Podcast
Questions and Answers
At what vertebral level does the trachea begin in the neck?
At what vertebral level does the trachea begin in the neck?
- Upper border of T1
- Lower border of C7
- Lower border of C6 (correct)
- Upper border of C5
At what anatomical landmark does the trachea terminate in the thorax?
At what anatomical landmark does the trachea terminate in the thorax?
- Xiphoid process
- Sternal angle (correct)
- Manubrium
- Suprasternal notch
Which part of the trachea lies predominantly in the neck?
Which part of the trachea lies predominantly in the neck?
- Cervical part (correct)
- Carinal part
- Thoracic part
- Mediastinal part
Which of the following structures causes the trachea to deviate slightly to the right at its lower end?
Which of the following structures causes the trachea to deviate slightly to the right at its lower end?
What type of cartilage forms the incomplete rings that support the trachea?
What type of cartilage forms the incomplete rings that support the trachea?
What is the name of the muscle that connects the ends of the C-shaped cartilaginous rings of the trachea?
What is the name of the muscle that connects the ends of the C-shaped cartilaginous rings of the trachea?
What is the name of the ridge formed by the last tracheal cartilage that projects upwards inside the trachea?
What is the name of the ridge formed by the last tracheal cartilage that projects upwards inside the trachea?
Which structure constricts the trachea at its upper end?
Which structure constricts the trachea at its upper end?
Which artery constricts the trachea at its middle?
Which artery constricts the trachea at its middle?
Which structure is posterior to the thoracic part of the trachea?
Which structure is posterior to the thoracic part of the trachea?
Which artery provides the arterial supply to the trachea?
Which artery provides the arterial supply to the trachea?
Which structure provides the nerve supply to the trachea?
Which structure provides the nerve supply to the trachea?
Into which lymph nodes does the lymphatic drainage of the trachea primarily occur?
Into which lymph nodes does the lymphatic drainage of the trachea primarily occur?
What is the approximate length of the trachea?
What is the approximate length of the trachea?
The right bronchus differs from the left bronchus in that it is:
The right bronchus differs from the left bronchus in that it is:
What is the approximate angle formed by the right bronchus with the middle line of the trachea?
What is the approximate angle formed by the right bronchus with the middle line of the trachea?
Which of the following is a characteristic of the left principal bronchus compared to the right?
Which of the following is a characteristic of the left principal bronchus compared to the right?
How many lobar bronchi does the right principal bronchus divide into to supply the lobes of the lung?
How many lobar bronchi does the right principal bronchus divide into to supply the lobes of the lung?
From which artery does the right bronchus typically receive its blood supply?
From which artery does the right bronchus typically receive its blood supply?
Where does venous drainage from the right bronchus typically terminate?
Where does venous drainage from the right bronchus typically terminate?
The left bronchus typically receives blood supply from which arteries?
The left bronchus typically receives blood supply from which arteries?
After entering the thorax, the esophagus passes behind which structure at the level of the sternal angle?
After entering the thorax, the esophagus passes behind which structure at the level of the sternal angle?
In the mediastinum, the thoracic duct travels superiorly, and is located anterior to the vertebral column, but posterior to what anatomical structure?
In the mediastinum, the thoracic duct travels superiorly, and is located anterior to the vertebral column, but posterior to what anatomical structure?
Flashcards
Trachea Location
Trachea Location
The trachea begins at the lower border of C6 and ends at the sternal angle (T4/T5), dividing into two principal bronchi.
Trachea Size
Trachea Size
About 4-5 inches (10-12 cm) long and 1/2-3/4 inch (1.5-2 cm) in diameter.
Trachea Parts
Trachea Parts
The upper half lies in the neck (cervical part), and the lower half in the thorax (thoracic part).
Trachea Structure
Trachea Structure
Signup and view all the flashcards
Carina
Carina
Signup and view all the flashcards
Trachea Constrictions
Trachea Constrictions
Signup and view all the flashcards
Location of the tracheal cartilage?
Location of the tracheal cartilage?
