Podcast
Questions and Answers
Which characteristic distinguishes connective tissue from epithelial tissue?
Which characteristic distinguishes connective tissue from epithelial tissue?
- Presence of a basement membrane
- Cells are tightly packed together
- Abundant extracellular matrix between cells (correct)
- Ability to readily divide
What type of tissue is defined as a group of similar cells with a common function?
What type of tissue is defined as a group of similar cells with a common function?
- Organ
- System
- Organelle
- Tissue (correct)
Which of the following is NOT a major type of tissue in the human body?
Which of the following is NOT a major type of tissue in the human body?
- Muscle tissue
- Osseous tissue (correct)
- Epithelial tissue
- Connective tissue
Which type of intercellular junction creates a barrier that prevents the movement of substances between cells?
Which type of intercellular junction creates a barrier that prevents the movement of substances between cells?
What is the primary function of desmosomes in tissues?
What is the primary function of desmosomes in tissues?
Which type of intercellular junction allows for the exchange of substances between cells?
Which type of intercellular junction allows for the exchange of substances between cells?
Which characteristic is NOT associated with epithelial tissues?
Which characteristic is NOT associated with epithelial tissues?
Which feature is characteristic of simple squamous epithelium?
Which feature is characteristic of simple squamous epithelium?
In what type of tissue would you find cells that readily allow substances to pass through, such as in the air sacs of the lungs?
In what type of tissue would you find cells that readily allow substances to pass through, such as in the air sacs of the lungs?
What primary function is associated with simple cuboidal epithelium?
What primary function is associated with simple cuboidal epithelium?
Where is simple cuboidal epithelium commonly found in the body?
Where is simple cuboidal epithelium commonly found in the body?
What structural feature is characteristic of simple columnar epithelium?
What structural feature is characteristic of simple columnar epithelium?
Microvilli and goblet cells are commonly found in which type of epithelium?
Microvilli and goblet cells are commonly found in which type of epithelium?
What is a key characteristic of pseudostratified columnar epithelium?
What is a key characteristic of pseudostratified columnar epithelium?
Which tissue type is primarily found lining the respiratory passageways and is characterized by having cilia and goblet cells?
Which tissue type is primarily found lining the respiratory passageways and is characterized by having cilia and goblet cells?
What is the primary function of stratified squamous epithelium?
What is the primary function of stratified squamous epithelium?
Where would keratinized stratified squamous epithelium be most likely found?
Where would keratinized stratified squamous epithelium be most likely found?
What structural characteristic defines stratified cuboidal epithelium?
What structural characteristic defines stratified cuboidal epithelium?
What is the primary characteristic of transitional epithelium that allows it to function effectively?
What is the primary characteristic of transitional epithelium that allows it to function effectively?
Which location is most likely to contain transitional epithelium?
Which location is most likely to contain transitional epithelium?
Glandular epithelium is characterized by its...
Glandular epithelium is characterized by its...
What is the key difference between endocrine and exocrine glands?
What is the key difference between endocrine and exocrine glands?
Merocrine glands secrete their products by...
Merocrine glands secrete their products by...
Apocrine glands are characterized by...
Apocrine glands are characterized by...
Holocrine glands release their products by...
Holocrine glands release their products by...
Which of the following is NOT a function of connective tissues?
Which of the following is NOT a function of connective tissues?
What is the most abundant tissue type in the body by weight?
What is the most abundant tissue type in the body by weight?
Which cell type found in connective tissue secretes fibers into the extracellular matrix?
Which cell type found in connective tissue secretes fibers into the extracellular matrix?
What role do macrophages play in connective tissue?
What role do macrophages play in connective tissue?
What is the function of mast cells in connective tissue?
What is the function of mast cells in connective tissue?
Which of the following is NOT a type of fiber found in connective tissue?
Which of the following is NOT a type of fiber found in connective tissue?
Which characteristic is associated with collagen fibers?
Which characteristic is associated with collagen fibers?
Elastic fibers are primarily composed of what protein?
Elastic fibers are primarily composed of what protein?
Where are reticular fibers most commonly found?
Where are reticular fibers most commonly found?
Which of the following is a characteristic of loose connective tissue?
Which of the following is a characteristic of loose connective tissue?
Which of the following is NOT a type of loose connective tissue?
