Podcast
Questions and Answers
What is the age range when Trigeminal Neuralgia usually occurs?
What is the age range when Trigeminal Neuralgia usually occurs?
- 30-50
- 70-90
- 50-70 (correct)
- 20-40
Which of the following is NOT a characteristic of Trigeminal Neuralgia?
Which of the following is NOT a characteristic of Trigeminal Neuralgia?
- No structural damage to the neurons
- Bilateral (correct)
- Unilateral
- Affects both motor and sensory functions
Which division of the trigeminal nerve is less commonly affected in Trigeminal Neuralgia?
Which division of the trigeminal nerve is less commonly affected in Trigeminal Neuralgia?
- Mandibular
- Frontal
- Maxillary
- Ophthalmic (correct)
What is the name of the muscle that the trigeminal nerve supplies motor function to?
What is the name of the muscle that the trigeminal nerve supplies motor function to?
What is the duration of each bout of pain in Trigeminal Neuralgia?
What is the duration of each bout of pain in Trigeminal Neuralgia?
In which condition may Trigeminal Neuralgia be an early sign?
In which condition may Trigeminal Neuralgia be an early sign?
What is the name of the part of the brain where the trigeminal nerve exits?
What is the name of the part of the brain where the trigeminal nerve exits?
What is the gender that is more affected by Trigeminal Neuralgia?
What is the gender that is more affected by Trigeminal Neuralgia?
What is the primary consideration when testing for trigeminal neuralgia?
What is the primary consideration when testing for trigeminal neuralgia?
Why may a client with trigeminal neuralgia be referred to an MD?
Why may a client with trigeminal neuralgia be referred to an MD?
What is the recommended position for a client with trigeminal neuralgia during massage therapy?
What is the recommended position for a client with trigeminal neuralgia during massage therapy?
What is a contraindication for massage therapy in clients with trigeminal neuralgia?
What is a contraindication for massage therapy in clients with trigeminal neuralgia?
What is the goal of massage therapy for clients with trigeminal neuralgia?
What is the goal of massage therapy for clients with trigeminal neuralgia?
What is a common medication used to treat trigeminal neuralgia?
What is a common medication used to treat trigeminal neuralgia?
What is a possible surgical approach for treating trigeminal neuralgia?
What is a possible surgical approach for treating trigeminal neuralgia?
What is a possible outcome of severe trigeminal neuralgia treatment?
What is a possible outcome of severe trigeminal neuralgia treatment?
Why is it important to consider other conditions that may mimic trigeminal neuralgia during assessment?
Why is it important to consider other conditions that may mimic trigeminal neuralgia during assessment?
What is an important consideration when providing massage therapy for clients with trigeminal neuralgia resulting from pathologies such as MS or RA?
What is an important consideration when providing massage therapy for clients with trigeminal neuralgia resulting from pathologies such as MS or RA?
What are the three divisions of the Trigeminal Nerve?
What are the three divisions of the Trigeminal Nerve?
Which muscle is responsible for tensor tympani?
Which muscle is responsible for tensor tympani?
What is the most common location of the trigger zone in Trigeminal Neuralgia?
What is the most common location of the trigger zone in Trigeminal Neuralgia?
What is a common cause of Trigeminal Neuralgia?
What is a common cause of Trigeminal Neuralgia?
What is the recommended position for a person with Trigeminal Neuralgia during massage therapy?
What is the recommended position for a person with Trigeminal Neuralgia during massage therapy?
What is the duration of pain in Trigeminal Neuralgia?
What is the duration of pain in Trigeminal Neuralgia?
What is a secondary symptom of Trigeminal Neuralgia?
What is a secondary symptom of Trigeminal Neuralgia?
What is the impact of Trigeminal Neuralgia on daily activities?
What is the impact of Trigeminal Neuralgia on daily activities?
What is a common description of the pain in Trigeminal Neuralgia?
What is a common description of the pain in Trigeminal Neuralgia?
What is the importance of assessment in Trigeminal Neuralgia?
What is the importance of assessment in Trigeminal Neuralgia?
Which cranial nerve is affected in Bell's palsy?
