Podcast
Questions and Answers
The thyroid gland originates from which embryonic tissue?
The thyroid gland originates from which embryonic tissue?
- Mesoderm
- Ectoderm
- Endoderm (correct)
- Neural crest
At what point during gestation does the thyroid gland begin to function?
At what point during gestation does the thyroid gland begin to function?
- End of the second trimester
- End of the first trimester
- Beginning of the second trimester (correct)
- Beginning of the third trimester
The foramen cecum is an important anatomical landmark in the development of the thyroid gland. Where is it located?
The foramen cecum is an important anatomical landmark in the development of the thyroid gland. Where is it located?
- The floor of the embryonic pharynx at the junction of the anterior 2/3 and posterior 1/3 of the developing tongue (correct)
- The posterior aspect of the cricoid cartilage
- The anterior aspect of the larynx
- Within the developing esophagus
What is the fate of the thyroglossal duct after thyroid gland development?
What is the fate of the thyroglossal duct after thyroid gland development?
Which of the following best describes a thyroglossal cyst?
Which of the following best describes a thyroglossal cyst?
During the surgical removal of a thyroglossal cyst, why is it important to also remove a portion of the hyoid bone?
During the surgical removal of a thyroglossal cyst, why is it important to also remove a portion of the hyoid bone?
The occasional levator glandulae thyroideae is a fibromuscular slip that may attach the pyramidal lobe to which structure?
The occasional levator glandulae thyroideae is a fibromuscular slip that may attach the pyramidal lobe to which structure?
In a normal adult, what is the approximate average weight of the thyroid gland?
In a normal adult, what is the approximate average weight of the thyroid gland?
Which of the following best describes the location of the apex of each thyroid lobe?
Which of the following best describes the location of the apex of each thyroid lobe?
At which vertebral level does the base of the thyroid gland typically lie?
At which vertebral level does the base of the thyroid gland typically lie?
Where is the isthmus of the thyroid gland typically located?
Where is the isthmus of the thyroid gland typically located?
Why does an enlarged thyroid gland typically shift downward into the superior mediastinum rather than upward?
Why does an enlarged thyroid gland typically shift downward into the superior mediastinum rather than upward?
Which structure is derived from the pretracheal layer of the deep cervical fascia?
Which structure is derived from the pretracheal layer of the deep cervical fascia?
What clinical significance does the venous plexus lying deep to the true capsule of the thyroid gland have during thyroid surgery?
What clinical significance does the venous plexus lying deep to the true capsule of the thyroid gland have during thyroid surgery?
The movement of the thyroid gland during swallowing is primarily due to the attachment of the pretracheal fascia to which structures?
The movement of the thyroid gland during swallowing is primarily due to the attachment of the pretracheal fascia to which structures?
Where is the suspensory ligament of Berry located, and what is its significance during thyroid surgery?
Where is the suspensory ligament of Berry located, and what is its significance during thyroid surgery?
Which of the following structures lies immediately behind the cricothyroid joint and the ligament of Berry?
Which of the following structures lies immediately behind the cricothyroid joint and the ligament of Berry?
Describe the anterior relations of each lobe of the thyroid gland.
Describe the anterior relations of each lobe of the thyroid gland.
The superior thyroid artery is a branch of which artery?
The superior thyroid artery is a branch of which artery?
The inferior thyroid artery typically arises from which of the following?
The inferior thyroid artery typically arises from which of the following?
Why is it generally safer to ligate the inferior thyroid artery away from the lower pole of the gland during surgery?
Why is it generally safer to ligate the inferior thyroid artery away from the lower pole of the gland during surgery?
Which arteries typically supply the anterior surface of the thyroid isthmus?
Which arteries typically supply the anterior surface of the thyroid isthmus?
Which vein does not directly drain into the internal jugular vein?
Which vein does not directly drain into the internal jugular vein?
Where do the initial lymphatic vessels from the upper part of the thyroid gland drain?
Where do the initial lymphatic vessels from the upper part of the thyroid gland drain?
Which of the following best describes the function of thyroid scans using radioactive iodine?
Which of the following best describes the function of thyroid scans using radioactive iodine?
The thyroid gland begins its functional activity during gestation in which month?
The thyroid gland begins its functional activity during gestation in which month?
From which of the following does the thyroid gland originate during embryonic development?
From which of the following does the thyroid gland originate during embryonic development?
A midline foramen at the junction of the anterior 2/3 and posterior 1/3 of the developing tongue is known as what?
A midline foramen at the junction of the anterior 2/3 and posterior 1/3 of the developing tongue is known as what?
