Podcast
Questions and Answers
Which cellular classification is characterized by a quiescent state under normal physiological conditions, yet retains the capacity for proliferation in response to specific stimuli?
Which cellular classification is characterized by a quiescent state under normal physiological conditions, yet retains the capacity for proliferation in response to specific stimuli?
- Stable cells, including hepatocytes and renal tubular cells, that can re-enter the cell cycle when triggered by injury or growth factors. (correct)
- Labile cells, exemplified by the continuous turnover observed in the stratified squamous epithelium of the skin.
- Permanent cells, such as cardiomyocytes and neurons, which are terminally differentiated and incapable of mitotic division.
- Transient amplifying cells, which undergo rapid proliferation for a limited number of divisions before differentiating permanently.
What is the crucial distinction between regeneration and repair by fibrosis following tissue injury, focusing on the restoration of structural and functional integrity?
What is the crucial distinction between regeneration and repair by fibrosis following tissue injury, focusing on the restoration of structural and functional integrity?
- Regeneration results in complete restoration of the original tissue architecture and function, while repair by fibrosis leads to scar formation and potential functional impairment. (correct)
- Regeneration is primarily mediated by inflammatory cells, whereas repair by fibrosis is driven by resident fibroblasts and myofibroblasts.
- Regeneration involves the replacement of damaged tissue with undifferentiated stem cells, whereas repair by fibrosis relies on the deposition of extracellular matrix.
- Regeneration occurs exclusively in tissues with high proliferative capacity, whereas repair by fibrosis is the default response in tissues with limited regenerative potential.
What are the principal cellular and molecular components orchestrating the deposition and remodeling of the extracellular matrix during granulation tissue formation, subsequent to acute tissue injury?
What are the principal cellular and molecular components orchestrating the deposition and remodeling of the extracellular matrix during granulation tissue formation, subsequent to acute tissue injury?
- Lymphocytes producing cytokines to inhibit fibroblast proliferation, coupled with endothelial cells forming new capillaries via vasculogenesis.
- Eosinophils releasing major basic protein to cross-link collagen fibers, synergistically with keratinocytes migrating to re-epithelialize the wound surface.
- Neutrophils releasing reactive oxygen species to degrade damaged collagen, alongside mast cells secreting histamine to enhance vascular permeability.
- Macrophages secreting matrix metalloproteinases (MMPs) to degrade provisional matrix, concurrently with fibroblasts synthesizing collagen types I and III. (correct)
Which statement accurately describes the biomechanical and compositional evolution of granulation tissue during the transition from its nascent formation to a mature scar?
Which statement accurately describes the biomechanical and compositional evolution of granulation tissue during the transition from its nascent formation to a mature scar?
In the context of 'healing by primary intention,' what are the cardinal features that critically influence the spatiotemporal progression of tissue repair?
In the context of 'healing by primary intention,' what are the cardinal features that critically influence the spatiotemporal progression of tissue repair?
How does 'healing by secondary intention' diverge mechanistically and clinically from 'healing by primary intention,' emphasizing the contrasting roles of inflammation, matrix deposition, and wound contraction?
How does 'healing by secondary intention' diverge mechanistically and clinically from 'healing by primary intention,' emphasizing the contrasting roles of inflammation, matrix deposition, and wound contraction?
Which local factor exerts the most profound influence on the kinetics and quality of wound healing, considering the interplay between tissue perfusion, oxygen tension, and growth factor bioavailability?
Which local factor exerts the most profound influence on the kinetics and quality of wound healing, considering the interplay between tissue perfusion, oxygen tension, and growth factor bioavailability?
What is the role of systemic factors in modulating the wound healing process, considering the complex interactions between metabolic status, immune competence, and pharmacological interventions?
What is the role of systemic factors in modulating the wound healing process, considering the complex interactions between metabolic status, immune competence, and pharmacological interventions?
Which statement accurately differentiates a sinus from a fistula in the context of wound healing complications, regarding their anatomical connections and pathological significance?
