologic response to infection
Nursing Interventions
- Assess temperature every 2 hours as needed
- Provide cooling measures to avoid shivering
- Administer ordered antipyretics and antibiotics and monitor parenteral fluids
- Control exposure to extremes in temperature
- Assess temperature, pulse, and respiration every 2 hours as indicated
- A kind tone, speaking in short sentences and a therapeutic attitude can promote a therapeutic environment
Teaching for Infections or Inflammation Conditions
- Educate patients about the disease process, the treatments involved, and anticipated outcomes
- If the patient is seriously ill, the starting point of education should begin with the family
- Patient teaching for motor and sensory problems may be needed depending on signs and symptoms.
Guillain-Barré Syndrome (GBS)
- Guillain-Barré Syndrome (GBS) is also called acute inflammatory polyradiculopathy or postinfectious polyneuritis
- It is an acute, rapidly progressing, and potentially fatal form of polyneuritis
- It causes widespread inflammation with demyelination of the peripheral nervous system
- Not explicitly known, it is believed to be an autoimmune reaction, involving the peripheral nerves, most often after a respiratory or gastrointestinal viral infection
- GBS has been reported as a result of common immunizations such as surgery, viral vaccinations, and Epstein-Barr
Guillain-Barré Syndrome (GBS) Etiology
- The peripheral nervous system consists of 31 pairs of spinal nerves, 12 pairs of cranial nerves, and various plexuses and ganglia
- Communication is possible using neuronal communication and structure like the axon which is insulated by myelin sheaths that consist of Schwann cells
- In people with GBS the antibodies attack the Schwann cells, causing the myelin sheath to break down (demyelination) resulting in inflamed and uninsulted nerve portions
- Classical indicators: Weakness, Tingling, and Numbness, because proper neuronal communication is interrupted
Guillain-Barré Syndrome (GBS) Symptoms
- Symptoms start in the legs or feet and travel upward because signals travel to and from the legs the furthest distance
- The demyelination is self-limiting and Schwann cells rebuild the lost insulation stopping demyelination
- Remyelination and recovery takes places in reverse working from the head to feet
Clinical Manifestations of Guillain-Barré Syndrome (GBS)
- There is variation in the onset of weakness and in the rate of progression of symptoms
- Progression can stop at any point, and If cranial nerves VII, IX, and X are involved then the patient may have difficulty swallowing, breathing, and speaking
- Paralysis usually starts in the lower extremities and moves upward to include the thorax, the upper extremities, and the face, along with symmetrical muscle weakness and motoneuron paralysis
- If the intercostal muscles are affected respiratory failure may occur Fluctuating blood pressure may occur as a result to the autonomic nervous system
Diagnostic Tests for Guillain-Barré Syndrome (GBS)
- GBS gets diagnosed by eliminating other causes for the signs and symptoms and assessing for characteristic muscle weakness
- A CT scan rules out tumors or stroke, while changes in the respiratory status may aid in the diagnosis and a lumbar puncture is done
- Elevated levels are common in CSF of those with GBS
- To test for slow impulse transmission, nerve conduction velocity studies will be ordered
- Expect Electromyography and nerve conduction studies as markedly abnormal and a recent history of a recent infection
Medical Management of Guillain-Barré Syndrome (GBS)
- Since GBS can accelerate rapidly and paralysis can impair respiratory muscles, hospitalization should be immediate
- Therapeutic plasmapheresis, the removal, cleaning, and returning of unwanted or pathologic components from blood serum in the first 2 weeks can decrease severity and length of infection and adrenocortical steroids treat symptoms
- IV immune globulin (Sandoglobulin) can be an alternative, and patients receiving high-dose immune globulin need to be well hydrated and have adequate renal function
- Mechanical ventilation and a tracheostomy can be interventions for those with respiratory failure. Close ABG monitoring and pulmonary function tests are important
Nursing Interventions and Prognosis of Guillain-Barré Syndrome (GBS)
- Cognition is not impaired, and reassurance is helpful because patients require ventilation
- Nutrition may require enteral (IV infusion) or a nasogastric tube
- Maintaining motor abilities, prevention of complications and ROM are an important factor
- Help neuropathic pain by using drugs like Gabapentin or other tricyclic antidepressant like Amitriptyline.
