Podcast
Questions and Answers
Trigeminal neuralgia is a specific type of what?
Trigeminal neuralgia is a specific type of what?
- Central nervous system disorder
- Brain tumor
- Spinal cord injury
- Peripheral nerve problem (correct)
Trigeminal neuralgia is caused by degeneration of or pressure on which of the following cranial nerves?
Trigeminal neuralgia is caused by degeneration of or pressure on which of the following cranial nerves?
- Cranial nerve VII
- Cranial nerve V (correct)
- Cranial nerve III
- Cranial nerve X
Trigeminal neuralgia is also known as?
Trigeminal neuralgia is also known as?
- Carpal Tunnel Syndrome
- Tic douloureux (correct)
- Bell's Palsy
- Sciatica
Which population is most commonly affected by trigeminal neuralgia?
Which population is most commonly affected by trigeminal neuralgia?
What type of pain is characteristic of trigeminal neuralgia?
What type of pain is characteristic of trigeminal neuralgia?
In trigeminal neuralgia, the pain radiates along branches of which cranial nerve?
In trigeminal neuralgia, the pain radiates along branches of which cranial nerve?
Which branches of the trigeminal nerve are typically involved in trigeminal neuralgia?
Which branches of the trigeminal nerve are typically involved in trigeminal neuralgia?
The pain associated with trigeminal neuralgia usually extends to what point on the face and head?
The pain associated with trigeminal neuralgia usually extends to what point on the face and head?
How long do the attacks of pain typically last in trigeminal neuralgia?
How long do the attacks of pain typically last in trigeminal neuralgia?
What is the typical pattern of pain laterality in trigeminal neuralgia?
What is the typical pattern of pain laterality in trigeminal neuralgia?
What are areas along the course of the nerve that may initiate pain in trigeminal neuralgia known as?
What are areas along the course of the nerve that may initiate pain in trigeminal neuralgia known as?
Which of the following is a common stimulus that can trigger pain in trigeminal neuralgia?
Which of the following is a common stimulus that can trigger pain in trigeminal neuralgia?
Which class of medications is commonly used to treat the pain of trigeminal neuralgia?
Which class of medications is commonly used to treat the pain of trigeminal neuralgia?
Which medication may be used alone or in combination with antiseizure medications for trigeminal neuralgia?
Which medication may be used alone or in combination with antiseizure medications for trigeminal neuralgia?
What substance may be injected into the peripheral branches of the trigeminal nerve to provide relief?
What substance may be injected into the peripheral branches of the trigeminal nerve to provide relief?
What intervention can provide permanent relief of pain in trigeminal neuralgia?
What intervention can provide permanent relief of pain in trigeminal neuralgia?
Why is it common for patients with trigeminal neuralgia to have difficulty eating?
Why is it common for patients with trigeminal neuralgia to have difficulty eating?
What is a common comfort measure for patients with trigeminal neuralgia
What is a common comfort measure for patients with trigeminal neuralgia
How long does an acute pain episode typically last in trigeminal neuralgia?
How long does an acute pain episode typically last in trigeminal neuralgia?
What is the typical pattern of pain onset and recurrence in trigeminal neuralgia?
What is the typical pattern of pain onset and recurrence in trigeminal neuralgia?
Bell's Palsy affects which cranial nerve?
Bell's Palsy affects which cranial nerve?
What is believed to be the cause of Bell's palsy?
What is believed to be the cause of Bell's palsy?
What sensation is typically experienced at the onset of Bell's palsy?
What sensation is typically experienced at the onset of Bell's palsy?
What is a common symptom of Bell's palsy regarding facial muscles?
What is a common symptom of Bell's palsy regarding facial muscles?
What causes an asymmetric appearance of the face in Bell's palsy?
What causes an asymmetric appearance of the face in Bell's palsy?
What is a common medical intervention for Bell's Palsy?
What is a common medical intervention for Bell's Palsy?
What is a crucial nursing intervention for Bell's palsy due to eyelid closure issues?
What is a crucial nursing intervention for Bell's palsy due to eyelid closure issues?
What is the average recovery time for Bell's Palsy?
What is the average recovery time for Bell's Palsy?
What is the first sign of improvement in Bell's Palsy?
What is the first sign of improvement in Bell's Palsy?
What is caused by infection or inflammation?
What is caused by infection or inflammation?
Which of these provides protection to the brain and spinal cord?