Which cranial nerve is affected in Bell's palsy?
What is the most common neurological condition affecting how many people each year?
What is the most common neurological condition affecting how many people each year?
What is the duration of the abrupt rapid onset of Bell's palsy?
What is the duration of the abrupt rapid onset of Bell's palsy?
Which muscle is NOT supplied by the facial nerve?
Which muscle is NOT supplied by the facial nerve?
Where does the facial nerve pass through?
Where does the facial nerve pass through?
What is the prognosis of Bell's palsy that results from complete compression?
What is the prognosis of Bell's palsy that results from complete compression?
What percentage of Bell's palsy cases recover spontaneously?
What percentage of Bell's palsy cases recover spontaneously?
Through which foramen does the facial nerve exit?
Through which foramen does the facial nerve exit?
What is the direction of pressure applied during facial massage for clients with facial paralysis?
What is the direction of pressure applied during facial massage for clients with facial paralysis?
Why is it important to keep the affected eye covered during facial massage?
Why is it important to keep the affected eye covered during facial massage?
What is the purpose of having the client practice facial exercises during remedial exercise and self-care?
What is the purpose of having the client practice facial exercises during remedial exercise and self-care?
What is the recommended frequency for using lubricating ointment for clients with facial paralysis?
What is the recommended frequency for using lubricating ointment for clients with facial paralysis?
What is a common risk factor for non-recovery of facial paralysis?
What is a common risk factor for non-recovery of facial paralysis?
What is the purpose of lymphatic drainage for the face and neck during facial massage?
What is the purpose of lymphatic drainage for the face and neck during facial massage?
Why is it important to stabilize the head during facial massage for clients with facial paralysis?
Why is it important to stabilize the head during facial massage for clients with facial paralysis?
What is the percentage of clients with facial paralysis who recover within 6 months?
What is the percentage of clients with facial paralysis who recover within 6 months?
What muscles are affected in Bell's palsy?
What muscles are affected in Bell's palsy?
Which salivary gland is affected in Bell's palsy?
Which salivary gland is affected in Bell's palsy?
What is a common symptom of Bell's palsy?
What is a common symptom of Bell's palsy?
What is a possible cause of Bell's palsy?
What is a possible cause of Bell's palsy?
How is the affected eye affected in Bell's palsy?
How is the affected eye affected in Bell's palsy?
What is the purpose of wearing a patch over the eye in Bell's palsy?
What is the purpose of wearing a patch over the eye in Bell's palsy?
What is a common sign of Bell's palsy?
What is a common sign of Bell's palsy?
What is the goal of massage therapy in Bell's palsy?
What is the goal of massage therapy in Bell's palsy?
What is an important consideration during assessment of Bell's palsy?
What is an important consideration during assessment of Bell's palsy?
What is a possible outcome of Bell's palsy?
What is a possible outcome of Bell's palsy?
What is the compression syndrome of the brachial plexus within the shoulder girdle?
What is the compression syndrome of the brachial plexus within the shoulder girdle?
Which muscles form the interscalene triangle?
Which muscles form the interscalene triangle?
What space narrows when the shoulder is fully abducted and externally rotated?
What space narrows when the shoulder is fully abducted and externally rotated?
What is the course of the neurovascular bundle?
What is the course of the neurovascular bundle?
What is the function of the brachial plexus?
What is the function of the brachial plexus?
What is the effect of slouching forward on the costoclavicular space?
What is the effect of slouching forward on the costoclavicular space?
What is the effect of taking a deep inhale on the interscalene triangle?
What is the effect of taking a deep inhale on the interscalene triangle?
What is the effect of a tight subclavius muscle on the costoclavicular space?
What is the effect of a tight subclavius muscle on the costoclavicular space?
Which of the following does not involve the subclavian vein in Thoracic Outlet Syndrome?
Which of the following does not involve the subclavian vein in Thoracic Outlet Syndrome?
What is the typical presentation of Thoracic Outlet Syndrome?
What is the typical presentation of Thoracic Outlet Syndrome?
What is a possible symptom of neurological involvement in Thoracic Outlet Syndrome?