The bilobed lower end of the thyroglossal duct gives rise to which of the following?
The bilobed lower end of the thyroglossal duct gives rise to which of the following?
Failure of the thyroglossal duct to descend can result in ectopic thyroid tissue located where?
Failure of the thyroglossal duct to descend can result in ectopic thyroid tissue located where?
During surgical removal of a thyroglossal cyst, the body of the hyoid bone is also removed to prevent what?
During surgical removal of a thyroglossal cyst, the body of the hyoid bone is also removed to prevent what?
What is the average weight of the adult thyroid gland?
What is the average weight of the adult thyroid gland?
Which anatomical structure lies opposite the apex of each thyroid lobe?
Which anatomical structure lies opposite the apex of each thyroid lobe?
The base of the thyroid gland typically lies at which vertebral level?
The base of the thyroid gland typically lies at which vertebral level?
At which vertebral level does the isthmus of the thyroid gland typically lie?
At which vertebral level does the isthmus of the thyroid gland typically lie?
The pretracheal fascia attaches superiorly to what?
The pretracheal fascia attaches superiorly to what?
Movements of the thyroid during swallowing (deglutition) and speech are due to the attachments of the pretracheal fascia to which structures?
Movements of the thyroid during swallowing (deglutition) and speech are due to the attachments of the pretracheal fascia to which structures?
The anterior border of the thyroid gland is related to which structure?
The anterior border of the thyroid gland is related to which structure?
What anatomical relationship does the superior pole of the thyroid gland have with the thyrohyoid muscle?
What anatomical relationship does the superior pole of the thyroid gland have with the thyrohyoid muscle?
Which vessels supply twigs to the anterior surface of the thyroid isthmus?
Which vessels supply twigs to the anterior surface of the thyroid isthmus?
What lies immediately behind the cricothyroid joint and the ligament of Berry?
What lies immediately behind the cricothyroid joint and the ligament of Berry?
Which arteries accompany the external laryngeal nerve, and descends to the superior pole of the lateral lobe of the gland?
Which arteries accompany the external laryngeal nerve, and descends to the superior pole of the lateral lobe of the gland?
Why is it safer to tie the inferior thyroid artery away from the lower pole of the gland, during thyroidectomy?
Why is it safer to tie the inferior thyroid artery away from the lower pole of the gland, during thyroidectomy?
Which of the pairs of veins that drains the thyroid gland drains directly into the left brachiocephalic vein?
Which of the pairs of veins that drains the thyroid gland drains directly into the left brachiocephalic vein?
Lymphatic vessels from the thyroid gland drain into which nodes?
Lymphatic vessels from the thyroid gland drain into which nodes?
The presence of the thyroid isthmus and associated vessels may cause difficulty in performing what procedure?
The presence of the thyroid isthmus and associated vessels may cause difficulty in performing what procedure?
During thyroid surgery, inadvertent removal of parathyroid glands or injury to their arterial supply may lead to what?
During thyroid surgery, inadvertent removal of parathyroid glands or injury to their arterial supply may lead to what?
A congenital anomaly in which the right recurrent laryngeal nerve arises non recurrently from the right vagus nerve higher up in the neck is due to what?
A congenital anomaly in which the right recurrent laryngeal nerve arises non recurrently from the right vagus nerve higher up in the neck is due to what?
Which of the following statements accurately describes thyroid hormone synthesis?
Which of the following statements accurately describes thyroid hormone synthesis?
Flashcards
Thyroid gland development
Thyroid gland development
Thyroid gland development begins in the 4th month of intrauterine life.
Foramen cecum
Foramen cecum
A midline foramen at the junction of the anterior 2/3 and posterior 1/3 of the developing tongue.
Origin of thyroglossal duct
Origin of thyroglossal duct
Arises from the endoderm of the embryonic pharynx floor at the foramen cecum.
Cranial end fate
Cranial end fate
Signup and view all the flashcards
Pyramidal lobe
Pyramidal lobe
Signup and view all the flashcards
Thyroglossal cyst
Thyroglossal cyst
Signup and view all the flashcards
Thyroglossal cyst removal
Thyroglossal cyst removal
Signup and view all the flashcards
Thyroid isthmus
Thyroid isthmus
Signup and view all the flashcards
Each thyroid lobe
Each thyroid lobe
Signup and view all the flashcards
Vertebral level
Vertebral level
Signup and view all the flashcards
True capsule (fibrous)
True capsule (fibrous)
Signup and view all the flashcards
False capsule (fascial)
False capsule (fascial)
Signup and view all the flashcards
Importance
Importance
Signup and view all the flashcards
Suspensory ligament of Berry
Suspensory ligament of Berry
Signup and view all the flashcards
Relation to sternothyroid
Relation to sternothyroid
Signup and view all the flashcards
Palpation of the lobes
Palpation of the lobes
Signup and view all the flashcards
Palpation of the isthmus
Palpation of the isthmus
Signup and view all the flashcards
Thyroid gland supplied by
Thyroid gland supplied by
Signup and view all the flashcards
Superior Thyroid Arteries Descend
Superior Thyroid Arteries Descend
Signup and view all the flashcards
Inferior Thyroid Arteries.