Signup and view all the flashcards
Arterial Supply of Trachea
Arterial Supply of Trachea
Signup and view all the flashcards
Venous Drainage of Trachea
Venous Drainage of Trachea
Signup and view all the flashcards
Nerve Supply of Trachea
Nerve Supply of Trachea
Signup and view all the flashcards
Lymphatic Drainage of Bronchi
Lymphatic Drainage of Bronchi
Signup and view all the flashcards
Esophagus Location
Esophagus Location
Signup and view all the flashcards
Esophagus Constrictions
Esophagus Constrictions
Signup and view all the flashcards
Esophagus Curvatures
Esophagus Curvatures
Signup and view all the flashcards
Arterial Supply of Esophagus
Arterial Supply of Esophagus
Signup and view all the flashcards
Blood Supply to Thoracic Esophagus
Blood Supply to Thoracic Esophagus
Signup and view all the flashcards
Lymphatic Drainage of Esophagus
Lymphatic Drainage of Esophagus
Signup and view all the flashcards
Nerve Supply of Esophagus
Nerve Supply of Esophagus
Signup and view all the flashcards
Esophagus Relations
Esophagus Relations
Signup and view all the flashcards
Thoracic Duct
Thoracic Duct
Signup and view all the flashcards
Thoracic Duct Origin
Thoracic Duct Origin
Signup and view all the flashcards
Thoracic Duct Tributaries
Thoracic Duct Tributaries
Signup and view all the flashcards
Thoracic Duct Drainage
Thoracic Duct Drainage
Signup and view all the flashcards
Right Lymphatic Duct Formation
Right Lymphatic Duct Formation
Signup and view all the flashcards
Lymph Nodes of Thorax
Lymph Nodes of Thorax
Signup and view all the flashcards
Study Notes
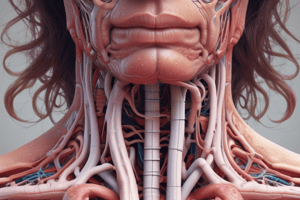
- The trachea begins in the neck at the level of the lower border of C6, continuing from the larynx
- It ends in the thorax at the sternal angle (disc between T4/T5), dividing into 2 principal bronchi
- Approximate tracheal dimensions are 4-5 inches (10-12 cm) long and 1/2-3/4 inch (1½-2 cm) in diameter
- The upper half of the trachea resides in the neck (cervical part), and the lower half in the thorax (thoracic part)
- The thoracic part spans the entire superior mediastinum from the suprasternal notch to the sternal angle
- The trachea is midline except at its lower end, where it deviates to the right due to the aortic arch
- As the trachea descends, it recedes from the surface, following the vertebral column's curvature
- Surface anatomy can be represented by a 2 cm wide band from the lower larynx to the sternal angle, just right of the median plane
Structure of Trachea
- An elastic tube maintained by 16-20 C-shaped cartilaginous rings
- The opening of the C-shaped rings faces backward to allow for esophageal distension during swallowing
- Smooth muscle fibers (trachealis muscle) connect the 2 ends of each cartilaginous ring
- The lower border of the last cartilaginous ring projects upwards inside the trachea, forming the carina
Constrictions of the Trachea
- Constriction at the upper end is due to the thyroid gland
- Constriction at the middle is due to the brachiocephalic artery on the right side
- Constriction at the lower end is due to the arch of the aorta on the left side
Relations of the Thoracic Part of the Trachea
- Anteriorly, relations from before backwards: manubrium sterni and the left brachiocephalic vein running obliquely along the upper aspect of the arch of the aorta
- Posteriorly, relations: the esophagus and the left recurrent laryngeal nerve between the trachea and esophagus
- On the right side, relations include: right vagus nerve, paratracheal lymph nodes, upper part of the brachiocephalic artery, right brachiocephalic vein, the upper half of the superior vena cava, arch of the azygos vein, and mediastinal surface of right pleura and lung
- On the left side, relations include: left subclavian artery, upper part of the left common carotid artery, arch of the aorta, paratracheal lymph nodes, and mediastinal surface of the left pleura and lung
- At the bifurcation of the trachea relations include: the deep cardiac plexus on the front and sides of the bifurcation, and three groups of tracheobronchial lymph nodes
Blood Supply, Lymphatic Drainage and Innervation
- Arterial supply: bronchial arteries
- Venous drainage: bronchial veins to the azygos system
- Lymphatics drain to tracheobronchial and paratracheal lymph nodes
- Nerve Supply: autonomic fibers from 2 vagi and their recurrent laryngeal branches and sympathetic chains
Bronchi
- Arise from the lower end of the trachea at the level of the sternal angle (disc between T4/T5), bifurcating into 2 principal (main) bronchi
- Each bronchus descends downwards and laterally into the lung at its hilum
- The right and left bronchi differ in length, width, direction, way of division, relations, and blood supply
Difference between Right and Left Bronchi
- The right bronchus is shorter (one inch), wider and more in line with the trachea, forming a 25° angle
- The left bronchus is longer (2 inches), narrower, and more horizontal, forming a 45° angle
- The right principal bronchus divides into 3 lobar bronchi for the 3 lobes of the lung; the superior lobar bronchus arises outside the hilum
- The left principal bronchus divides into 2 lobar bronchi for the 2 lobes of the lung, as it enters the hilum
- The right bronchus receives one (right) bronchial artery from the 3rd right posterior intercostal or the upper left bronchial artery; venous drainage ends in the azygos vein
- The left bronchus receives 2 (left) bronchial arteries from the descending thoracic aorta; venous drainage ends in the superior and inferior hemiazygos veins
Lymphatic Drainage and Innervation of 2 Bronchi
- Lymphatics drain into inferior tracheobronchial nodes and a chain of bronchopulmonary nodes