Which of the following is NOT a type of loose connective tissue?
Which type of tissue is characterized by having abundant yellow elastic fibers and some collagenous fibers?
Which type of tissue is characterized by having abundant yellow elastic fibers and some collagenous fibers?
Chondrocytes are cells specifically found in what type of tissue?
Chondrocytes are cells specifically found in what type of tissue?
What is the primary role of fibroblasts within connective tissue?
What is the primary role of fibroblasts within connective tissue?
How does the arrangement of collagen fibers in dense irregular connective tissue contribute to its function?
How does the arrangement of collagen fibers in dense irregular connective tissue contribute to its function?
How do merocrine glands differ from holocrine glands in their mode of secretion?
How do merocrine glands differ from holocrine glands in their mode of secretion?
Which statement best describes the functional significance of transitional epithelium?
Which statement best describes the functional significance of transitional epithelium?
What distinguishes elastic cartilage from hyaline cartilage regarding composition and function?
What distinguishes elastic cartilage from hyaline cartilage regarding composition and function?
How do the structural differences between compact bone and spongy bone relate to their respective functions?
How do the structural differences between compact bone and spongy bone relate to their respective functions?
What is the functional consequence of the presence of microvilli on the apical surface of simple columnar epithelium?
What is the functional consequence of the presence of microvilli on the apical surface of simple columnar epithelium?
If a person has a genetic disorder affecting collagen synthesis, which of the following tissues would likely be most affected?
If a person has a genetic disorder affecting collagen synthesis, which of the following tissues would likely be most affected?
How do gap junctions facilitate intercellular communication in tissues such as cardiac muscle?
How do gap junctions facilitate intercellular communication in tissues such as cardiac muscle?
What characteristic of pseudostratified columnar epithelium explains its classification, and what adaptation is commonly associated with it?
What characteristic of pseudostratified columnar epithelium explains its classification, and what adaptation is commonly associated with it?
What roles do wandering cells, such as macrophages, play in connective tissue?
What roles do wandering cells, such as macrophages, play in connective tissue?
How does the avascular nature of epithelial tissue influence its metabolic requirements and relationship with adjacent tissues?
How does the avascular nature of epithelial tissue influence its metabolic requirements and relationship with adjacent tissues?
Which type of connective tissue would likely be found in ligaments, and why is it suited for this location?
Which type of connective tissue would likely be found in ligaments, and why is it suited for this location?
In what way does stratified squamous epithelium demonstrate the relationship between structure and function?
In what way does stratified squamous epithelium demonstrate the relationship between structure and function?
How does the presence of chondrocytes in lacunae contribute to cartilage function?
How does the presence of chondrocytes in lacunae contribute to cartilage function?
What is a key difference between epithelium and connective tissue regarding blood supply and cell density?
What is a key difference between epithelium and connective tissue regarding blood supply and cell density?
Endocrine glands and Exocrine glands differ, because endocrine glands?
Endocrine glands and Exocrine glands differ, because endocrine glands?
Which type of tissue is responsible for conducting electrical impulses to facilitate communication between different parts of the body?
Which type of tissue is responsible for conducting electrical impulses to facilitate communication between different parts of the body?
What is the primary function of serous membranes in the body?
What is the primary function of serous membranes in the body?
Which of the following represents a critical function of blood as a specialized connective tissue?
Which of the following represents a critical function of blood as a specialized connective tissue?
Flashcards
Tissue
Tissue
A group of similar cells with a common function.
Histology
Histology
The study of tissues.
Major Tissue Types
Major Tissue Types
Epithelial, Connective, Muscle, Nervous.