Which statement accurately differentiates a sinus from a fistula in the context of wound healing complications, regarding their anatomical connections and pathological significance?
What is the distinct pathological mechanism underlying keloid formation compared to hypertrophic scar formation, emphasizing the role of aberrant collagen synthesis and matrix remodeling?
What is the distinct pathological mechanism underlying keloid formation compared to hypertrophic scar formation, emphasizing the role of aberrant collagen synthesis and matrix remodeling?
In the pathogenesis of squamous cell carcinoma arising as a complication of chronic wounds, what is the etiological basis and cellular transformation process?
In the pathogenesis of squamous cell carcinoma arising as a complication of chronic wounds, what is the etiological basis and cellular transformation process?
How do local infections impair the orderly progression of wound healing?
How do local infections impair the orderly progression of wound healing?
A patient develops an incisional hernia following abdominal surgery. What is the primary mechanism?
A patient develops an incisional hernia following abdominal surgery. What is the primary mechanism?
What is the significance of collagen type III in early granulation tissue, elucidating its functional role before its eventual replacement by collagen type I?
What is the significance of collagen type III in early granulation tissue, elucidating its functional role before its eventual replacement by collagen type I?
Following a deep partial-thickness burn injury, what are the key cellular and molecular events that dictate whether the wound heals primarily through re-epithelialization or progresses to scar formation, considering the depth of dermal involvement and inflammatory milieu?
Following a deep partial-thickness burn injury, what are the key cellular and molecular events that dictate whether the wound heals primarily through re-epithelialization or progresses to scar formation, considering the depth of dermal involvement and inflammatory milieu?
How do corticosteroids impede wound healing at the molecular level, focusing on their impact on growth factor signaling, collagen synthesis, and inflammatory cell function?
How do corticosteroids impede wound healing at the molecular level, focusing on their impact on growth factor signaling, collagen synthesis, and inflammatory cell function?
What is the role of myofibroblasts in wound contraction?
What is the role of myofibroblasts in wound contraction?
Which nutritional deficiency most significantly impairs wound healing, considering the diverse roles of micronutrients and macronutrients in cellular metabolism, matrix synthesis, and immune function?
Which nutritional deficiency most significantly impairs wound healing, considering the diverse roles of micronutrients and macronutrients in cellular metabolism, matrix synthesis, and immune function?
What are the implications of cicatrization on flexure points?
What are the implications of cicatrization on flexure points?
An epidermal cyst develops within a healing wound. What is the underlying pathological process?
An epidermal cyst develops within a healing wound. What is the underlying pathological process?
Flashcards
Definition of Repair
Definition of Repair
Replacement of damaged tissue by living tissue.
Regeneration
Regeneration
Replacement of destroyed tissue by the same cells.
Labile Cells
Labile Cells
Cells with a good power of continuous proliferation to replace aging cells.