- The 2 bronchi receive autonomic fibres from the 2 vagi (parasympathetic) and 2 sympathetic chains via the anterior and posterior pulmonary plexuses
Clinically Important Points on Trachea and Bronchi
- The trachea may be compressed/displaced by enlarged lymph nodes or aortic arch
- Carina may widen or distort (seen by bronchoscope) with inferior tracheobronchial lymph node cancer involvement
- A foreign body entering the trachea goes to the right bronchus due to its wider and more in-line structure
Oesophagus
- It is approximately 10 inches (25 cm) long, starting in the neck at the lower border of C6 and ending in the abdomen at the lower border of T10, joining the stomach
Constrictions of the Oesophagus
- Four normal constrictions exist: beginning (7 inches/17 cm from incisors), aortic arch crossing (9 inches/22 cm from incisors), left principal bronchus crossing (11 inches/27 cm from incisors), and esophageal opening of the diaphragm (17 inches/42 cm from incisors)
Curvatures of the Esophagus
- Anteroposterior curves follow the vertebral column with the thoracic part concave anteriorly
- Left lateral curves are exhibited at the upper thorax and below T7, where it deviates to reach the esophageal opening of the diaphragm
Thoracic Part of the Oesophagus
- The esophagus enters the thorax through the inlet, midline between the trachea (front) and vertebral column (behind)
- It runs vertically downwards in the superior mediastinum
- At the sternal angle, it passes behind the left principal bronchus into the posterior mediastinum
- It descends along the right side of the descending thoracic aorta, behind the pericardium and base of the heart (mainly the left atrium) down to T7
- Below T7, it deviates forwards and to the left, crossing the descending thoracic aorta to reach the esophageal opening of the diaphragm at T10
- At T10, it leaves the thorax to enter the abdomen
Blood Supply and Lymphatic Drainage of Oesophagus
- Thoracic part: esophageal branches from the descending aorta and bronchial arteries
- Venous drainage: azygos and hemiazygos veins
- Lymphatics: tracheobronchial, brachiocephalic, and posterior mediastinal lymph nodes
Nerve Supply of Esophagus
- Autonomic nerves form anterior and posterior esophageal nerve plexuses
- Parasympathetic fibres from the 2 vagi and sympathetic fibres from the upper 5 thoracic sympathetic ganglia
Clinically Important Points for Oesophagus
- Oesophagoscopy measurements from upper incisor teeth correspond to normal constriction levels
- Narrowest parts are sites for impacted foreign bodies and strictures after corrosive fluids
- Oesophagus relates to base of heart/left atrium and may enlarge in mitral stenosis, displacing the oesophagus backwards
- The approach during surgery can be done on the right side, as it is crossed on the right side by the azygos vein
Thoracic Duct
- The main lymphatic vessel in the body, about 45 cm long, running from the upper abdomen to neck root
- It begins in the abdomen from cisterna chyli and enters the thorax through the aortic opening of the diaphragm, between the aorta and azygos vein
- It traverses the thorax first in the posterior mediastinum then in the superior mediastinum to enter the root of the neck where it empties into in the angle between the left internal jugular and left subclavian veins
Tributaries of the Thoracic Duct in the Thorax
- Posterior intercostal nodes, draining parts of the thoracic wall, and posterior mediastinal nodes, draining the oesophagus, pericardium, and diaphragm
Field of Lymph Drainage of the Thoracic Duct
- The two lower limbs, the left side of the thorax, the abdomen (except upper surface of right lobe of liver), the left upper limb, and the left side of head and neck
Right Lymphatic Duct
- Short lymph trunk which lies in the right side of the root of the neck and corresponds to the thoracic duct
- It is formed by the union of the right jugular, subclavian and bronchomediastinal lymph trunks
- It ends by opening in the angle between the right internal jugular and right subclavian veins.
- Field of lymph drainage: right side of the head and neck, right upper limb, right side of the thorax, and upper surface of right lobe of the liver
Lymphatic Drainage of the Thoracic Contents
- Pericardium and heart: brachiocephalic, posterior mediastinal, and tracheobronchial lymph nodes
- Esophagus and descending aorta: tracheobronchial, brachiocephalic and the posterior mediastinal lymph nodes
- Lungs, bronchi and trachea: pulmonary, bronchopulmonary, tracheobronchial and paratracheal lymph nodes
Lymph Nodes of the Thorax
- Parasternal Lymph Nodes are at the anterior ends of the upper 6 intercostal spaces, alongsidethe internal thoracic artery that drains deep parts of the anterior thoracic wall and the medial part of the mammary gland, and efferent vessels join the bronchomediastinal lymph trunk
- Intercostal Lymph Nodes at the posterior ends of the intercostal spaces that drain deep parts of the posterolateral thoracic wall, and efferent vessels unite with efferent vessels
- Diaphragmatic Lymph Nodes on the upper surface of the diaphragm (anterior, posterior, and left lateral groups) that drains the diaphragm
- Brachiocephalic (anterior mediastinal) Lymph Nodes are in the anterior part of the superior mediastinum along the left brachiocephalic vein that drains Pericardium and heart
- Posterior mediastinal Lymph Nodes in the posterior mediastinum close to the oesophagus anddescending thoracic aorta that drains the esophagus, pericardium, and efferent vessels from posterior diaphragmatic lymph nodes
- Lymph nodes draining the lungs, bronchi and trachea: pulmonary nodes, bronchopulmonary nodes, tracheobronchial nodes, and paratracheal nodes
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.