What is a possible symptom of neurological involvement in Thoracic Outlet Syndrome?
Which of the following can cause compression of the neurovascular bundle?
Which of the following can cause compression of the neurovascular bundle?
What is a possible outcome of severe Thoracic Outlet Syndrome?
What is a possible outcome of severe Thoracic Outlet Syndrome?
What is a common location of trigger points in Thoracic Outlet Syndrome?
What is a common location of trigger points in Thoracic Outlet Syndrome?
What is a possible sign of vascular involvement in Thoracic Outlet Syndrome?
What is a possible sign of vascular involvement in Thoracic Outlet Syndrome?
What is a common postural assessment finding in Thoracic Outlet Syndrome?
What is a common postural assessment finding in Thoracic Outlet Syndrome?
What is a possible cause of Thoracic Outlet Syndrome?
What is a possible cause of Thoracic Outlet Syndrome?
What is a common finding on palpation in Thoracic Outlet Syndrome?
What is a common finding on palpation in Thoracic Outlet Syndrome?
What is the primary goal of treatment for thoracic outlet syndrome?
What is the primary goal of treatment for thoracic outlet syndrome?
What is the name of the syndrome that involves compression of the brachial plexus and subclavian artery between the anterior and/or middle scalene?
What is the name of the syndrome that involves compression of the brachial plexus and subclavian artery between the anterior and/or middle scalene?
What is the name of the test used to assess the length of the Pectoralis Minor muscle?
What is the name of the test used to assess the length of the Pectoralis Minor muscle?
What is the name of the technique used to retrain apical breathers and reduce stress on the scalenes?
What is the name of the technique used to retrain apical breathers and reduce stress on the scalenes?
What is a contraindication for massage therapy in clients with thoracic outlet syndrome?
What is a contraindication for massage therapy in clients with thoracic outlet syndrome?
What is the recommended frequency of treatment for thoracic outlet syndrome?
What is the recommended frequency of treatment for thoracic outlet syndrome?
What is the purpose of joint play to the cervical spine, sternoclavicular, and GH joints in the treatment of thoracic outlet syndrome?
What is the purpose of joint play to the cervical spine, sternoclavicular, and GH joints in the treatment of thoracic outlet syndrome?
What is the name of the test used to assess for compression of the brachial plexus, subclavian artery, and vein between the clavicle and the first rib?
What is the name of the test used to assess for compression of the brachial plexus, subclavian artery, and vein between the clavicle and the first rib?
What is the name of the technique used to release tension in the Scalenes, Pectoralis Minor, and Subclavius muscles?
What is the name of the technique used to release tension in the Scalenes, Pectoralis Minor, and Subclavius muscles?
What is the importance of client compliance to self-care and avoidance of aggravating factors in the treatment of thoracic outlet syndrome?
What is the importance of client compliance to self-care and avoidance of aggravating factors in the treatment of thoracic outlet syndrome?