Tight junctions
Tight junctions
Signup and view all the flashcards
Desmosomes
Desmosomes
Signup and view all the flashcards
Gap junction
Gap junction
Signup and view all the flashcards
Epithelial Tissues Function
Epithelial Tissues Function
Signup and view all the flashcards
Characteristics of Epithelial Tissue
Characteristics of Epithelial Tissue
Signup and view all the flashcards
Shapes of Epithelial Cells
Shapes of Epithelial Cells
Signup and view all the flashcards
Epithelial Cell Layers
Epithelial Cell Layers
Signup and view all the flashcards
Simple Squamous Epithelium
Simple Squamous Epithelium
Signup and view all the flashcards
Simple Cuboidal Epithelium
Simple Cuboidal Epithelium
Signup and view all the flashcards
Simple Columnar Epithelium
Simple Columnar Epithelium
Signup and view all the flashcards
Pseudostratified Columnar Epithelium
Pseudostratified Columnar Epithelium
Signup and view all the flashcards
Stratified Squamous Epithelium
Stratified Squamous Epithelium
Signup and view all the flashcards
Stratified Cuboidal Epithelium
Stratified Cuboidal Epithelium
Signup and view all the flashcards
Stratified Columnar Epithelium
Stratified Columnar Epithelium
Signup and view all the flashcards
Transitional Epithelium
Transitional Epithelium
Signup and view all the flashcards
Glandular Epithelium
Glandular Epithelium
Signup and view all the flashcards
Endocrine Glands
Endocrine Glands
Signup and view all the flashcards
Exocrine Glands
Exocrine Glands
Signup and view all the flashcards
Unicellular Exocrine Gland
Unicellular Exocrine Gland
Signup and view all the flashcards
Multicellular Exocrine Gland
Multicellular Exocrine Gland
Signup and view all the flashcards
Merocrine Glands
Merocrine Glands
Signup and view all the flashcards
Apocrine Glands
Apocrine Glands
Signup and view all the flashcards
Holocrine Glands
Holocrine Glands
Signup and view all the flashcards
Connective Tissue
Connective Tissue
Signup and view all the flashcards
Types of Connective Tissue Cells
Types of Connective Tissue Cells
Signup and view all the flashcards
Fibroblast
Fibroblast
Signup and view all the flashcards
Macrophages
Macrophages
Signup and view all the flashcards
Mast Cells Definition
Mast Cells Definition
Signup and view all the flashcards
Types of Connective Tissue Fibers
Types of Connective Tissue Fibers
Signup and view all the flashcards
Collagen Fibers
Collagen Fibers
Signup and view all the flashcards
Elastic Fibers
Elastic Fibers
Signup and view all the flashcards
Reticular Fibers
Reticular Fibers
Signup and view all the flashcards
Types of Connective Tissue Proper
Types of Connective Tissue Proper
Signup and view all the flashcards
Loose Connective Tissue
Loose Connective Tissue
Signup and view all the flashcards
Dense Connective Tissue
Dense Connective Tissue
Signup and view all the flashcards
Specialized Connective Tissues
Specialized Connective Tissues
Signup and view all the flashcards
Chondrodysplasia
Chondrodysplasia
Signup and view all the flashcards
Marfan Syndrome
Marfan Syndrome
Signup and view all the flashcards
Areolar Connective Tissue
Areolar Connective Tissue
Signup and view all the flashcards
Adipose Tissue
Adipose Tissue
Signup and view all the flashcards
Reticular Connective Tissue
Reticular Connective Tissue
Signup and view all the flashcards
Dense Regular Connective Tissue
Dense Regular Connective Tissue
Signup and view all the flashcards
Dense Irregular Connective Tissue
Dense Irregular Connective Tissue
Signup and view all the flashcards
Elastic Connective Tissue
Elastic Connective Tissue
Signup and view all the flashcards
Cartilage
Cartilage
Signup and view all the flashcards
Chondrocytes location
Chondrocytes location
Signup and view all the flashcards
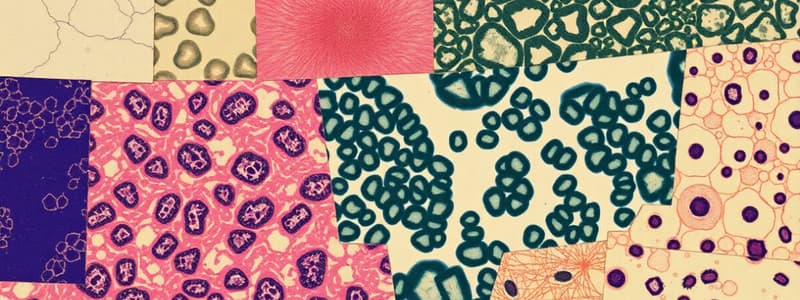
Study Notes
- Cells are organized into tissues in complex organisms.
- A tissue consists of similar cells performing a shared function.
- Histology is the study of tissues.
- The body has four major tissue types: epithelial, connective, muscle, and nervous.