Which of these provides protection to the brain and spinal cord?
How can many infections of the nervous system be diagnosed?
How can many infections of the nervous system be diagnosed?
With an infection or inflammation, what can elevated body temperature indicate?
With an infection or inflammation, what can elevated body temperature indicate?
The removal of unwanted components from the patients blood serum is called?
The removal of unwanted components from the patients blood serum is called?
Maintaining respiratory function is crucial because the patients condition can rapidly detoriate into paralysis that affects the ?
Maintaining respiratory function is crucial because the patients condition can rapidly detoriate into paralysis that affects the ?
Meningitis is an acute infection of the?
Meningitis is an acute infection of the?
Flashcards
Trigeminal Neuralgia
Trigeminal Neuralgia
A peripheral nerve problem caused by deterioration or pressure on cranial nerve V. Also called tic douloureux.
Trigeminal Neuralgia Pain
Trigeminal Neuralgia Pain
Severe, stabbing facial pain lasting seconds to minutes, usually unilateral, along trigeminal nerve divisions.
Trigeminal Neuralgia Triggers
Trigeminal Neuralgia Triggers
Avoid stimulating trigger points: chewing, toothbrushing, wind on face, washing face, yawning, talking.
Medications for Trigeminal Neuralgia
Medications for Trigeminal Neuralgia
Signup and view all the flashcards
Bell's Palsy
Bell's Palsy
Signup and view all the flashcards
Bell's Palsy Symptoms
Bell's Palsy Symptoms
Signup and view all the flashcards
Bell's Palsy Treatments
Bell's Palsy Treatments
Signup and view all the flashcards
Nursing for Bell's Palsy
Nursing for Bell's Palsy
Signup and view all the flashcards
CNS Infections
CNS Infections
Signup and view all the flashcards
Meningitis
Meningitis
Signup and view all the flashcards
Meningitis Symptoms
Meningitis Symptoms
Signup and view all the flashcards
Meningitis Diagnosis
Meningitis Diagnosis
Signup and view all the flashcards
Meningitis Treatment
Meningitis Treatment
Signup and view all the flashcards
Nursing for Meningitis
Nursing for Meningitis
Signup and view all the flashcards
Encephalitis
Encephalitis
Signup and view all the flashcards
Encephalitis Symptoms
Encephalitis Symptoms
Signup and view all the flashcards
Encephalitis Diagnosis
Encephalitis Diagnosis
Signup and view all the flashcards
Encephalitis Treatment
Encephalitis Treatment
Signup and view all the flashcards
Guillain-Barré Syndrome (GBS)
Guillain-Barré Syndrome (GBS)
Signup and view all the flashcards
GBS Symptoms
GBS Symptoms
Signup and view all the flashcards
Diagnosing GBS
Diagnosing GBS
Signup and view all the flashcards
Treating GBS
Treating GBS
Signup and view all the flashcards
Nursing for GBS
Nursing for GBS
Signup and view all the flashcards
West Nile Virus Symptoms
West Nile Virus Symptoms
Signup and view all the flashcards
Diagnosing West Nile Virus
Diagnosing West Nile Virus
Signup and view all the flashcards
Treatment for West Nile Virus
Treatment for West Nile Virus
Signup and view all the flashcards
Brain Abscess
Brain Abscess
Signup and view all the flashcards
Symptoms of a Brain Abscess
Symptoms of a Brain Abscess
Signup and view all the flashcards
Treatment of Brain Abscess
Treatment of Brain Abscess
Signup and view all the flashcards
AIDS
AIDS
Signup and view all the flashcards
AIDS Neurologic Effects
AIDS Neurologic Effects
Signup and view all the flashcards
AIDS Treatment
AIDS Treatment
Signup and view all the flashcards
Nursing for AIDS
Nursing for AIDS
Signup and view all the flashcards
Primary Brain Tumors
Primary Brain Tumors
Signup and view all the flashcards
Secondary Brain Tumors
Secondary Brain Tumors
Signup and view all the flashcards
Brain Tumors
Brain Tumors
Signup and view all the flashcards
Brain Tumor Diagnosis
Brain Tumor Diagnosis
Signup and view all the flashcards
Brain Tumor Treatment
Brain Tumor Treatment
Signup and view all the flashcards
Brain Tumors
Brain Tumors
Signup and view all the flashcards
Study Notes
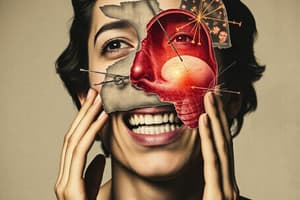
Trigeminal Neuralgia
- A specific peripheral nerve issue, also called tic douloureux.
