Podcast
Questions and Answers
What is the primary reason for prioritizing trauma evaluation?
What is the primary reason for prioritizing trauma evaluation?
- Saving life (correct)
- Identifying the type of fracture
- Prescribing medications
- Performing surgery
Which of the following is NOT part of the trauma ABCDE assessment?
Which of the following is NOT part of the trauma ABCDE assessment?
- Breathing
- Diagnosis (correct)
- Circulation
- Exposure
Which tissue is primarily responsible for providing a barrier against infection?
Which tissue is primarily responsible for providing a barrier against infection?
- Periosteum
- Bone
- Muscle
- Skin (correct)
What type of fracture is characterized by a break that does not fully penetrate the bone?
What type of fracture is characterized by a break that does not fully penetrate the bone?
What is a key finding in a fracture diagnosis?
What is a key finding in a fracture diagnosis?
Which artery system provides a blood supply to the outer third of the bone?
Which artery system provides a blood supply to the outer third of the bone?
Which type of fracture is often associated with a fragment of bone being pulled away by muscle or tendon?
Which type of fracture is often associated with a fragment of bone being pulled away by muscle or tendon?
What imaging technique is typically used for diagnosing fractures?
What imaging technique is typically used for diagnosing fractures?
What characteristic is least likely to indicate a fracture?
What characteristic is least likely to indicate a fracture?
An open fracture is defined by which of the following characteristics?
An open fracture is defined by which of the following characteristics?
What is the typical duration of the remodeling phase during fracture healing?
What is the typical duration of the remodeling phase during fracture healing?
Which factor is known to inhibit bone formation during fracture healing?
Which factor is known to inhibit bone formation during fracture healing?
What characterizes a 2nd degree/grade muscle strain?
What characterizes a 2nd degree/grade muscle strain?
Which type of hematoma is formed due to a direct blow on the muscle?
Which type of hematoma is formed due to a direct blow on the muscle?
In which grade of soft tissue injury is there significant instability due to complete rupture?
In which grade of soft tissue injury is there significant instability due to complete rupture?
What typically contributes to swelling in an intramuscular hematoma?
What typically contributes to swelling in an intramuscular hematoma?
Which of the following symptoms is not associated with ligament injuries?
Which of the following symptoms is not associated with ligament injuries?
What is a common symptom of a 1st degree muscle strain?
What is a common symptom of a 1st degree muscle strain?
Which of the following factors does not affect fracture healing?
Which of the following factors does not affect fracture healing?
In 3rd degree muscle strains, what happens to the muscle?
In 3rd degree muscle strains, what happens to the muscle?
What is the recommended antibiotic treatment for a contaminated type 3 injury with fecal material?
What is the recommended antibiotic treatment for a contaminated type 3 injury with fecal material?
What is the classification for a wound that measures 3 cm in length?
What is the classification for a wound that measures 3 cm in length?
Which primary surgery method is most commonly used for temporary or permanent fixation of fractures?
Which primary surgery method is most commonly used for temporary or permanent fixation of fractures?
How long should secondary surgery for soft tissue occur after the initial injury?
How long should secondary surgery for soft tissue occur after the initial injury?
What characterizes Type 3B injuries in the Gustillo and Anderson classification?
What characterizes Type 3B injuries in the Gustillo and Anderson classification?
Which phase of healing involves the stabilization of a hematoma through fibrin fibers?
Which phase of healing involves the stabilization of a hematoma through fibrin fibers?
What is the probability of amputation in Type 3C injuries?
What is the probability of amputation in Type 3C injuries?
During which phase does endochondral ossification primarily occur?
During which phase does endochondral ossification primarily occur?
Which factor primarily leads to the development of necrotic bone fragments without soft tissue connection?
Which factor primarily leads to the development of necrotic bone fragments without soft tissue connection?
For patients who have not been vaccinated against tetanus, what action should be taken?
For patients who have not been vaccinated against tetanus, what action should be taken?