Study Notes
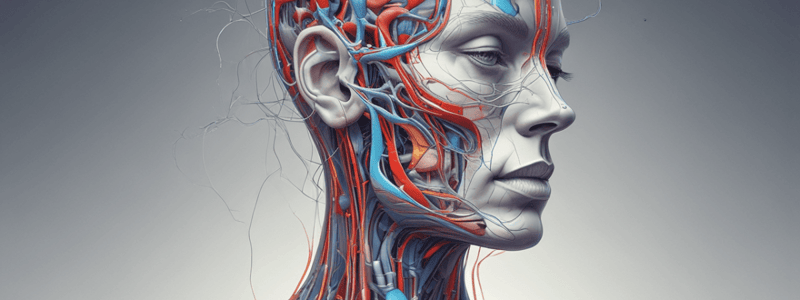
Trigeminal Neuralgia (Tic Douloureux)
- A disorder of the trigeminal nerve producing severe bouts of lancinating pain lasting several seconds to minutes
- Pain is distributed along one or more of the trigeminal nerve's sensory divisions, most commonly in the maxillary and less often the ophthalmic division
- The neuralgia is usually unilateral and commonly affects only one branch of the trigeminal nerve, but may affect both maxillary and mandibular divisions in some cases
Characteristics
- Bouts of pain may last a few seconds to several seconds, and may be longer
- Attacks may progress to several attacks a day, lasting days, weeks, months, or longer
- Some may have periods with no attacks (remission period)
- The neuralgia usually occurs in people between the ages of 50-70, but may also be seen in younger people with Multiple Sclerosis
Anatomy
- The trigeminal nerve is the largest of the cranial nerves and supplies sensory awareness to the face and head, and motor function to the muscles of mastication and the tensor tympani muscle
- The nerve exits the brainstem from the pons and its sensory information is transmitted back directly to the brainstem to sensory nuclei that are connected to the reticular formation, cerebellum, and thalamus
- The nerve passes through four foramen in the skull
- The afferent branches are separated into three divisions: Ophthalmic, Maxillary, and Mandibular
Signs and Symptoms
- There are generally no sensory alterations between attacks, but altered sensation to the face may be present during an attack
- Other symptoms during an attack may include:
- Spasm and locking of the muscles of mastication
- Loss of hearing due to temporary paralysis of the tensor tympani muscle
- Facial "tics" or grimacing in pain (AKA, "tic douloureux")
- Extreme antalgic expression, screaming, crying, debilitation
- Tearing of the eye if the ophthalmic division is affected
Causes
- The cause is generally uncertain or idiopathic
- Compression of the artery or vein "strangles" the nerve and damages the myelin sheath surrounding it, causing it to malfunction
- Contact with the artery or vein may cause malfunction as well
- Other causes include:
- Bone spurs at the foramina
- Tumors (identified with MRI)
- Multiple sclerosis; demyelination of the nerve followed by scarring (identified with MRI)
- TMJ imbalances
Triggers and Trigger Zone
- Attacks are generally triggered by touching a trigger zone or an activity involving the trigger zone
- The trigger zone includes the lips, face, or tongue
- Triggers include:
- Light touch
- Chewing
- Brushing teeth
- Washing face
- Sneezing
- Blowing the nose
- Talking
- A breeze
- Facial movements
- Sinus infection
- Tooth or gum infection
- Stress
- A combination of triggers
Assessment Case History
- General health (TMJ, Multiple sclerosis)
- Diagnosis by M.D.?
- Treatment and Results (medication, surgery)
- Location of pain (Most commonly maxillary or mandibular)
- Location of Trigger Zone (small area on face, cheek, tongue)
- Triggers (light touch, chewing, sneezing, washing face, etc.)
- Quality of pain (often described as the worst pain in the world, sharp, electrical, stabbing, lancinating, burning, hot poker)
- Duration of pain (usually 15-30 seconds, may last for a minute or two)
- Symptoms other than pain (facial "tic" or grimace, tearing of the eye, nausea, weight loss, depression, anxiety, and fear of next attack, suicidal tendencies)
Treatment and Contraindications
- The therapist must provide a safe treatment, minding all the contraindications and modifications that need to be made for a person with trigeminal neuralgia
- Client may be positioned in supine and/or side-lying on unaffected side
- Absolutely no treatment in prone
- Hydrotherapy may include heat for trigger points, but should not touch the face
- Massage may include visualizations, deep breathing, and progressive relaxation techniques
- The trigger zone must be avoided at all times during treatment
Medical Treatment
- Medications include painkillers and anti-seizure drugs
- Carbamazepine (a powerful anti-convulsent) is often the drug of choice, but liver and hematopoietic functions should be monitored
- If medication does not control the problem, surgery may be performed
Bell's Palsy
- Unilateral flaccid paralysis of the muscles of facial expression caused by a lesion of cranial nerve #7/facial nerve
- Idiopathic in 70% of cases, with spontaneous recovery in 70% of cases
- Affects 25 in 100,000 people each year
- Abrupt rapid onset, reaching maximum weakness within 48 hours
- Most often unilateral, but can present bilaterally in less than 1% of cases
- Palsy may result from partial compression or complete compression, leading to Wallerian degeneration (poorer prognosis)
- Can affect taste sensation, lacrimation, and salivary flow depending on lesion location
Anatomy
- Facial nerve arises from the pons, passes through the geniculate ganglion, and exits at the stylomastoid foramen
- Motor division passes through the osseous petrous canal of the temporal bone, where minor swelling can compress the nerve
- Five branches supply the face, including:
- Muscles of facial expression (smiling, frowning, etc.)