- Cause is unknown, but related to degeneration or pressure on cranial nerve V (trigeminal nerve).
- More common in middle-aged to late adulthood, and slightly more prevalent in women.
- Pathophysiology is not fully understood.
Clinical Presentation of Trigeminal Neuralgia
- Excruciating, knifelike, or lightning-like pain affects the lips, gums, cheek, forehead, or side of the nose.
- Pain radiates along one or more of cranial nerve V's three divisions, which include motor and sensory branches.
- Sensory branches (maxillary and mandibular) are primarily affected in trigeminal neuralgia.
- Pain usually stops at the face and head midline, reflecting the tissue supplied by the affected nerve.
- Attacks are brief, from seconds up to three minutes, and usually only affect one side.
- Recurrences are unpredictable, from multiple times a day to weeks or months apart.
- Trigger points along the nerve course can initiate pain with even slight stimulation.
- Chewing, toothbrushing, hot or cold air, face washing, yawning, or talking can trigger pain.
Medical Management of Trigeminal Neuralgia
- Antiseizure drugs such as carbamazepine (Tegretol), phenytoin, valproate, gabapentin, oxcarbazepine (Trileptal), lamotrigine (Lamictal), and topiramate may alleviate pain
- Muscle relaxants like baclofen (Gablofen) can be used with or instead of antiseizure drugs.
- Absolute alcohol injected into trigeminal nerve branches provides relief by damaging nerves and blocking pain signals for weeks to months.
- Biofeedback, acupuncture, and megavitamins have been used as therapies.
- Surgical options, including sensory root resection (traditional), microvascular decompression, and Gamma Knife radiosurgery, exist for permanent pain relief.
Nursing Interventions for Trigeminal Neuralgia
- Patients may have difficulty eating, and be undernourished and dehydrated.
- Patients may have neglected washing, shaving, or combing their hair.
- Oral hygiene is often neglected
- Comfort measures include a draft-free room and moderate temperature should be provided.
- Touching a patient's face should be avoided
- Avoid urging patients to wash/shave the affected area or comb their hair during attacks.
- Emphasize hygiene, nutrition, and oral care while also conveying an understanding if patients have neglected this in the past.
- Use lukewarm water, soft cloths, and cotton with solutions that will not require the use of water for cleaning the face
- A warm mouthwash and soft toothbrush can help promote oral care.
- Hygiene instruction is best provided when analgesia is at its peak.
- It is best to allow patients to perform their own care if they fear inadvertent injury at the hands of someone else.
- The patient should avoid hot/cold fluids, which trigger pain.
- Puree the patients food and ensure it is lukewarm, suggesting that they use a straw.
Trigeminal Neuralgia Prognosis
- Acute pain lasts seconds to minutes but is excruciating.
- Pain onset is unpredictable, occurring anytime and potentially recurring many times daily for weeks.
- Surgery is often required for permanent pain relief.
Bells Palsy
- Also known as peripheral facial paralysis, is thought to be caused by inflammation involving cranial nerve VII (facial nerve).
- Inflammation can occur anywhere from the brain nucleus to the nerve's periphery
- Reactivated herpes simplex virus (HSV) is believed to be a trigger in many instances, though the exact cause is unknown
- Reactivated HSV results in inflammation, edema, ischemia and demyelination of the facial nerve, causing pain and motor/sensory disturbances
- Any of the facial nerve's three branches may be affected.
Clinical Presentation of Bells Palsy
- Abrupt onset of numbness, stiffness, or a drawing sensation in the face.
- Facial muscle weakness on one side results in flaccidity, causing inability to wrinkle the forehead, close the eyelid, pucker lips, smile, frown, whistle, or retract the mouth
- The face appears asymmetrical with a drooping mouth and cheek, and can result in loss of taste, altered chewing ability, reduction of saliva, and pain/ringing in the affected ear.
Medical Management of Bells Palsy
- There is no specific therapy for Bell's Palsy
- Electrical stimulation or warm, moist heat to help maintain muscle tone and prevent atrophy.
- Corticosteroids (especially prednisone) should be started immediately, and tapered off over two weeks as the patient improves.
