Podcast
Questions and Answers
What is the primary role of fibroblasts in the process of fibrosis?
What is the primary role of fibroblasts in the process of fibrosis?
- Secretion of inflammatory cytokines
- Formation of new endothelial cells
- Remodeling the extracellular matrix
- Migration and proliferation into injured tissue (correct)
Which growth factor is primarily secreted by macrophages during the proliferative phase of fibrosis?
Which growth factor is primarily secreted by macrophages during the proliferative phase of fibrosis?
- Vascular Endothelial Growth Factor (VEGF)
- Epidermal Growth Factor (EGF)
- Transforming Growth Factor-beta (TGF-beta) (correct)
- Fibroblast Growth Factor (FGF)
What are the initial processes involved in tissue repair by fibrosis?
What are the initial processes involved in tissue repair by fibrosis?
- Scar formation and local tissue inflammation
- Deposition of collagen and ECM remodeling
- Migration of macrophages and endothelial cells
- Formation of new blood vessels and fibroblast proliferation (correct)
What is the main function of angioblasts in the context of angiogenesis?
What is the main function of angioblasts in the context of angiogenesis?
What is the final phase of fibrosis that involves reshaping the extracellular matrix?
What is the final phase of fibrosis that involves reshaping the extracellular matrix?
Which factor primarily influences the scar formation phase in tissue repair by fibrosis?
Which factor primarily influences the scar formation phase in tissue repair by fibrosis?
What is the role of angiogenesis in the repair of injured tissues?
What is the role of angiogenesis in the repair of injured tissues?
Which of the following best describes the role of local factors in wound healing?
Which of the following best describes the role of local factors in wound healing?
What distinguishes the process of fibrosis from normal tissue regeneration?
What distinguishes the process of fibrosis from normal tissue regeneration?
What characterizes the late response in wound healing after 4 weeks?
What characterizes the late response in wound healing after 4 weeks?
Which statement is true regarding fibroblast activity during the deposition of the extracellular matrix?
Which statement is true regarding fibroblast activity during the deposition of the extracellular matrix?
What is the primary goal of suturing wounds during healing?
What is the primary goal of suturing wounds during healing?
Which phase of wound healing follows inflammation and involves re-epithelialization?
Which phase of wound healing follows inflammation and involves re-epithelialization?
In the context of wound healing by secondary intention, which characteristic is most accurate?
In the context of wound healing by secondary intention, which characteristic is most accurate?
What is the role of growth factors in tissue and organ regeneration?
What is the role of growth factors in tissue and organ regeneration?
What is the primary difference between primary and secondary union in wound healing?
What is the primary difference between primary and secondary union in wound healing?
Which aspect is NOT a feature of the maturation phase of wound healing?
Which aspect is NOT a feature of the maturation phase of wound healing?
What accurately describes granulation tissue during the early response phase of wound healing?
What accurately describes granulation tissue during the early response phase of wound healing?
The balance between extracellular matrix synthesis and degradation is critically maintained during which phase of healing?
The balance between extracellular matrix synthesis and degradation is critically maintained during which phase of healing?
Which collagen type is primarily involved during the inflammation phase of wound healing?
Which collagen type is primarily involved during the inflammation phase of wound healing?
What percentage of normal wound strength is achieved by day 10 following a deep clean laceration?
What percentage of normal wound strength is achieved by day 10 following a deep clean laceration?
Which systemic factor is known to inhibit collagen synthesis in wound healing?
Which systemic factor is known to inhibit collagen synthesis in wound healing?
What is the main characteristic of the maturation phase of wound healing?
What is the main characteristic of the maturation phase of wound healing?
How does diabetes mellitus affect wound healing?
How does diabetes mellitus affect wound healing?
What primarily dictates the accumulation of collagen type I in wound healing beyond day 10?
What primarily dictates the accumulation of collagen type I in wound healing beyond day 10?
Which condition is known to limit blood supply and therefore slow down wound healing?
Which condition is known to limit blood supply and therefore slow down wound healing?
In which tissue repair process is pathologic repair primarily indicated?
In which tissue repair process is pathologic repair primarily indicated?
Which hormone is known to inhibit wound healing but may be beneficial in certain circumstances?
Which hormone is known to inhibit wound healing but may be beneficial in certain circumstances?
Which type of suturing technique is best described as approximating the edges of the dermis in a deep clean laceration?
Which type of suturing technique is best described as approximating the edges of the dermis in a deep clean laceration?
What is the primary outcome of regeneration after acute injury?
What is the primary outcome of regeneration after acute injury?
Which of the following processes is NOT associated with persistent tissue damage?
Which of the following processes is NOT associated with persistent tissue damage?
What primarily contributes to the increased synthesis of collagen during chronic inflammation?
What primarily contributes to the increased synthesis of collagen during chronic inflammation?
Which immune cells are notably activated during chronic inflammation?
Which immune cells are notably activated during chronic inflammation?
What effect do cytokines have in the context of chronic inflammation?
What effect do cytokines have in the context of chronic inflammation?
How does fibrosis primarily differ from regeneration following injury?
How does fibrosis primarily differ from regeneration following injury?
Which factor is identified as the single most important cause of delayed wound healing?
Which factor is identified as the single most important cause of delayed wound healing?
What effect does the presence of foreign bodies have on wound healing?
What effect does the presence of foreign bodies have on wound healing?
Which type of wound is likely to heal the fastest?
Which type of wound is likely to heal the fastest?
What is the primary cause of wound dehiscence?
What is the primary cause of wound dehiscence?
Keloids are characterized by which of the following features?
