Podcast
Questions and Answers
Which symptom is NOT associated with the active stage of traumatic ossification?
Which symptom is NOT associated with the active stage of traumatic ossification?
- Decreased range of movement
- Swelling
- Pain
- Circumscribed shadow of calcification (correct)
What is a treatment strategy for the active stage of traumatic ossification?
What is a treatment strategy for the active stage of traumatic ossification?
- Early reduction of fracture
- Immediate excision of calcified tissue
- Avoid passive movement after plaster removal
- Encourage graduated active exercises (correct)
Which of the following is NOT part of the management for acute ischemia?
Which of the following is NOT part of the management for acute ischemia?
- Wait for spontaneous recovery (correct)
- Suture torn vessels
- Explore vessels surgically if no improvement
- Remove tight bandages
What is the earliest and most objective sign of compartment syndrome?
What is the earliest and most objective sign of compartment syndrome?
Which of the following is a component of the 5Ps of compartment syndrome?
Which of the following is a component of the 5Ps of compartment syndrome?
What might be done if a vessel is thrombosed during management of acute ischemia?
What might be done if a vessel is thrombosed during management of acute ischemia?
During which stage of traumatic ossification do patients still experience local heat?
During which stage of traumatic ossification do patients still experience local heat?
What is the recommended management for vasospasm in acute ischemia?
What is the recommended management for vasospasm in acute ischemia?
What is the classic clinical finding of compartment syndrome?
What is the classic clinical finding of compartment syndrome?
Which of the following is NOT a recommended early treatment for compartment syndrome?
Which of the following is NOT a recommended early treatment for compartment syndrome?
What is a primary characteristic of Volkmann's ischaemic contracture?
What is a primary characteristic of Volkmann's ischaemic contracture?
What is a crucial preventive measure against Volkmann’s ischaemic contracture?
What is a crucial preventive measure against Volkmann’s ischaemic contracture?
Which method is included in the non-operative treatment for Volkmann's ischaemic contracture?
Which method is included in the non-operative treatment for Volkmann's ischaemic contracture?
Which nerve injury type is characterized by complete loss of nerve function?
Which nerve injury type is characterized by complete loss of nerve function?
What is the recommended treatment approach for carpal tunnel syndrome following a Colles' fracture?
What is the recommended treatment approach for carpal tunnel syndrome following a Colles' fracture?
Which treatment for Volkmann's ischaemic contracture may involve excision of necrotic muscle?
Which treatment for Volkmann's ischaemic contracture may involve excision of necrotic muscle?
Which of the following is a general complication of fractures?
Which of the following is a general complication of fractures?
What type of local complication is caused by rib fractures penetrating the lung?
What type of local complication is caused by rib fractures penetrating the lung?
Which of the following is NOT considered a late complication of fractures?
Which of the following is NOT considered a late complication of fractures?
What complication is associated with prolonged recumbency following a fracture?
What complication is associated with prolonged recumbency following a fracture?
Which of the following describes myositis ossificans?
Which of the following describes myositis ossificans?
Which of the following represents a respiratory complication that can arise from fractures?
Which of the following represents a respiratory complication that can arise from fractures?
What is the primary mechanism that leads to traumatic myositis ossificans?
What is the primary mechanism that leads to traumatic myositis ossificans?
Which complication would be classified as an urgent local complication?
Which complication would be classified as an urgent local complication?
What characterizes neuroapraxia?
What characterizes neuroapraxia?
What is the most accurate outcome for axonotmesis within six months?
What is the most accurate outcome for axonotmesis within six months?
Which injury is most likely to result in a claw hand?
Which injury is most likely to result in a claw hand?
Which of the following is NOT a common complication of joint injury?
Which of the following is NOT a common complication of joint injury?
What is the potential outcome of reflex sympathetic dystrophy?
What is the potential outcome of reflex sympathetic dystrophy?
What is a primary cause of post-traumatic arthritis?
What is a primary cause of post-traumatic arthritis?