Flashcards
Trauma Priority
Trauma Priority
Saving life is the top priority in trauma cases, focusing on major injuries (head, abdomen, pelvic fractures, extremities, vascular injuries, open fractures, etc.)
Initial Trauma Assessment
Initial Trauma Assessment
Quickly assessing and stabilizing the patient using the ABCDE method (Airway, Breathing, Circulation, Disability, Exposure).
Fracture Components
Fracture Components
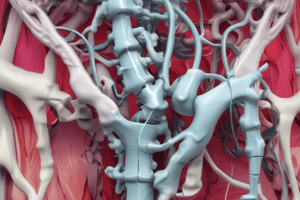
Fractures involve damage to bone, periosteum, muscle, subcutaneous tissue and skin.
Soft Tissue Importance
Soft Tissue Importance
Signup and view all the flashcards
Bone Blood Supply
Bone Blood Supply
Signup and view all the flashcards
Fracture Diagnosis
Fracture Diagnosis
Signup and view all the flashcards
Fracture Types
Fracture Types
Signup and view all the flashcards
Open Fracture
Open Fracture
Signup and view all the flashcards
Fracture Signs
Fracture Signs
Signup and view all the flashcards
Fracture Impact
Fracture Impact
Signup and view all the flashcards
Gustillo-Anderson Type 1 Fracture
Gustillo-Anderson Type 1 Fracture
Signup and view all the flashcards
Gustillo-Anderson Type 2 Fracture
Gustillo-Anderson Type 2 Fracture
Signup and view all the flashcards
Gustillo-Anderson Type 3C Fracture
Gustillo-Anderson Type 3C Fracture
Signup and view all the flashcards
Primary Fracture Fixation (Plates)
Primary Fracture Fixation (Plates)
Signup and view all the flashcards
Primary Fracture Fixation (Intramedullary Nails)
Primary Fracture Fixation (Intramedullary Nails)
Signup and view all the flashcards
External Fixation
External Fixation
Signup and view all the flashcards
Secondary Surgery (Soft Tissue)
Secondary Surgery (Soft Tissue)
Signup and view all the flashcards
Secondary Surgery (Bone Tissue)
Secondary Surgery (Bone Tissue)
Signup and view all the flashcards
Inflammation Phase Healing
Inflammation Phase Healing
Signup and view all the flashcards
Repair Phase Healing
Repair Phase Healing
Signup and view all the flashcards
Remodeling Phase (Fracture)
Remodeling Phase (Fracture)
Signup and view all the flashcards
Fracture Healing Factors
Fracture Healing Factors
Signup and view all the flashcards
Rotator Cuff Tear
Rotator Cuff Tear
Signup and view all the flashcards
Soft Tissue Injury Grades
Soft Tissue Injury Grades
Signup and view all the flashcards
Ligament Injury Symptoms
Ligament Injury Symptoms
Signup and view all the flashcards
Strain Grade 1
Strain Grade 1
Signup and view all the flashcards
Strain Grade 2 and 3
Strain Grade 2 and 3
Signup and view all the flashcards
Contusion
Contusion
Signup and view all the flashcards
Intramuscular Hematoma
Intramuscular Hematoma
Signup and view all the flashcards
Intermuscular Hematoma
Intermuscular Hematoma
Signup and view all the flashcards
Study Notes
Trauma Evaluation Priorities
- Saving lives through treating major abdominal and head injuries, pelvic fractures (difficult to assess bleeding), and saving extremities with vascular injuries or open fractures.
- Joint dislocations and fracture reduction are crucial.
- Initial assessment includes assessment and resuscitation, and applying trauma ABCDE (airway, breathing, circulation, disability, exposure).
- Tissues damaged in fractures include bone, periosteum, muscle, subcutaneous fat, and skin.
- Skin's importance as a primary barrier against infection.
- Muscles help with circulation.
- Periosteum, providing blood supply (outer layer), includes osteoprogenitor cells.