Four Major Tissue Types:
- Epithelial tissue protects, secretes, absorbs, and excretes; it covers body surfaces, lines internal organs, and forms glands.
- Connective tissue binds, supports, and protects, fills spaces, stores fat, and produces blood cells. It is distributed widely.
- Muscle tissue facilitates movement and is present in bones, hollow organ walls, and the heart.
- Nervous tissue conducts impulses for coordination, regulation, integration, and sensory reception and is present in the brain, spinal cord, and nerves.
Intercellular Junctions:
- Tight junctions close the space between cells by fusing cell membranes; an example is cells lining the small intestine.
- Desmosomes bind cells by forming "spot welds" between cell membranes; an example is cells of the outer skin layer.
- Gap junctions form tubular channels between cells for substance exchange; an example is muscle cells of the heart and digestive tract.
General Characteristics of Epithelial Tissues:
- Epithelial tissues cover organs and body surfaces.
- Epithelial tissues line cavities and hollow organs.
- Epithelial tissues comprise glands.
- Epithelial tissues have a free surface on the outside and a basement membrane on the inside.
- Epithelial tissues lack blood vessels (are avascular).
- Nutrients diffuse to from underlying connective tissue to epithelial tissue
- Epithelial tissue cells divide readily, allowing injuries to heal rapidly.
- Cells are tightly packed in epithelial tissues.
- Epithelial tissues are classified by cell shape and number of cell layers.
- Shapes consist of squamous (flat), cuboidal (cube-shaped), and columnar (tall).
- Layers consist of simple (one layer), stratified (two or more layers), or pseudostratified (appears layered but is not).
Simple Squamous Epithelium:
- Single layer of thin, flat cells
- Allows substances to pass easily through air sacs (alveoli) and capillaries.
- Is thin, delicate, and easily damaged.
- Found in diffusion and filtration sites.
- Makes up walls of air sacs (alveoli) and capillaries.
- Lines blood and lymphatic vessels.
Simple Cuboidal Epithelium:
- Single layer of cube-shaped cells
- Involved in secretion and absorption.
- Lines kidney tubules, thyroid follicles, and ducts of some glands.
- Covers ovaries.
Simple Columnar Epithelium:
- Single layer of elongated cells.
- Nuclei usually at the same level, near the bottom of the basement membrane.
- Sometimes possesses microvilli, cilia, or goblet cells (which secrete mucus).
- Involved in secretion and absorption.
- Lines the uterus, stomach, and intestines.
Pseudostratified Columnar Epithelium:
- Single layer, but appears layered.
- Nuclei are at two or more levels.
- Cells vary in shape, but all touch the basement membrane.
- Often possesses cilia and goblet cells.
- Provides protection from infection.
- Lines respiratory passageways.
Stratified Squamous Epithelium:
- Many cell layers; thick.
- Protective layer.
- Outermost cells are squamous, deeper cells are cuboidal.
- New cells produced in deep layers push older cells toward free surface.
- Outer layer of skin, epidermis, is keratinized.
- Lines the oral cavity, vagina, and anal canal.
Stratified Cuboidal Epithelium:
- Two to three layers of cube-shaped cells.
- Provides more protection than one layer.
- Lines ducts of mammary glands, sweat glands, salivary glands, and the pancreas.
Stratified Columnar Epithelium:
- Several layers of cells.
- The top layer made of elongated cells.
- Cube-shaped cells in deeper layers.
- Lines part of the male urethra and ducts of exocrine glands.
Transitional Epithelium (Uroepithelium):
- Many cell layers.
- Composed of cube-shaped and elongated cells.
- Changes shape and appearance with increased tension and stretches.
- Forms a barrier and expansible lining.
- Lines the urinary bladder, ureters, and part of the urethra.
Epithelial Tissues:
- Simple squamous epithelium consists of a single layer of flattened cells where filtration, diffusion, and osmosis occur, covering surfaces in locations such as air sacs of the lungs and walls of capillaries.
- Simple cuboidal epithelium, made of a single layer of cube-shaped cells, is involved in protection, secretion, and absorption such as occurring on the surface of ovaries and lining kidney tubules.
- Simple columnar epithelium features a single layer of elongated cells for protection, secretion, and absorption, lining the uterus, stomach, and intestines
- Pseudostratified columnar epithelium consists of a single layer of elongated cells involved in protection, secretion, and mucus movement with locations in the lining of respiratory passages.