Which treatment is NOT typically associated with reflex sympathetic dystrophy?
Which treatment is NOT typically associated with reflex sympathetic dystrophy?
What is a key symptom of Sudeck's osteodystrophy?
What is a key symptom of Sudeck's osteodystrophy?
What is the primary cause of avascular necrosis (AVN)?
What is the primary cause of avascular necrosis (AVN)?
Which complication involves healing that takes longer than the typical time frame for a bone injury?
Which complication involves healing that takes longer than the typical time frame for a bone injury?
What term describes a fracture that has healed in a non-anatomical position, potentially causing deformities?
What term describes a fracture that has healed in a non-anatomical position, potentially causing deformities?
What is a potential treatment option for non-union fractures?
What is a potential treatment option for non-union fractures?
Which local cause is NOT associated with delayed union and non-union?
Which local cause is NOT associated with delayed union and non-union?
Flashcards are hidden until you start studying
Study Notes
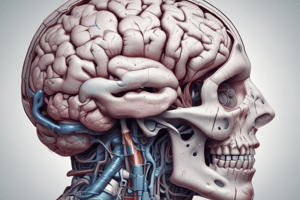
Traumatic Ossification (Myositis Ossificans)
- Calcification and ossification outside the skeleton causing joint movement restriction
- Can involve lacerated muscle, torn capsule, fascia, tendon, and periosteum
- Frequent after elbow and hip injuries, but can occur at other sites
- Predisposing factors: delayed reduction, massage, and passive exercises
- Pathogenesis: osteoblasts from injured periosteum migrating to form bone in muscle hematoma, metaplasia of fibroblasts to osteoblasts
Traumatic Ossification Stages
- Active stage: pain, swelling, local heat, decreased joint range of motion, cloudy shadow of calcification on X-ray
- Quiescent stage: pain and heat subside, swelling rare, joint stiffness persists, circumscribed and denser calcification shadow on X-ray
Traumatic Ossification Treatment
- Prophylactic: early fracture and dislocation reduction, immobilization, avoiding massage and passive movement after plaster removal
- Curative: active exercises after rest in active stage, excision in quiescent stage (aware of recurrence tendency), vascular injuries
Acute Ischemia
- Compartment syndrome: raised pressure within a closed space, potential for irreversible tissue damage
- Diagnosis: tense compartment (earliest and most objective sign), 5 Ps (pain, parathesia, pallor, paralysis, and pulselessness)
Acute Ischemia Management
- Surgical emergency, measures taken until blood flow restored: removal of tight bandages/plaster, fracture reduction if compressing artery, vessel exploration by urgent operation if no improvement within 30 minutes
Compartment Syndrome
- Early detection and treatment are essential
- Treatment: removal of constrictive dressings and casts, avoiding joint flexion, fracture reduction, elevation of limb
- Operative treatment: fasciotomy (decompression by opening threatened compartments)
Volkmann's Ischemic Contracture
- Massive forearm muscle infarction leading to fibrosis and permanent muscle shortening
- Clinically: wrist flexion, interphalangeal joint flexion, metacarpophalangeal joint extension, muscle atrophy, ischemic neuritis with sensory loss along median nerve distribution, trophic changes in fingers
- Contracture: flexors are short, fingers flex when wrist dorsiflexed and cannot passively extend, fingers can be passively extended when wrist flexed
Volkmann's Ischemic Contracture Prevention
- Early fracture reduction around the elbow, avoiding acute elbow flexion after supracondylar fracture reduction, avoiding tight bandages and casts, treating ischemia and performing fasciotomy
Volkmann's Ischemic Contracture Treatment
- Non-operative: gradual stretching with splint or wedged plaster cast in recent mild cases
- Operative: muscle slide operation, carpectomy, excision of necrotic muscle and transfer of healthy muscle tendon in selected cases