Inferior Thyroid Arteries.
Signup and view all the flashcards
Accessory thyroid arteries
Accessory thyroid arteries
Signup and view all the flashcards
Thyroid arteries size
Thyroid arteries size
Signup and view all the flashcards
Arise from venous plexus
Arise from venous plexus
Signup and view all the flashcards
Lymphatics drainage
Lymphatics drainage
Signup and view all the flashcards
Thyroid scan
Thyroid scan
Signup and view all the flashcards
Thyroglossal Duct Course
Thyroglossal Duct Course
Signup and view all the flashcards
Derivatives
Derivatives
Signup and view all the flashcards
Caudal Pharyngeal Complex
Caudal Pharyngeal Complex
Signup and view all the flashcards
Lingual thyroid
Lingual thyroid
Signup and view all the flashcards
Thyroid gland
Thyroid gland
Signup and view all the flashcards
Thyroid Lobe Dimensions
Thyroid Lobe Dimensions
Signup and view all the flashcards
Cause of Arrest
Cause of Arrest
Signup and view all the flashcards
Downward shift
Downward shift
Signup and view all the flashcards
Anterior and Posterior border
Anterior and Posterior border
Signup and view all the flashcards
Superficial Surface
Superficial Surface
Signup and view all the flashcards
Tubes
Tubes
Signup and view all the flashcards
Medial Surface
Medial Surface
Signup and view all the flashcards
Carotid sheath contents
Carotid sheath contents
Signup and view all the flashcards
Anterior Relations of Isthmus
Anterior Relations of Isthmus
Signup and view all the flashcards
Anterior relations of the Isthmus
Anterior relations of the Isthmus
Signup and view all the flashcards
Poles Relation
Poles Relation
Signup and view all the flashcards
Superior thyroid vein origin
Superior thyroid vein origin
Signup and view all the flashcards
Inferior thyroid vein origin
Inferior thyroid vein origin
Signup and view all the flashcards
Goiter
Goiter
Signup and view all the flashcards
goiter character
goiter character
Signup and view all the flashcards
Thyroid surgery complications
Thyroid surgery complications
Signup and view all the flashcards
Non-recurrent laryngeal nerve
Non-recurrent laryngeal nerve
Signup and view all the flashcards
TSAb
TSAb
Signup and view all the flashcards
Thyroid follicles
Thyroid follicles
Signup and view all the flashcards
Thyroid hormone:
Thyroid hormone:
Signup and view all the flashcards
Study Notes
- Study notes, focusing on the surgical anatomy of the thyroid.
Embryology
- The thyroid gland begins functioning in the 4th month of intrauterine life.
- The thyroid gland is derived from the thyroglossal duct and the ultimobranchial body.
Thyroglossal Duct
- Originates from the endoderm of the floor of the embryonic pharynx at the foramen cecum.
- Foramen cecum is a midline foramen at the junction of the anterior 2/3 and posterior 1/3 of the developing tongue.
- Starts at the foramen caecum via the substance of the tongue.
- Passes downward in the midline anterior to the hyoid bone.
- The duct usually recurs posterior to the hyoid bone.
- Proceeds down in front of thyroid and cricoid cartilages.
Fate of the Thyroglossal Duct
- Cranial end is indicated by the foramen cecum of the tongue.
- May persist as a pyramidal lobe, extending from the isthmus.
- May persist as the occasional levator glandulae thyroideae, a fibromuscular slip attaching the pyramidal lobe to the hyoid bone.
- The remainder of the duct obliterates.
- Derivatives include the follicular cells of the thyroid gland, originating from the bilobed lower end.
Ultimobranchial Body
- Referred to as the "Caudal pharyngeal complex."
- Derivatives include parafollicular cells, joining each side of the lower end of the thyroglossal duct.
Congenital Anomalies
- Ectopic thyroid results from the thyroglossal duct failing to descend.