- Closely monitor respiratory function with vitals
- Long term weakness can be experienced 15% of the time with post disease reports being fatigue is common
- Total recovery varies between weeks to years and can require medical interventions
- Supporting acute patients with the disease correlates how well a patient can recover
Meningitis Transmission
- Causes can be viral, bacterial, or even fungal
- Pneumococci, meningococci, staphylococci, streptococci, and Haemophilus influenzae are major bacteria causes with possibilities from viral agents, fungi, parasites or toxins
- The actual microorganisms cause different effects during transmission and development depending on origin and pathophysiology
Bacterial vs Viral Meningitis
High protein and white blood cell levels in the CSF, with bacteria causing an inflammatory reaction in the pia mater and pus accumulation where injury to tissue may occur
- Bacterial is classified as Septic. This infection is diagnosed commonly in the Winter
- Classified as aseptic, Viral meningitis diagnosis is more common during Fall with upper respiratory tract infections as common indicators
Diagnostic Signs
- Kernig’s Sign - Inability to straighten legs with pain
- Brudzinski’s Sign- Flexion of the knees and hips when flexing the neck Signs show intense headache, neck stiffness, irritability, and nausea
Medical Interventions for Meningitis
- Antibiotics by IV for 2 weeks
- Possible medications are ampicillin, ceftriaxone, penicillin, and others
- To decrease ICP using corticosteroids along with anticonvulsants to help prevent the possibilities of seizures
- Aseptic Meningitis can be suppressed by using the supportive medical interventions to help ensure balancing of key electrolytes
Nursing Interventions for Meningitis
- Respiratory isolation due to cultures can have risks when pathogen’s is unsuppressed
- Antibiotic therapy is only effective later on and dehydration of nasal passages is very common when infected and other nursing interventions are to care for patients who have critical illness or illness along with administering fluids
- Seizure prevention is important from stimuli as the room needs to be darkened
- Manage a patient's fever
- Cooling is important to control swelling
- Cool the body from neurological damage
Encephalitis
- Encephalitis is an acute inflammation of the brain from a viral infection
- Epidemic encephalitis cases are transmitted by mosquitoes and ticks, with cases occurring often as complications from mumps or chickenpox
- Signs are similar to meningitis as well, which includes similar onset involving signs such as fever, high and severe headaches, a patient can undergo seizures, coupled with a change in LOC
Diagnoses for Encephalitis:
- Encephalitis diagnoses are early on to have favorable outcomes
- Use brain imaging (MRI and PET scans) to detect for this certain illness
Medical Interventions:
- Symptomatic and supportive
- Diuretics are efficient to help diminish brain functioning
- Damage is likely in neurological activity which in turn can progress swelling to spread even further from nerve tissues
Acyclovir Implications:
- Used to treat encephalitis by the HSV infection from fewer side effects than vidarabine
- The best choice is before coma
West Nile Virus (WNV)
- Commonly found in the Middle East, Africa, and Eastern Europe, but undocumented in the US until 1999 to carry the virus and infect horses, birds, humans, and mosquitoes
Transmission and Incubation
- Mosquitoes will become infected if they bite a bird that is carrying the virus
- Transmissions into humans must be from a mosquito
- Incubation takes 2-14 days
WNV symptoms:
- Resembles the flu
- Fever, headache, and anorexia lasting a few days
- Meningitis can have chills, illness, and headaches
- Encephalitis can influence neurological and behavioral signs coupled with confusion or even a coma
Diagnoses and Cautions:
- Blood/CSF samples help with Immunoglobulin
- Be cautious when symptoms strike as the virus can spread, a recently vaccinated patient can test very positive
- Casual Contact is extremely rare for it to spread as the virus is often transmitted through contact, such as even pregnancy or during blood transfusions
Preventions and Patient Teaching
- Insect repellent to exposed areas as it decreases the viral spread, containing DEET
- Cover all areas during trips to the outdoors
- Make sure to take precautions between April to October for high transmission
- DEET is currently the golden standard used ever since the US Army as it contains a remarkable safety profile for others
WNV Safety- DEET Misuse
- Toxic reactions as a result from excessive use
- Eye and Inhalation irritation
- It’s only a Class D due to 30% concentration, which is not harmful, but has possibilities if not controlled
Infection Control
- Limit outdoors activity as this helps with transmission control due to windows needing to be repaired
- Also include mosquito repellent and containers filled with fluid to avoid infection
- Encephalitis has potential complications
Medical Interventions
- Support the nervous and immune systems during illness with fever, pain, and nausea management
- Encephalitis patients must undergo a variety of other therapies, such as ventilation and more care in intensive units to help prevent death and potential infection
Abscess in the Brain
- Pus accumulated within the brain causes this
- From sinus, tooth or ear infections
- Brain Abscess can develop with thrombosis from bacterial and fungal infections
- Primary infectors can be staphylococci and streptococci
Manifestations and Symptoms in Neurological Problems:
- Infection in the brain that causes issues like meningitis and encephalitis
- Symptoms can be headache, increased ICP, drowsiness, confusion or seizures
Symptom Interventions:
- Antimicrobial, Symptomatic Relief, Drainage and Removal
- In severe cases, the medication is not affective unless the abscess is drained if the capsules are impenetrable
- Prevention measures can be meningitis management
Brain Tumor Prognosis
- Can increase the risk of seizure and other sicknesses involving the blood-brain, especially with the infection
- There are cases that result in death
Acquired Immunodeficiency Syndrome (AIDS)
- AIDS as the last term for HIV(Neurological issues in the nervous system)
- Signs/Symptoms: Associated HIV infection from neurologic signs
- Meningitis herpes, shingles, tumors with cryptococcal diagnosis
- Causes headaches, palsies, and more issues of neurological pain ADC- Brain loss memory, dementia
Diagnoses and Treatment
- Diagnoses helps with any neurological effects that have serologic effects or implications with HIV(MRI< CT, Spinal tap for any spinal/brain fluids)
- Treatment depending what’s happening with the infection Used to combat dehydration with fluid from various sources
- Use medication from those as well for seizures (Diazepam, phenytoin, Fosphenytoin)
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.