- Acyclovir (Zovirax), alone or with prednisone, is used due to HSV's implication in approximately 70% of cases.
Nursing Interventions for Bells Palsy
- When the eyelid does not close, it is important to protect the eye.
- Eye shields at night prevent cornea dryness and damage.
- Artificial tears may be prescribed, and should be administered as directed.
- Massaging the affected area may be recommended.
- Active facial exercises for 5 minutes, three times daily, can include wrinkling the brow, closing the eyes, and puffing cheeks.
Bells Palsy Prognosis
- Most patients fully recover within 3-6 months, although recovery can take up to a year.
- The degree of the nerve damage indicates recovery length.
- Recovery of taste within the first week signals a good chance of motor function recovery.
- Paralysis that remains incomplete within 5-7 days is another favorable sign.
- Permanent paralysis occurs in a few cases, and the disorder rarely recurs.
Infection and Inflammation Etiology and Pathophysiology
- Infection or inflammation often interferes with function.
- Meningitis, encephalitis, brain abscess, GBS, herpes zoster, neurosyphilis, poliomyelitis, and AIDS are a few conditions that can affect nerve function
- The brain and spinal cord are usually protected by the skull and vertebral column, meninges, and blood-brain barrier.
- Infective agents may enter the CNS via air sinuses, the middle ear, or blood.
- Injuries and treatments disrupting the dura (basilar skull fractures, missile injuries, neurosurgical procedures) increase infection risk.
- Meningitis can be caused by bacteria, viruses, fungi, parasites, or toxins, and is classified as acute, subacute, or chronic.
- Pathophysiology, clinical presentation, and management vary based on the infecting microorganism.
- GBS, meningitis, encephalitis, brain abscess, and AIDS are just some conditions discussed
- Various organisms and toxins can affect the nervous system.
- Toxins reach the nervous system from surrounding bones, blood, or lymph, and meningitis can result from invasive procedures like surgery.
Assessement for Infection and Inflammation
-
Subjective data includes a history of infection (such as upper respiratory) and discomfort (headache/stiff neck).
-
Objective data includes, behavioral signs (discomfort or disorientation), inability to perform ADLs, fever, vomiting, abnormal CT results, seizures, altered respiratory patterns, tachycardia, and meningeal irritation.
-
Important to assess LOC and orientation.
Diagnostic Tests, Interventions and Patient Problems for Infections and Inflammation
- Many nervous system infections are diagnosed via CSF examination.
- CT scans and EEGs can also be conducted.
- Patient problems for elevated boy temperature include assess temperature q2 hours and administer cooling measures.
- Problems for recent onset of confusion include introducing self to the patient, relating time and date and using short, simple sentences.
Education for patients with Infection includes
- Teaching about treatments, disease and expected outcomes.
Guillain-Barre syndrome (GBS)/Polyneuritis Etiology
- Acute inflammatory polyradiculopathy or postinfectious polyneuritis, known as Guillain-Barré syndrome (GBS).
- Acute, rapidly progressing, potentially fatal polyneuritis that causes widespread inflammation and demyelination in the peripheral nervous system.
- While the cause is unknown, the condition is believed to be an autoimmune reaction affecting the peripheral nerves.
- GBS is most often linked to respiratory or gastrointestinal viral infections
- Less commonly seen after viral immunizations, surgery, or Epstein-Barr virus.
- PNS consists of cranial nerves, 31 spinal nerve pairs, plexuses, and ganglia; neurons comprise axons.
- Axons transmit the nerve impulses and are insulated in segments called the myelin sheath, made from the Schwann cells.
- In GBS, antibodies target Schwann cells, breaking down the myelin sheath (demyelination) and inflaming the nerve.
- Signs of muscle weakness, tingling, and numbness start as nerve conduction is interrupted.
- Symptoms typically begin in the legs or feet and progress upward, due to the long nerve distance to the legs.
- Demyelination is self-limiting, and once stopped, Schwann cells rebuild the insulation
- Remyelination and recovery occur in reverse, starting at the top and progressing downward.
Clinical Presentation of GBS
- The pattern of weakness onset/symptom progression varies and may halt at any point.
- Breathing, swallowing or speaking may become difficult if cranial nerves are involved
- Symmetric muscle weakness and lower motor neuron paralysis is present
- Paralysis usually starts in the lower extremities and moves up to include the thorax, the upper extremities, and the face.