- Ectopic thyroid presents along the course of the thyroglossal duct as:
- Lingual thyroid: The gland remains in the oral cavity on the dorsum of the tongue.
- Intralingual.
- Suprahyoid.
- Retrohyoid.
- Infrahyoid.
- Thyroglossal cyst results from persistence of the thyroglossal duct, presenting as midline swelling in the neck.
- The cyst is in the vicinity of the hyoid bone; surgical removal includes the body of the hyoid bone to prevent recurrence.
- When the cyst breaks through the skin, it results in a thyroglossal fistula, which is never congenial.
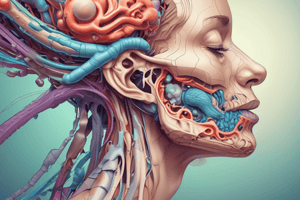
Surgical Anatomy: General Characteristics
- The thyroid gland is a highly vascular endocrine gland.
- Located in the lower part of the front of the neck, close to the larynx and trachea.
- Average weight is approximately 25 grams in adults, slightly heavier in females.
Parts of the Thyroid Gland
- Two lateral lobes (right and left), each measuring about 5 cm in length, 3 cm in breadth, and 2 cm in thickness.
- Isthmus connects the two lateral lobes over the trachea.
- A small pyramidal lobe may also be present.
Each Lobe
- Apex lies opposite the oblique line of the thyroid cartilage.
- Base is at the level of the 5th or 6th tracheal ring, corresponding to the C5-T1 vertebral level.
- Isthmus is against the level from the 2nd to 3rd or 4th tracheal rings.
- Pyramidal lobe extends from the upper margin of the isthmus on the left side.
- It may be attached to the hyoid bone by a slip of muscle called levator glandulae thyroideae.
Capsule of Thyroid
- It has a true (fibrous) and a false (fascial) capsule.
Clinical Correlation: Enlarged Thyroid Gland
- Upward shift is arrested by the attachment of the sternothyroid muscle to the oblique line of the thyroid cartilage.
- Downward shift occurs due to short neck and strong strap muscles pushing the lower pole downward into the superior mediastinum (retrosternal goiter).
Thyroid Capsule: True Capsule (Fibrous)
- Consists of connective tissue condensation at the periphery of the gland.
- Completely surrounds the gland.
- Venous plexus lies deep to it.
- During surgical removal, care is taken to remove the gland along with its true capsule to avoid injury to the venous plexus.
False Capsule (Fascial)
- Derived from the pretracheal layer of deep cervical fascia.
Attachment and Importance of Pretracheal Fascia
- Superiorly, attaches to the oblique line of the thyroid cartilage.
- Laterally, continuous with the deep cervical fascia.
- Inferiorly, continuous with the fibrous pericardium.
- Responsible for movement of the thyroid gland up with deglutition.
Pretracheal Fascia Considerations
- Movements of the thyroid during swallowing and speech are due to attachments to thyroid and cricoid cartilages, plus the hyoid bone.
- Related to retrosternal extension and compression manifestation of huge goiters.
Suspensory Ligament of Berry
- Thickening of the pretracheal fascia.
- Located at the posteromedial aspect of the thyroid gland lobe and cricoid cartilage.
- Holds the gland firmly in contact with the larynx.
- The ligament must be identified and cut, because the recurrent laryngeal nerve (RLN) lies behind it and is liable to injury during operation.
Relations of Lobes of the Thyroid Gland
- Surfaces: Superficial (anterolateral), medial, posterior (posterolateral).
- Borders: Anterior and posterior.
- Poles: Superior and inferior.
Relations of Surfaces
Superficial Surface
- Infrahyoid muscles (sternothyroid, sternohyoid, and omohyoid "superior belly").
- Laterally covered by the anterior margin of the sternomastoid.
Medial Surface
- Two tubes: Larynx and pharynx above and trachea and esophagus below.
- Two muscles: Inferior constrictor and cricothyroid.
- Two cartilages: Cricoid and thyroid.
- Two nerves: External and recurrent laryngeal.
- The recurrent laryngeal nerve passes upwards in the groove between the trachea & esophagus.
- It lies immediately behind the cricothyroid joint and the ligament of Berry.
Posterior Relations
- Carotid sheath (vagus nerve, carotid artery, internal jugular vein).
- Sympathetic chain "behind the carotid sheath."
- Prevertebral fascia and longus colli, "directly behind."
- On the left side, the lower pole may be closely related to the arch of the thoracic duct.
Relations of Borders
Anterior Border
- Related to the anterior branch of the superior thyroid artery.