- Bone blood supply comes from arteries such as feeding, metaphyseal-epiphyseal and periosteal artery systems.
- Fractures, causing impaired bone integrity usually associated with soft tissue injury.
- Diagnosis via plain radiographs in two planes, at right angles to each other, with one view from above and below the joint.
Fracture Types
- Open fractures involve a fracture communicating with the external environment without a skin barrier.
- 3% of fractures in the extremities (femur or humerus) are open fractures.
- Rapid wound assessment and removal of contamination are necessary.
- Use sterile, moist, loose dressing for single use.
- Antibiotic treatment depends on the type of bacteria, e.g., Gram (+) use cephalosporins, Gram (-) use aminoglycosides, and contaminated wounds may require penicillin.
Fracture Findings
- Pain and tenderness
- Deformity
- Swelling
- Limited range of motion (ROM)
- Ecchymosis (bruising)
- Pathological motion
Tetanus Prophylaxis
- Tetanus toxoid is required.
- Individuals <5 years old generally do not need vaccination.
- Individuals > 5 years old should have a booster vaccination.
- No vaccine is required for individuals who have had a dose of tetanus vaccine in the past year.
Gustillo & Anderson Classification
- Type I: <1 cm
- Type II: 1-10 cm
- Type III: divided by the presence or absence of soft tissue coverage.
- Type III-A: Adequate soft tissue coverage.
- Type III-B: Inadequate soft tissue coverage. -Type III-C: Vascular injury requiring repair
Primary Surgery Fracture Fixations
- Plates, often used for upper extremity and metaphyseal fractures.
- Intramedullary (IM) nails might be used with or without reaming, especially for type 3B fractures.
- External fixators (EFs) are often the most common temporary or permanent fixation method.
Secondary Surgery Soft Tissue and Bone Tissue
- Soft-tissue transfer often happens as soon as possible (within 7 days).
- Types I, II, and III-A fractures may have primary closures.
- Type III-B fractures necessitate soft tissue transfer for proper bone closure.
- Internal fixation transition is key; defects are closed using bone transport or vascularized bone grafting (8–12 weeks).
Healing Phases
- Inflammation phase (1–4 days): fragments of devascularized tissue, macrophage/neutrophil action, clearing necrotic bone fragments, and formation of hematoma.
- Repair phase (2–40 days): primary callus response, angiogenesis, collagen fibers for loosely binding fragments, and endochondral ossification.
- Remodelling phase (25–100+) : bone returns to normal shape.
Factors Affecting Fracture Healing
- Age
- Chronic disease
- Vascular damages
- Smoking
- Nerve function
- Sterility (open fractures)
Soft Tissue Injuries
- 1st degree: microscopic structural damage, mild tenderness
- 2nd degree: Partial tissue rupture, swelling and tenderness.
- 3rd degree: Complete tissue rupture, significant swelling, and instability.
Ligament Injuries
- Bruising, swelling, tenderness, pain on movement/palpation, and instability, especially with significant injuries.
- MRI scans confirm diagnoses.
Strains
- First-degree: minimal strength/movement loss, pain on active/passive stretching.
- Second-/Third-degree: significant functional loss, severe pain exacerbated by muscle contraction, and potential palpable defects resembling tumors.
Contusions
- Caused by direct blows, causing bleeding within a muscle, muscle tears with heavy bleeding.
Intramuscular Hematoma
- Bleeding within muscle fascia, causing swelling and limited mobility.
- Damage may include fascia and adjacent blood vessels and/or bleeding between muscles.
- Swelling occurs slowly distally to the injury site within 24–48 hours.
- Muscle function often gradually improves.
- Treatment usually involves RICE (Rest, Ice, Compression, Elevation).
Cubitus Valgus/Varus and Genu Varum/Valgum
- These describe forearm and knee angulation issues.
Skeletal Alignment
- Specific grades describe the degree of misalignment and joint instability.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.