- If the intercostal muscles are affected, respiratory failure may occur.
- Autonomic nervous system effects may cause fluctuating blood pressure.
Diagnostic Tests for GBS
- GBS diagnosis involves ruling out other conditions and identifying characteristic muscle weakness.
- A CT scan may rule out tumors/stroke. Respiratory status changes aid in diagnosis.
- Lumbar puncture is performed.
- CSF of GBS patients typically has elevated protein levels.
- A nerve conduction velocity study may be performed to test for slow impulse transmission.
- Electromyography/nerve conduction studies are markedly abnormal in a recent infection
Medical Management of GBS
- Hospitalization is vital if GBS is suspected as the patient can rapidly deteriorate into paralysis affecting the respiratory muscles
- Adrenocortical steroids treat GBS.
- Therapeutic plasmapheresis (removal of unwanted components from the patient's blood) during the first 2 weeks reduces the severity and length of symptoms
- IV immune globulin (Sandoglobulin) is an alternate to plasmapheresis, requiring patients to be hydrated and have adequate renal function
- Respiratory failure requires mechanical ventilation and tracheostomy. ABG monitoring and pulmonary function tests assess respiratory status.
- Gastrostomy tubes may be placed for severe paralysis/long recovery periods to provide adequate nourishment
Nursing Interventions for GBS
- Closely monitor the patient's respiratory function. Provide reassurance if they require mechanical ventilation, as cognition is not affected
- The patient may need to be fed intravenously or via nasogastric tube. Prevent complications like contractures, pressure ulcers, and ROM loss to allow complete recovery.
- Early physical therapy can prevent contractures. Administer neuropathic pain medication, such as gabapentin or amitriptyline.
- Assess the patient's vital signs/motor strength frequently; monitor for signs of hypoxia
Prognosis of GBS
- 15% of patients experience long term weakness and report fatigue.
- The recovery period ranges from weeks to years.
- Some patients experience a degree of permanent neurologic deficit.
- Disease recovery typically mirrors how the paralysis (or loss of strength), occurred.
- Recovery is directly correlated with the quality of support received during the acute phase of the illness.
Infection Meningitis Etiology
- Acute meningeal infection caused by bacteria (pneumococci, meningococci, N. meningitidis, staphylococci, streptococci, H. influenzae), viruses, fungi, parasites, or toxins.
- Bacterial infection leads to inflammation in the pia mater/pus in the arachnoid space, raising protein/WBC levels in the CSF, possibly harming nervous tissue.
- Can be septic (bacterial) or aseptic (viral) and is often seen during fall/winter when upper respiratory infections are common.
- Key changes include engorgement of meningeal vessels (hyperemia), brain tissue edema, increased ICP, inflammatory reaction/WBC entering subarachnoid spaces, and hydrocephalus caused by exudate blocking infant ventricles.
Clinical Manifestations of Meningitis
- Kernig’s Sign, defined as an inability to extend the leg completely without pain, is an abnormal sign of meningitis
- Brudzinski Sign, defined as flexion of the hip and knee caused from neck flexion, is an abnormal sign of meningitis
- Meningitis onset is usually sudden, marked by severe headache, neck stiffness, irritability, malaise, and restlessness.
- Other symptoms include vomiting/nausea, delirium, increased temperature, pulse and respiratory rate.
Diagnostics Tests Used For Meningitis
- CT scan of the head to rule out increased ICP from meningitis
- Lumbar puncture to draw CSF, sent to the lab to identify the pathogen causing meningitis.
- If ICP is increased, do not perform a lumbar puncture.
Medical Management For Meningitis
- Rapid diagnosis and treatment are essential for bacterial meningitis patients.
- When meningitis is suspected, collect cultures to confirm the diagnosis. Antibiotics are given for over two weeks.
- Ampicillin, penicillin, vancomycin, piperacillin, and third-generation cephalosporins (ceftriaxone/cefotaxime) are medication options when treating bacterial meningitis.
- IV corticosteroids reduce ICP
- Anticonvulsants prevent any seizures that may be associated with an infection of the meninges
- Viral meningitis is managed with supportive therapy like maintaining the patient on bed rest to minimize spread, fluid and electrolyte balance management, and supportive comfort measures.
Nursing Interventions For Meningitis
- Respiratory isolation is necessary until the pathogen is no longer in the nasopharynx, and is usually accomplished in 24 hours with antibiotics.