- Stratified squamous epithelium has many layers in the skin and lines the oral cavity featuring protection on top flattened cells
- Stratified cuboidal epithelium with 2 - 3 layers of cube-shaped cells provides protection by lining ducts such as ducts of mammary glands
- Stratified columnar epithelium with the top layer of elongated cells and lower cube-shaped cells protects and secretes in larger ducts of excretory glands
- Transitional epithelium which includes many cube-shaped and elongated cells creates a stretchable and protective inner lining of the urinary bladder, ureters, and part of the urethra
Glandular Epithelium:
- Contains cells that produce and secrete substances into ducts or body fluids.
Two types of glands:
- Endocrine glands secrete into tissue fluid or blood.
- Exocrine glands secrete into ducts that open onto a surface.
Two structural types of exocrine glands:
- Unicellular glands consist of one cell, such as a goblet cell (secreting mucus).
- Multicellular glands consist of many cells and can be simple or compound.
Structural types of exocrine glands:
- Simple glands features that duct does not branch
- Compound glands features duct that branches before it reaches secretory portion
- Tubular glands consist of epithelial-lined tubes
- Alveolar glands features its terminal portions in sac-like dilations
Types of glandular secretion:
- Merocrine glands secrete fluid products by exocytosis such as salivary and sweat glands, and the pancreas.
- Apocrine glands lose a small part of their cells during secretion such as mammary and ceruminous glands.
- Holocrine glands release entire cells filled with product such as sebaceous glands.
Types of Exocrine Glands:
- Unicellular glands are single secretory mucus-secreting cells.
- Multicellular glands consist of many cells.
- Simple Glands communicate with the surface through unbranched ducts.
- The simple tubular gland is a straight tube that opens directly onto the surface which makes up intestinal glands within the small intestine.
- The simple branched tubular gland is a branched tube gland with a duct being short or absent and is apart of the gastric glands.
- The simple coiled tubular gland is a long coiled tube-like gland with a long duct and its the merocrine sweat glands in the skin.
- The simple branched alveolar gland consists of the secretory portions of gland expanding into sac like compartments the integumentary system.
- Compound glands communicate with the surface via repeatedly branching ducts.
- The compound tubular gland is where Secretory portions are tubules extending from branches of branches that combine into one duct. An example is the bulbourethral glands of the male (see Figure 22.4) An example is the sebaceous gland of skin
- The compound alveolar gland is where secretory portions are irregularly branched tubules with numerous saclike outgrowths. Mammary glands (see Figure 23.28)
General characteristics of connective tissues:
- Most abundant tissue type by weight.
- Cells are farther apart than epithelial cells.
- Contain abundant extracellular matrix between cells made of protein fibers and a ground substance.
- Consistency varies from fluid to solid.
Categories of connective tissues:
- Connective tissue proper.
- Specialized connective tissues.
- Most have a good blood supply, so are well-nourished.
- Most cells can divide.
- Contain fixed cells, which remain in one place, and wandering cells move throughout tissues.
Functions of connective tissues:
- Bind structures together.
- Provide support and protection.
- Serve as frameworks.
- Fill spaces.
- Store fat.
- Produce blood cells.
- Protect against infections.
- Help repair tissue damage.
Major Cell Types of Connective Tissue:
- Fibroblasts are the most common fixed cell, are large and star-shaped, and secrete fibers into the extracellular matrix.
- Macrophages (histiocytes) are usually attached to fibers, but can detach and wander to conduct phagocytosis and defend against infection.
- Mast cells are large cells that are widely distributed, release heparin to prevent blood clotting, and release histamine, triggering an inflammatory response.
Connective Tissue Fibers:
- Fibroblasts produce three types of fibers in connective tissue.
- Collagen Fibers are thick threads of collagen which give the body its main structural protein. They are strong and flexible.
- Elastic Fibers are composed of elastin protein, stretch and return to original shape, as well as being found in vocal cords and respiratory air passages.
- Recticular Fibers are thin, branching fibers of collagen. They form delicate supporting networks and are found in the spleen and liver.
Components of Connective Tissue:
- Fibroblasts are widely distributed, large, star-shaped cells that secrete proteins that become fibers.