Keloids are characterized by which of the following features?
Which sites are likely to heal the fastest due to their vascularity?
Which sites are likely to heal the fastest due to their vascularity?
What phenomenon occurs primarily in large surface wounds that heal by secondary union?
What phenomenon occurs primarily in large surface wounds that heal by secondary union?
Excessive wound contraction can lead to which of the following deformities?
Excessive wound contraction can lead to which of the following deformities?
Which condition is a common underlying cause of chronic ulceration?
Which condition is a common underlying cause of chronic ulceration?
What is a key distinction between hypertrophic scars and keloids?
What is a key distinction between hypertrophic scars and keloids?
Flashcards are hidden until you start studying
Study Notes
Tissue Repair: A Look at the Processes Involved
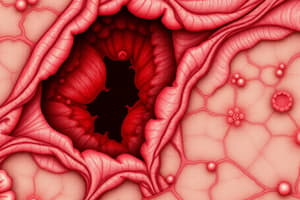
- Fibrosis: A process of tissue repair through collagen and ECM deposition, forming a scar. This occurs when tissue damage is severe or chronic, preventing regeneration by parenchymal cells alone.
- Phases of Fibrosis:
- Inflammation: Removal of dead or damaged cells.
- Angiogenesis: Formation of new blood vessels.
- Fibroblast migration and proliferation: Fibroblasts migrate to the injury site and multiply.
- ECM deposition: Fibroblasts become more synthetic, producing collagen and other ECM components.
- Connective tissue remodeling: A balance between ECM synthesis and degradation, leading to increased tensile strength.
- Angiogenesis Mechanisms:
- Sprouting: New vessels sprout from existing vessels.
- Angioblast-like endothelial-precursor cells (EPCs): Cells from bone marrow migrate to the site of angiogenesis.
Wound Healing: First and Second Intention
-
First Intention (Primary Union):
- Minor damage to keratinocytes and dermal cells with a minimal rupture of the basement membrane.
- Example: Surgical incision.
- Result: Thin fibrous union.
-
Second Intention (Secondary Union):
- Large defects require more inflammation, granulation tissue, collagen deposition, and wound contraction.
- Example: Deep traumatic abrasion.
- Result: Wide scar with potential for skin depression or contraction.
Wound Healing Phases: A Detailed Look
- Inflammation:
- Blood clot formation.
- Chemotaxis of immune cells to the wound site.
- Proliferation:
- Epithelialization: Restoration of the skin surface.
- Angiogenesis: New blood vessel formation.
- Granulation tissue formation: A mixture of fibroblasts, collagen, and blood vessels.
- Provisional matrix formation: A temporary ECM that supports the healing process.
- Maturation:
- Collagen deposition: Continued accumulation of Type I collagen.
- Collagen matrix remodeling: Formation of a strong and organized collagen network.
- Wound contraction: Myofibroblasts pull the wound edges together.
Factors Influencing Wound Healing
-
Systemic Factors:
- Nutrition: Protein and vitamin C deficiency inhibit collagen synthesis.
- Metabolic status: Diabetes mellitus delays healing due to insulin's role in nucleic acid and protein synthesis.
- Circulatory status: Insufficient blood supply due to conditions like arterial atherosclerosis or venous stasis slows down healing.
- Steroid hormones: Glucocorticoids inhibit healing but can be beneficial in certain areas, such as the eye.
-
Local Factors:
- Infection: Persistent inflammation caused by infection is a major factor in delayed healing.
- Mechanical: Early tension on the wound may separate edges, delaying healing.
- Foreign bodies: Material like metal, glass, wood, or bone prolong inflammation and hinder healing.
- Anatomic location: Sites with rich vascularity (face) heal faster than sites with reduced vascularity (foot).
- Type of wound: Sharp incisions (surgical) heal faster than larger wounds (traumatic deep abrasion).
Pathologic Wound Repair: When Healing Goes Wrong
-
Deficient Scar Formation:
- Wound dehiscence: Separation of wound edges due to forces like vomiting or coughing.
- Wound necrosis: Death of tissue due to infection or inadequate blood supply.
-
Excessive Repair:
- Hypertrophic scar: Excess collagen deposition, raised and itchy, but stays within the boundaries of the original wound.
- Keloid: Excess collagen deposition extending beyond the original wound boundaries, often with genetic predisposition.
-
Contracture Formation:
- Deformity caused by excessive wound contraction, often seen after burns.
Chronic Ulceration: A Persistent Wound
- Arterial atherosclerosis: Compromised blood flow leading to chronic ulceration, especially in the lower extremities.
- Venous stasis: Reduced venous return to the heart, also leading to chronic ulceration.
Summary: Responses After Injury and Inflammation
- Cellular and vascular responses:
- Stimulus removal (acute injury):
- Parenchymal cell death (intact tissue framework) - Regeneration: Restitution of normal structure.
- Persistent tissue damage:
- Parenchymal cell death (damaged tissue framework) - Repair: Scar formation.
- Fibrosis: Tissue scar (chronic inflammatory diseases).
- Stimulus removal (acute injury):
Fibrosis: An Ongoing Process
- Persistent stimulus (chronic inflammation):
- Macrophage and lymphocyte activation:
- Growth factors: PDGF, FGF, TGF-β.
- Cytokines: TNF, IL-1, IL-4, IL-13.
- Reduced metalloproteinase activity.
- Increased proliferation of fibroblasts, endothelial cells, and specialized fibrogenic cells.
- Increased collagen synthesis and decreased collagen degradation.
- Ultimately leading to fibrosis.
- Macrophage and lymphocyte activation:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.