- Supportive care should be given to critically ill patients that may be irritable, disoriented and unable to take fluids.
- Dehydration is very common, and IV fluid replacement is generally necessary.
- Sensory stimulation may cause a seizure so patients should be kept in a darkened, quiet room.
- It is important to manage a patients fever because it increases the frequency of seizures, as well as cerebral edema formation
- Neurologic damage may occur, with acetaminophen as a medication to reduce fever
- In some cases, the use of a cooling blanket is necessary because patients may not respond to acetaminophen
- Recommended treatment plans may include providing prophylactic antibiotic therapy for the patient's family, to ensure causative bacteria that may have colonized in the nasopharynx are eradicated.
- Pneumococcal vaccination should be given to adults 65 and older and for high risk adults, as well as an MCV4 Booster at 16 for those that have gotten their first dose at age 11-12 years old to protect them from N. meningitidis.
- An MCV4 booster can be given at the ages of 16-18 years old if they received their first dose between 13-15 years old and is not necessary if they already received their dose at 16 years old or older.
- The H. influenzae vaccine significantly decreased the amount of meningitis that is caused by this particular organism in children.
Prognosis of Meningitis
- If the infection is diagnosed early, it is a good prognosis
- If severe meningitis is left intreated however, it may result in residual neurologic damage, or even death.
Encephalitis Etiology and Pathophysiology
- Encephalitis is usually caused by a viral infection, which results in acute inflammation in the brain.
- Epidemic Encephalitis is transmitted via ticks, mosquitos.
- Non-endemic encephalitis may present as a complication from the chickenpox, mumps or measles.
- Encephalitis is a fatal infection, which can be commonly caused by HSV, or cytomegalovirus (mainly for those who have AIDS).
Clinical Manifestations For Encephalitis
- Signs will resemble those of meningitis, but the symptoms may have a gradual onset (HA, fever, seizures, and change in LOC).
Diagnosis of Encephalitis
- Early diagnosis and treatment of viral encephalitis are essential for favorable outcomes, which can be done via MRI and PET.
Medical Management For Encephalitis
- Management is supportive (focus on cerebral edema and prevention of seizures).
- Control cerebral edema by using diuretics (mannitol) and corticosteroids (dexamethasone).
- Patients develop diffuse nerve cell damage, glial cell infiltration, and cerebral edema.
- Symptoms and sequelae in the population include mental deterioration, personality changes, memory loss, and hemiparesis.
- Anti virals (acycolvir and vidarabine have been used to try and aid in infection)
West Nile Virus Etiology and Pathophysiology
- WNV is commonly found in humans, birds, and other vertebrates in Africa, Eastern Europe, western Asia, and the Middle East but was not documented in the United States until 1999.
- The virus can infect humans, birds, mosquitoes, horses, and some other animals.
- The rate of transmission is through a female mosquito bite, after feeding on an infected bird, and incubating between 2-14 days in the human.
Clinical Manifestations Of West Nile Virus
- Flu like symptoms such as fever, HA, back pain, muscle fatigue lasting a few days.
- Some patients will get meningitis characterized by sudden HA, chills, and neck pain.
- Some patients get encephalitis that has severe fever, altered LOC, disorientation, behavioral and speech disturbances, hemiparesis, seizures, and coma.
Diagnostics of West Nile Virus
- Testing of blood and CSF that uses the immunoblot M (IgM), antibody, captured enzyme linked immunosorbent assay (ELISA).
- The test may not be positive until symptoms first occur.
- False positives may result from recent vaccinations (yellow fever/ Japanese)
Patient Teaching and Education Related to West Nile Virus
- WNV is not transmitted casually. WNV is only transmitted through blood to blood from organ transplantation, transfusions, breastfeeding, and pregnancy.
- Insect repellents should be choose when outside.
- Clothing should be sprayed with DEET insecticide for protection. Take necessary precaution between April and October.
- DEET has been tested and proved safe as an insecticide but should be used in moderation with children younger than 2 months with concentrations of 10-35%.
Medical Management
- Focuses on managing symptoms and supportive care.
- Intravenous fluids, airway management, respiratory support, prevention of any infection, interferon alfa-2b, steroids, anti-seizures medications, and osmotic diuretic medications may be needed for aggressive cases.
Brain Abscess
- An accumulation of pus forms within the brain tissue from a local or systemic infection, most commonly caused from ear, tooth, mastoid, and sinus infections.