- Macrophages are mobile cells that clear foreign particles from tissues by phagocytosis.
- Mast cells are large cells near blood vessels that release substances to prevent blood clotting (heparin) and to promote inflammation (histamine).
- Collagen fibers (white fibers) are thick, threadlike fibers of collagen with great tensile strength, holding structures together.
- Elastic fibers (yellow fibers) consist of bundles of microfibrils embedded in proteins, which provide elastic quality to parts that stretch.
- Reticular fibers are thin fibers of collagen that form supportive networks within tissues.
- Ground substance consists of a nonfibrous protein and other molecules, which fills space around cells and fibers.
Categories of Connective Tissue:
- Connective Tissue Proper has loose and dense connective tissues.
- Loose connective tissue has fewer collagen fibers than dense tissues.
- Types: Areolar, Adipose, Reticular. Example: Beneath most epithelia, where it nourishes nearby epithelial cells.
- Dense connective tissues contain abundant collagen fibers.
- Types: Dense regular, Dense irregular, Elastic. Example: Tendons, ligaments, dermis
- Loose connective tissue has fewer collagen fibers than dense tissues.
- Specialized connective tissues have Cartilage, Bone, and Blood. Example: The inner most lining of Bone (Spongy)
Clinical Application of Connective Tissue Proper:
- Collagen makes up >60% of protein in bone and cartilage.
- Collage chains are vulnerable to disruption.
- Chondrodysplasia where collagen chains are asymmetric cause stunted growth and deformed joints
- Marfan syndrome a deficiency of fibrillin which leads to long limbs, sinkin chest and and weak aorta
Areolar Connective Tissue:
- Forms thin, delicate membranes.
- Cells mainly are fibroblasts in a gel-like ground substance.
- Composed of collagenous and elastic fibers.
- Exists in the subcutaneous layer.
- Located beneath most epithelia, where it nourishes nearby epithelial cells.
Adipose Tissue (Fat):
- Has adipocytes, which store fat.
- Pushes nuclei to one side.
- Crowds out other cell types.
- Cushions and Insulates.
- Located beneath skin (subcutaneous layer), behind eyeballs, around the heart and kidneys, and in spaces between muscles.
Reticular Connective Tissue:
- Consists of a network of thin reticular fibers.
- Supports walls of internal organs.
- Walls of the liver and spleen.
Dense Regular Connective Tissue:
- Closely packed collagenous fibers.
- A fine network of elastic fibers.
- Most cells are fibroblasts.
- Very strong; withstands pulling and binds body parts together.
- Found in tendons, ligaments, and the dermis.
- Has poor blood supply; slow to heal.
Dense Irregular Connective Tissue:
- Features randomly organized, thick, interwoven collagenous fibers.
- It can withstand tension exerted from different directions.
- Located in the dermis of skin and around skeletal muscles.
Elastic Connective Tissue:
- Has abundant yellow elastic fibers and some collagenous fibers.
- Contains fibroblasts.
- Found in attachments between bones of the spinal column.
- Exists in walls of hollow organs, such as large arteries and airways.
- Found in parts of the heart.
- Has elastic quality and stretches.
Specialized Connective Tissues:
- Contain cartilage, bone, and blood
- They have unique matrices with specialized cells.
Cartilage:
- A rigid, specialized connective tissue
- Provides support, framework, and attachments.
- Offers protection of underlying tissue.
- Is a model for developing bone.
- The matrix contains collagen in gel-like ground substance.
- Has chondrocytes (cartilage cells) in lacunae (chambers), surrounded by matrix.
- Lacks a blood supply; heals slowly.
- Covered by perichondrium, to provide nutrients to the cartilage.
- Hyaline, Elastic, and Fibrocartilage are 3 types of cartilage.
Types of Cartilage:
- Hyaline cartilage is the most common type with fine collagen fibers which makes up ends of bones in joints, nose, respiratory passages, and the embryonic skeleton.
- Elastic cartilage is flexible which is found in the external ear, larynx
- Fibrocartilage, which is very tough due to many collagen fibers makes up the shock absorber, intervertebral disc and menisci of the knee.
Bone (Osseous Tissue):
- The most rigid connective tissue
- Solid matrix, composed of mineral (calcium) salts and collagen.
- This is important for Supports structures and Protects vital structures.