- Muscles of the eyes and forehead (except levator palpbrae superioris)
- Buccinator and muscles of upper lip
- Muscles of the lower lip and chin
- Muscles of the cheeks and nose
- Stapedius muscle of the eardrum
- Stylohyoid, platysma, and posterior digastric
Signs and Symptoms
- Mouth drooping on the affected side
- Difficulty chewing on the affected side
- Inability to wrinkle forehead or dilate nostril on the affected side
- Loss of lacrimation (tears) and salivation
- Decreased taste on anterior 2/3 of tongue
- Heightened sensitivity or distortion of sounds
- Pain, often localized to the mastoid area
- Sudden, unilateral palsy to one side of the face, which may be complete or partial flaccid paralysis
- Sagging of the face, deviating to the unaffected side (risk of contracture)
- Distortion of facial expressions, pulling towards the unaffected side
- Drooping eyelid, with inability to close the affected eye fully
Causes
- Compression from edema (pregnancy, middle ear infection, diabetes, hypertension)
- Tumour
- Trauma to face or head (birth trauma, blunt force trauma, stab wound, facial or dental surgery, concussion)
- Exposure to cold or chilling of the face
- Infection affecting the parotid gland (mumps)
- Middle ear infection
Assessment
- Case history: general health, pregnancy, onset, pain, doctor visits, diagnoses, lesion completeness, recent injury or surgery, exposure to cold, medications, steroids
- Testing:
- Eye closure: inability to close the affected eye, with eyeball rolling upward and inward
- Eyebrow raising: asymmetrical lifting and less forehead wrinkling on the affected side
- Smiling: drooping on the affected side and pulling towards the unaffected side
- Mouth movements: difficulty articulating certain words or sounds
Treatment
- Massage techniques:
- Neck and shoulder massage to reduce muscle tension and trigger points
- Facial stroking and running vibrations to relax facial muscles
- Treat unaffected side of the face first, supporting the affected side with a towel roll
- Pressure applied from the lateral side towards the midline to avoid tractioning on the nerve
- Light fingertip kneading and tapotement to affected muscles
- Facial exercises:
- Practice vowels and consonants (P, B, M, N)
- Raise eyebrows, smile, show teeth, whistle, and blow
- Imagine smelling something and scrunching the face
- Contraindications and precautions:
- Infection and injury of the eye
- Keep pressure and drag on flaccid muscles low
- Stabilize the head with pillows or towel rolls
- Avoid lying with face in face cradle due to flaccid paralysis
Remedial Exercise and Self-Care
- Practice facial exercises to promote recovery
- Protect the eye with an eye patch or sterile gauze
- Use artificial tears during the day and lubricating ointment at night
- Ensure good oral hygiene to prevent food from getting lodged between teeth and cheek on the affected side
Prognosis
- Typically, there is an 80% chance of recovery within 6 months
- Risks of non-recovery include:
- Age above 55
- Hypertension
- Complete facial paralysis
- Changes in tearing (crocodile tears – excessive tearing when salivary glands are stimulated during eating)
Thoracic Outlet Syndrome (TOS)
- A compression syndrome of the brachial plexus within the shoulder girdle
- Compression of the lower trunk of the brachial plexus (C8-T1), Subclavian artery, and in some cases the Subclavian Vein in the Thoracic Outlet
Thoracic Outlet Anatomy
- Extends from the cervical spine to the pectoralis minor muscle
- Located between the Scalene muscles, clavicle, and first rib
- Proximally, it is comprised of the interscalene triangle, formed by the anterior scalene muscle, middle scalene muscle, and the first rib
- The space may narrow due to:
- Scalene hypertonicity and trigger points
- Space-occupying structures (e.g., 7th cervical rib)
- Deep inhalation, which elevates the floor of the interscalene triangle