- Other causes of a brain abscess are septic venous thrombosis, pulmonary infection, infective endocarditis, skull fracture, and a nonsterile neurologic procedure.
- Streptococci and staphylococci are the primary infective organisms.
Manifestations of A Brain Abscess
- Headache and fever, as well as increased ICP (drowsiness, confusion, seizures).
- Focal symptoms reflect the abscess location.
- Temporal lobe abscesses result in visual field deficits or psychomotor seizures.
- Occipital abscesses can affect visual impairment and hallucinations.
Medical Management of A Brain Abscess
- The primary medical plan relies on Antimicrobial therapy
- All other signs and symptoms are to be treated supportively.
- Removal is needed if drug therapy is ineffective, or the abscess is encapsulated.
Nursing Interventions of A Brain Abscess
- Treat the same as that of a patient with meningitis, or presents with increased ICP
Prognosis for A Brain Abscess
- If Left Intreated, nearly 100% will be fatal in mortality rate with 30% encountering seizures.
Acquired Immunodeficiency Syndrome (AIDS)
- AIDS is the late or terminal stage of HIV infection, impacting the nervous system in 80% of patients.
- Neurologic signs/symptoms stem from HIV infection or associated infections.
- Meningitis, herpes simplex and cytomegalovirus, toxoplasmosis, and cryptococcal meningitis are some of these infections.
Clinical Manifestations of AIDS
- Neurologic problems affect 90% of those infected, including neuropathies, headaches, aseptic meningitis, cranial nerve dysfunction, and muscle diseases.
- Symptoms result from HIV or antiretroviral medication side effects.
- Advanced HIV/AIDS patients may have dementia complex (ADC), which causes difficulty concentrative and or remembering, progressing towards cognitive and or generalized deficiencies in intellect, awareness, and reasoning.
- Malignant lymphomas of the central nervous system can develop.
Diagnostic Tests for AIDS
- Diagnostics include serologic tests, CSF analysis via puncture, CT scan, and MRI, as well as a cerebral biopsy if needed.
Medical Management for AIDS
- Aims toward problems that are neurological.
- antivirals, antifungals, and antibacterials are commonly used as treatment options for the infection.
- In experimental therapy, radiation has been used for brain infections. Experimental therapies have consisted of DexFerrum.
- If patients is in shock they will need to be trated with electrolyte volume expanders. With mortality still remaining high in aggressive therapies, diazepam, phenytoin, and Fosphenyton still are needed to be used while seizures do occur.
Neurological Interventions of AIDS in the brain
- Because the patient may need to be re-orientated often due to disorientation, it is important to keep safety measures in place
- Side rails will need to be used for the event a seizure occurs
Etiology of Brain Tumors
- May be a primary source or metastatic.
- Each type can impact other structures and all parts of the brain.
- While the direct cause is unknown, tumors can be a result of genetic mutation with 150 different types of brain tumors.
Assessment of Brain Tumors
- Changes in sensation or the understanding the diagnosis. The patient may also be experiencing visual changes, or changes in personality.
- Tumor in the temporal lobe may cause the patient to complain of new odors.
- Headaches tend to be more prevalent in the morning
- Loss of balance/ dizziness might be present
- Vision changes/paresis
- Seizures could be a new incident sign
- Changes or cognitive memory and speech skills.
Objective Data of Brain Tumors
- Includes levels of the patients alertness, and the level, and their ability to be conscious, as well as their levels of orientation.
- Assess how pupil respond and their equality
- Seizures are likely
- In some pateints, the first sign of a brain is new onset seizures.
Diagnostics Of Brain Tumor
- The direct procedure for diagnosing a brain tumor is a CT Scan
- MRI, EEG, are testing methods also used with testing for brain scans.
Medical Management for Brain Tumors
- Involves surgical removal
- Chemotherapy with the aid of radiation
- Blood/ Brain barrier hinders effectiveness of chemotherapy used as adjuvant.
Surgery for Brain Tumors
- In Surgery
- Surgeons make an incision through to the cranium (craniotomy.) where the bone is preserved for possible need in the future
- Tissue sample are needed for diagnostic purposes. As a result of diagnostic measures surgeons get the necessary sample by drilling the tissue through a small incision (stereotactic biopsy).
- Computer aided navigation has increased and resulted in an increased rate of success amongst surgeons to guide them while performing such procedures
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.