Stable Cells
Stable Cells
Signup and view all the flashcards
Permanent Cells
Permanent Cells
Signup and view all the flashcards
Repair by Fibrosis
Repair by Fibrosis
Signup and view all the flashcards
Granulation Tissue
Granulation Tissue
Signup and view all the flashcards
Healing by Primary Intention
Healing by Primary Intention
Signup and view all the flashcards
Healing by Secondary Intention
Healing by Secondary Intention
Signup and view all the flashcards
Sinus (Wound Healing)
Sinus (Wound Healing)
Signup and view all the flashcards
Fistula (Wound Healing)
Fistula (Wound Healing)
Signup and view all the flashcards
Ulcer
Ulcer
Signup and view all the flashcards
Keloid
Keloid
Signup and view all the flashcards
Study Notes
- Repair refers to the replacement of damaged tissue by living tissue
Repair Types
- Regeneration replaces destroyed tissue with the same cells
- Repair by fibrosis replaces destroyed tissue with granulation tissue, which matures into fibrosis
Cell Proliferation Capacity
- Cells are classified by their proliferative capacity
- Labile cells have a good, continuous power of proliferation to replace aging cells
- Examples of labile cells are stratified squamous epithelium of skin and columnar epithelium of the GIT
- Stable cells do not proliferate under normal conditions, but will when needed
- Parenchymatous cells (liver, pancreas, renal tubules) & Mesenchymal cells (fibroblasts, chondroblasts, osteoblasts) are types of stable cells
- Permanent cells cannot proliferate at all
- Muscle cells and nerve cells are permanent cells
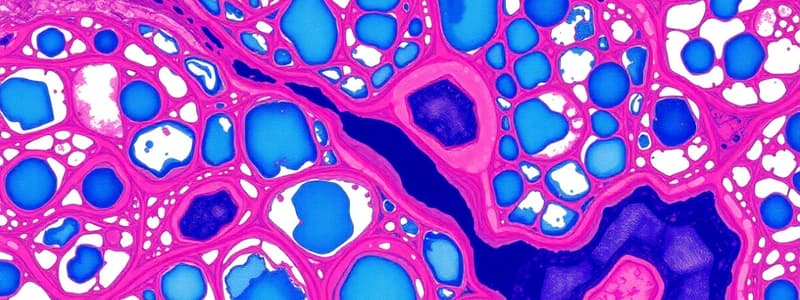
Granulation Tissue
- Granulation tissue is red, granular, soft, painless, and bleeds easily
- It forms in the gap of healing wounds
- Granulation tissue consists of fibroblasts surrounded by collagen, newly formed blood vessels, scattered macrophages, and some other inflammatory cells
- Scar formation occurs after excess collagen deposition and obliteration of the capillaries
Characteristics of Granulation Tissue
- Light red or dark pink in color due to perfusion with new capillary loops
- Soft to the touch
- Moist and granular in appearance because of punctate hemorrhages
- Pulsatile on palpation
- Painless when healthy
Wound Healing by Primary Intention
- Occurs in clean surgical wounds with minimal tissue destruction, minimal bleeding, no bacterial infection, and good apposition of wound edges
Steps of Healing by Primary Intention
- Initial hemorrhage fills the wound cavity with a blood clot
- Inflammation occurs within 24 hours, and PNLs infiltrate the blood clot
- Epithelial changes occur within 48 hours as epithelial cells from wound edges proliferate
- Early granulation tissue forms on the 3rd day when macrophages replace PNLs
- Macrophages stimulate the ingrowth of fibroblasts and angioblasts, which start forming collagen type III
- Epidermal cells form a bridge that seals off the defect
- Fully developed granulation tissue occurs in 4–6 days causing neovascularization, and the granulation tissue fills the wound gap
- Scar formation occurs during the 2nd week as inflammation subsides with fibroblastic proliferation and collagen deposition continues
- Remodeling of the scar occurs by the end of the 1st month
Healing by Secondary Intention
- Occurs in gaping wounds with marked tissue destruction, bleeding and infection, and poor apposition of wound edges
- Healing by secondary intention follows the same steps as primary intention
- The inflammatory response is greater in secondary intention
- Formation of abundant granulation tissue occurs
- Epithelization takes more time, depending on the wound gap
- Excessive fibrosis and wound contraction happens
- There is more liability to infection and complications
Factors Affecting Wound Healing
- Local factors include size and site of the wound, infection, foreign bodies, and blood supply to the area
- Systemic factors include age, nutritional disorders (anemia and malnutrition), metabolic disorders, chronic debilitating diseases, diabetes, and drugs (steroids and cytotoxic drugs)
Complications of Wound Healing
- Infection
- Sinus: blind duct lined by epithelium between the wound and external surface
- Fistula: duct lined by epithelium between the wound and a hollow organ
- Ulcer: loss of continuity of surface epithelium
- Keloid: excessive granulation tissue and scar formation
- Incisional hernia
- Cicatrization: scar on flexures interferes with movement
- Implantation (epidermal) cyst
- Malignant transformation: squamous cell carcinoma
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.