Nerve Injuries
- Types: neurapraxia, axontemesis, neurotemesis
- Common sites: carpal tunnel syndrome in Colles' fracture
- Neuroapraxia: physiologic interruption of nerve function, recovery in minutes to weeks
- Axonotemesis: cut nerve axon with intact sheath, complete recovery within 6 months
- Neurotemesis: cut nerve axon and sheath, bad prognosis
Nerve Injury Treatment
- Simple fractures with neurapraxia or axontemesis: spontaneous recovery
- Open fractures with neurotemesis: repair
Common Nerve Injuries and Their Effects
- Axillary nerve: shoulder dislocation, deltoid paralysis
- Radial nerve: humerus fracture, wrist drop
- Median nerve: supracondylar humerus fracture in children, pointing finger
- Ulnar nerve: medial epicondyle humerus fracture, claw hand
- Sciatic nerve: post-hip dislocation, foot drop
- Common peroneal nerve: knee dislocation, neck of fibula fracture, foot drop
Joint Complications
- Sprain, dislocation, subluxation, joint stiffness, effusion (traumatic synovitis), hemoarthrosis, septic arthritis, Sudeck's osteodystrophy, post-traumatic arthritis
Post-Traumatic Joint Stiffness
- Causes: adhesions (periarticular and intra-articular), traumatic ossification (myositis ossificans), Sudeck's osteodystrophy, osteoarthritis (late after many years), malunion, bone block
Reflex Sympathetic Dystrophy (Sudeck's Atrophy)
- Pain, swelling, osteoporosis, and stiffness of hand and foot in wrist and ankle fractures
- Etiology unknown, potentially due to disuse atrophy or over sympathetic activity
- Often a neurotic female, more common in wrist and ankle fractures
- Characterized by severe pain and stiffness, local vasomotor symptoms (discoloration, thinning, and excessive perspiration)
- X-ray: patchy rarefaction of bone
Reflex Sympathetic Dystrophy Treatment
- Physiotherapy: graduated exercises and paraffin baths
- Analgesics, TENS, sympathetic block, and sympathectomy
Post-Traumatic Arthritis
- Causes: joint incongruity after intraarticular fracture, avascular bone necrosis, malunited fractures
Bone Complications
- Avascular necrosis, non-union, malunion, delayed union, growth arrest, bone shortening, epiphyseal injuries, osteomyelitis
Avascular Bone Necrosis (AVN)
- Bone necrosis due to interruption of blood supply after fracture or dislocation injury
- Site: head of femur (femoral neck fracture, hip dislocation), scaphoid, talus
- Clinical presentation: late pain and malunion
Vulnerable Sites of AVN
- Head of femur, scaphoid, talus, knee (condyles and tibial plateau), humeral head, radial head, and lunate bone
Bone Healing Complications
- Delayed union: healing takes longer than average for a given bone injury
- Non-union: arrest of healing process, sclerosis at fracture ends, fracture does not unite, fibrous union with pseudoarthrosis
Fracture Healing Time Frame
- Clinical union: upper limb 3-4 weeks, lower limb 6-8 weeks in children, upper limb 6-8 weeks, lower limb 12-16 weeks in adults
- Radiological union: bridging callus formation and remodeling
Types of Non-union
- Atrophic: narrow fracture gap, sclerotic ends, minimal callus formation
- Hypertrophic: wide fracture gap, large callus formation, no bridging callus
Delayed Union and Non-union Local Causes
- Infection, inadequate blood supply, inadequate immobilization, distraction of fragments, interposition of soft tissue, severe soft tissue damage, avascular necrosis
###Delayed Union and Non-union Clinical Presentation
- Pain, swelling, abnormal movement
Delayed Union Treatment
- Prolonged immobilization, adequate fixation, bone graft for significant bone loss
Non-union Treatment
- Internal fixation, bone graft
Malunion
- Fracture healed in non-anatomical position
- Can cause angular deformity, rotational deformity, limb shortening
- Example: cubitus varus after supracondylar humerus fracture
- Treatment: osteotomy
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.