Compression Spaces
- Interscalene triangle: may narrow due to scalene hypertonicity and trigger points
- Costoclavicular space: formed by the clavicle anteriorly and the first rib posteromedially
- May narrow due to retraction of the shoulder, inspiration, and slouching forward
- Retropectoralis minor space: formed by the pectoralis minor muscle, coracoid process, and ribs 2-4
- May narrow due to shoulder abduction and external rotation, as well as retraction of the shoulder
Course of the Neurovascular Bundle
- The brachial plexus is made up of nerve roots from C5-T1, which innervates the arm
- Travels along with the Subclavian artery between the anterior and middle scalene
- Joined by the Subclavian Vein, becoming the neurovascular bundle, and travels deep to the clavicle and Pectoralis Minor
Signs and Symptoms
- Neurological symptoms:
- Numbness and/or tingling along the C8-T1 dermatomes
- Pain in the shoulder, upper limb, chest, neck, and head
- Muscle weakness and clumsiness in the hand
- Atrophy of the hypothenar eminence and interossei
- Vascular symptoms:
- Pallor in the hand
- Pain due to ischemia
- Cyanosis
- Distal coolness
- Venous distention
- Edema, especially upon waking
- Joint stiffness
Causes
- Compression of the neurovascular bundle by:
- Extra Cervical Rib (structural)
- Scalene hypertrophy from overuse, scar tissue, or trigger points
- Anatomically wide insertion of anterior or middle scalene on the first rib
- Brachial plexus piercing the anterior scalene muscle
- Structural bony abnormality of the clavicle and/or first rib
- Pec minor hypertrophy from repetitive use, scar tissue, or trigger points
- Trauma/Surgery to the neck or shoulder
- Respiratory pathologies (Asthma, Emphysema, Bronchitis)
- Edema (Pregnancy, lymphedema)
- Hyperkyphotic posture
Assessment
- Observation:
- Postural assessment (hyperkyphosis)
- Anterior head carriage, protracted scapulae, “slouchy shoulders”
- “Fullness” at supraclavicular fossa
- Atrophy of intrinsic hand muscles
- Swelling of the fingers or dorsum of hand
- Venous distention
- Skin/nail changes
- Palpation:
- Trigger points and tenderness in the scalenes, pec minor, and subclavius
- Coolness in the affected hand
- Edema in the dorsum of hand
- Testing:
- AF and PR ROM of C-spine and shoulder
- Myotomes and dermatomes
- Spurling’s to rule out possible nerve root compression
- Adson’s, Reverse Adson’s, Costoclavicular, and Wright’s Hyperabduction tests
Treatment
- Aims: relieve the compression site, identify and reduce contributors
- Techniques:
- Diaphragmatic breathing
- Fascial techniques to the upper chest, neck, and shoulder
- O&I, muscle stripping, and trigger point release to the scalenes, pec minor, and subclavius
- GTO, petrissage to the pectoralis major, SCM, upper trapezius, and posterior cervical paraspinals
- Rhythmic mobilizations to the scapulothoracic joint
- Joint play to the cervical spine, sternoclavicular, and GH joints
- Traction to the C-Spine
- PR ROM to the C-spine and Glenohumeral Joint
- Passive stretches to the muscles and joints of the forearm, wrist, and hand
- Strengthening to the interscapular muscles and grip muscles of the hand
- Lymphatic drainage to the arm if necessary
Contraindications and Precautions
- Refer immediately for medical attention if a thrombosis is suspected
- Avoid heavy or hot hydrotherapy and scalene stripping if the client has high blood pressure or a history of atherosclerosis
- Avoid frictions if the client is on anti-inflammatories
- Avoid trigger point release, deep petrissage, and deep fascial if the client is on analgesics
- Modify aggressive techniques where muscle, skin, or circulation is fragile
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers Trigeminal Neuralgia, a disorder of the trigeminal nerve that produces severe, lancinating pain. It's a common and severe neuralgia affecting females more than males.