- One key responsibility is Producing blood cells along with storing and releasing Ca and P
- Bone is an important Attachment site for muscles and bone is important.
- Forms the skeleton.
- Bone contains osteocytes (bone cells) in lacunae with 2 types being compact and spongy bone
Bone Tissue:
- Compact Bone features osteoblasts depositing matrix alongisde lamella.
- Osteocytes within matrix form cylindrical units called osteoms which are cemented together.
- Central canals well nourish osteons and are heal faster
- Spongy Bone forms bony plates containing osteocytes with space between for marrow. Spongy Bone is also lighter than compact bone.
Blood:
- Consists of formed elements (cells and fragments) suspended in a fluid matrix called plasma.
- Contains Red blood cells that transport gases.
- Contains White blood cells that defend again infection.
- Contains Platelets that help in blood clotting.
- Transports substances throughout the body.
Connective Tissue Summary:
- Areolar connective tissue is in a fluid-gel matrix which binds organs together and is beneath the skin, muscles, and linings of epithelial tissues
- Adipose tissue cells are in fluid-gel matrix to store fat
- Reticular connective cells in fluid-gel matrix supports walls of the liver and spleen
- Dense regular connective tissue cells in fluid-gel matrix binds the body parts
- Elastic connective tissue cells in fluid-gel matrix provides stretch
- Hyaline cartilage cells are in solid-gel matrix protects in ends of bones nose and walls of respiratory
- Elastic cartilage cells in solid-gel matrix gives flexible suppor in the external ear and laarynx
- Fibrocartilage cells in solid-gel matrix gives stretchablity to spinal column adn pelvic area
- Bone cells are protective in skelton
- Blood cells as well as platelets in the fluid matrix assist against disease.
Membranes:
- Sheets of cells.
- Epithelial membranes consist of epithelial and connective tissue and cover body surfaces and line cavities;
Three types of epithelial membranes:
- Serous membranes line body cavities not open to the outside, specifically the inner linings of the thorax and abdomen, covers organs, features simple squamous epithelium + areolar connective tissue, and secretes serous fluid for lubrication
- Mucous membranes line cavities and tubes that open to the outside, are in the digestive, respiratory, urinary, and reproductive tracts, which feature the epithelium +areolar connective tissue and goblet cells secrete mucus.
Types of Membranes:
- Cutaneous membranes cover the body surface, are known as skin, and part of the integumentary system.
- Synovial membranes differ from epithelial membranes, composed entirely of connective tissue, and line joint cavities.
General Characteristics of Muscle Tissue:
- Muscle tissues are excitable and responds to nervous system stimulation along with being contractile
- The types skeletal (bones and striated), cardiac (involuntary as well striated), and smooth ( walls of hollow organs and involuntary).
Skeletal Muscle Tissue:
- Attached to bones.
- Striated.
- Voluntary.
- Has long, cylindrical, multinucleated cells.
- Stimulated by nerve cells.
Smooth Muscle Tissue:
- Non-striated.
- Composed of spindle-shaped fibers.
- Located in walls of hollow organs and blood vessels.
- Involuntary.
Cardiac Muscle Tissue:
- Exists only in the wall of the heart.
- Contains branching cells.
- Involuntary.
- Striated.
- Features intercalated discs, specialized intercellular junctions.
Types of Muscle Tissue:
- Skeletal muscle tissue is a Long, thread-like cells, striated, and comprised of many nuclei. Functions consist of being voluntary movement of skeletal parts and it is in the muscles attached to bones and cartilage
- Smooth muscle tissue consists of Shorter cells, single, and central nuclei. Its role is Involuntary movements of internal organs and it is the Walls of hollow internal organs
- Cardiac muscle tissue consists of Branched cells, and are striated, single nucleus to create Heart movements. It is found in The Heart.
Nervous Tissues:
- Found in the brain, spinal cord, and peripheral nerves.
Neurons:
-
Main cells are specialized for communication, via conduction of nerve impulses.
-
They coordinate, integrate, and regulate body functions.
-
Composed of a cell body (soma), dendrites, and an axon.
-
Neuroglia are cells that support and nourish neurons.
-
Nervous tissue has cells with cytoplasmic extensions and help with sensory reception as well as a conduction of electrical impulses. It is foundin the core as well as the peripheral section
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.