Podcast
Questions and Answers
Following tissue injury, which process is the FIRST to occur and is essential for initiating the subsequent phases of tissue repair?
Following tissue injury, which process is the FIRST to occur and is essential for initiating the subsequent phases of tissue repair?
- Recruitment of fibroblasts to begin synthesizing extracellular matrix proteins.
- Coagulation and platelet activation to control bleeding and initiate the formation of a fibrin clot. (correct)
- Angiogenesis to re-establish blood supply to the damaged area.
- Stem cell proliferation and differentiation to replace damaged cells.
What is the primary role of myofibroblasts in tissue repair, and how do they contribute to the overall process?
What is the primary role of myofibroblasts in tissue repair, and how do they contribute to the overall process?
- Secreting growth factors that stimulate the proliferation of epithelial cells.
- Synthesizing collagen type III to form the initial scaffolding of granulation tissue.
- Exerting contractile forces to reduce wound size and facilitate tissue remodeling. (correct)
- Recruiting inflammatory cells to clear debris and prevent infection at the wound site.
How does Transforming Growth Factor beta (TGF-β) influence the fibrotic response in tissue repair, and what is its net effect on extracellular matrix remodeling?
How does Transforming Growth Factor beta (TGF-β) influence the fibrotic response in tissue repair, and what is its net effect on extracellular matrix remodeling?
- It promotes the breakdown of collagen and other extracellular matrix components by stimulating metalloproteinase activity.
- It stimulates fibroblast migration and proliferation, increases collagen and fibronectin synthesis, and inhibits metalloproteinases, leading to increased fibrosis. (correct)
- It inhibits fibroblast migration and proliferation, leading to reduced collagen synthesis and decreased fibrosis.
- It recruits inflammatory cells to the site of injury, which indirectly promotes extracellular matrix remodeling by releasing reactive oxygen species.
What is the function of angiogenesis in tissue repair, and how is it regulated to ensure proper vessel formation without excessive proliferation?
What is the function of angiogenesis in tissue repair, and how is it regulated to ensure proper vessel formation without excessive proliferation?
In the context of tissue regeneration and repair, what determines whether a damaged tissue will undergo complete restoration versus scar formation?
In the context of tissue regeneration and repair, what determines whether a damaged tissue will undergo complete restoration versus scar formation?
How do growth factors and cytokines secreted by inflammatory cells, particularly macrophages, influence the progression of tissue repair, and what specific roles do they play?
How do growth factors and cytokines secreted by inflammatory cells, particularly macrophages, influence the progression of tissue repair, and what specific roles do they play?
What is the significance of the transition from collagen type III to collagen type I during the remodeling phase of tissue repair, and how does this transition affect tissue strength and function?
What is the significance of the transition from collagen type III to collagen type I during the remodeling phase of tissue repair, and how does this transition affect tissue strength and function?
How do matrix metalloproteinases (MMPs) contribute to tissue remodeling, and how is their activity regulated to prevent excessive matrix degradation?
How do matrix metalloproteinases (MMPs) contribute to tissue remodeling, and how is their activity regulated to prevent excessive matrix degradation?
Considering the sequence of events in tissue repair, what is the correct order of phases, and how would you categorize them based on their primary functions?
Considering the sequence of events in tissue repair, what is the correct order of phases, and how would you categorize them based on their primary functions?
How can chronic inflammation impair tissue regeneration and lead to excessive fibrosis, and what cellular and molecular mechanisms are involved?
How can chronic inflammation impair tissue regeneration and lead to excessive fibrosis, and what cellular and molecular mechanisms are involved?
Flashcards
Regeneration
Regeneration
Occurs in cells with high proliferative capacity, such as skin, intestines, and liver.
Connective Tissue Components
Connective Tissue Components
Blood vessels contribute to angiogenesis; fibroblasts produce extracellular matrix proteins like collagen.
Myofibroblasts
Myofibroblasts
Specialized fibroblasts with contractile properties.
Collagen Type One
Collagen Type One
Signup and view all the flashcards
Tissue Injury Response (Initial Phase)
Tissue Injury Response (Initial Phase)
Signup and view all the flashcards
Regeneration Phase
Regeneration Phase
Signup and view all the flashcards
Tissue Remodeling
Tissue Remodeling
Signup and view all the flashcards
Tissue Repair Timeframe
Tissue Repair Timeframe
Signup and view all the flashcards
Platelet-Derived & Fibroblast Growth Factors
Platelet-Derived & Fibroblast Growth Factors
Signup and view all the flashcards
TGF-beta
TGF-beta
Signup and view all the flashcards
Study Notes
- Repair, healing, and resolution are interchangeable terms.
- Regeneration occurs in cells with high proliferative capacity (e.g., skin, intestines, liver).
Connective Tissue Components
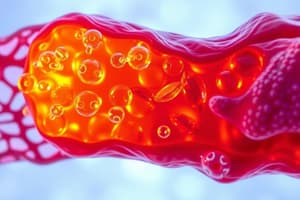
- Blood vessels contribute to angiogenesis.
- Fibroblasts produce extracellular matrix proteins (collagen, elastin, proteoglycans).
- Myofibroblasts are specialized fibroblasts with contractile properties.
- Collagen type one has high tensile strength.
- Collagen type three is found in reticular connective tissue and granulation tissue, forming a template for healing and scarring.
Phases of Tissue Regeneration and Repair
- Tissue Injury: Coagulation factors and platelets fill the defect and stop the bleed. Inflammatory cells (neutrophils, macrophages) fight potential infection.
- Regeneration Phase (days to weeks): Stem cell proliferation and differentiation occur. Connective tissue is laid down (dermis in the skin). Granulation tissue forms a scaffolding template. Angiogenesis occurs, and epithelial cells proliferate to bridge the gap.
- Remodeling Phase (one month onward): New cells fill the void. Collagen type three is converted to collagen type one (higher tensile strength).
Timeline of Tissue Regeneration
- One Day: Tissue injury and inflammation.
- One Week: Recruitment of materials for tissue repair (macrophages, secretions, angiogenesis).
- One Month: Remodeling phase, new cells have come in and replaced old, and remodeled end product.
Cellular Activity
- Cell migration, proliferation of fibroblasts, and deposition of extracellular matrix proteins (collagen) occur.
- Macrophages secrete growth factors and cytokines.
- Key players are macrophages and fibroblasts.
- Platelet-derived growth factor and fibroblast growth factor promote collagen and fibroblast proliferation.
- Tissue growth factor beta (TGF-β) stimulates fibroblast migration and proliferation, increases collagen and fibronectin synthesis, and inhibits metalloproteinases, contributing to fibrosis and scarring.
- Metalloproteinases break down extracellular matrix; their inhibition helps build tissue.
- Fibroblast growth factor recruits perivascular cells and smooth muscle cells. Endothelial proliferation is suppressed as new vessels form and basal lamina is deposited.
Recap of Tissue Repair
- Inflammation, regeneration/remodeling, and tissue repair are sequential steps.
- One Day: Inflammation and blood clot form.
- Up to Seven Days: Accumulation of materials, start of angiogenesis, and remodeling with granulation tissue formation, increased fibroblastic proliferation and collagen type three production. Collagen type three is replaced by collagen type one over time.
- Epithelial regeneration may occur depending on the organ involved.
- By One Month and Beyond: The end product can be regeneration (restoration of tissue) or scar formation.
- Lack of regenerative properties leads to scar formation. Increased collagen deposition leads to fibrosis and scarring.
- If regeneration is not possible, a scar will form.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.