Posterior Border
- Related to the parathyroid glands.
- Related to the anastomosis between the superior and inferior thyroid arteries.
Anteriorly
- Pretracheal fascia, strap muscles, investing layer of deep fascia, superficial fascia with anterior jugular veins, and the skin.
Relations of Isthmus
- Posteriorly it rests on the 2nd to 3rd or 4th tracheal rings.
- Upper margin is the terminal parts of anterior branches of the superior thyroid arteries.
- Inferior thyroid veins emerge, and the thyroidea ima (when present) enters.
Relations of Poles: Superior Pole "Apex"
- Limited by the insertion of the thyrohyoid muscle to the oblique line of the thyroid cartilage.
- Related to the superior thyroid artery and external laryngeal nerve.
Inferior Pole "Base"
- Related to the inferior thyroid artery and recurrent laryngeal nerve.
- On the left side, it may be related to the arch of the thoracic duct.
Surface Anatomy for Locating the Thyroid Gland
The Lobes (Left & Right)
- Located in the anterior triangles in the lower neck, on either side of the airway & digestive tract.
- Inferior to the position of the oblique line of the thyroid cartilage.
- Sternothyroid attaches superiorly to the oblique lines and lies anterior to the lobes of the thyroid gland, preventing the lobes from moving upward.
- Palpation can be done by finding the thyroid prominence & arch of the cricoid cartilage, and then feeling posterolateral to the larynx.
The Isthmus
- Crosses anterior to the upper end of the trachea.
- Easily palpated in the midline inferior to the arch of the cricoid.
- Makes palpating the tracheal cartilages difficult, and makes it difficult to artificially enter the airway anteriorly through the trachea, affecting tracheostomy
Arterial Supply to the Thyroid Gland
- Supplied by paired superior thyroid arteries, paired inferior thyroid arteries, the thyroidea ima, and accessory thyroid arteries.
Superior Thyroid Arteries
- Arise from the external carotid artery.
- Descend to the superior pole of the lateral lobe of the gland.
- The external laryngeal nerve accompanies the superior thyroid arteries.
- The artery enters the gland at the upper pole.
- The upper pole is the safest site for tying the superior thyroid artery during thyroidectomy.
Inferior Thyroid Arteries
- Arise from the thyrocervical trunk of the first part of the subclavian artery.
- Forms a loop with upward convexity to reach the level of the sixth cervical vertebra.
- Descends to reach the base of the lateral lobe of the gland.
- Enters the lower pole of the gland, where it is very close to the recurrent laryngeal nerve.
- Is safer to tie the inferior thyroid artery away from the lower pole of the gland as possible during thyroidectomy.
- The ascending branch of the inferior thyroid artery anastomoses with the descending branch of the superior thyroid artery along the posterior margin of the gland.
Additional Arteries
- The thyroidea ima arises from the arch of the aorta or brachiocephalic trunk and ascends in front of the trachea, entering the isthmus.
- Accessory thyroid arteries arise from esophageal & tracheal branches of inferior thyroid arteries.
Note
- Thyroid arteries are large-sized and show arterial loops to accommodate the upward & downward movements of the thyroid gland.
Venous Drainage of Thyroid
- The thyroid veins do not accompany the thyroid arteries.
- Three pairs of veins: superior, middle, and inferior.
- Superior thyroid vein: emerges from the upper pole on each side and drains into the corresponding internal jugular vein.
- Middle thyroid vein: emerges from the lobe and drains into the corresponding internal jugular vein.
- Inferior thyroid vein: emerges from the lower margin of the isthmus and descends on the anterior surface of the trachea, and both left and right veins drain into the left brachio-cephalic vein however sometimes each vein may drain into respective brachio-cephalic vein.
- Occasionally, Kocher's vein is present between the inferior & middle thyroid veins which opens into the internal jugular vein.
Lymphatics of the Thyroid
- Upper part of the thyroid drains into upper deep cervical nodes (jugulo-digastric) directly or indirectly through the prelaryngeal nodes.
- Lower part drains into lower deep cervical group (jugulo-omohyoid) directly or indirectly through the pretracheal (delphic) & paratracheal nodes.
- Lymph vessels may drain into brachiocephalic nodes in the superior mediastinum.
- Some vessels directly reach the thoracic duct.
- Lymphatic spread of papillary carcinoma of the thyroid gland manifests with normal thyroid looks, but deep cervical lymph nodes of the jugular chain are enlarged and contain thyroid tissue.
Nuclear Scan of Thyroid Gland
- Is a procedure to study the function of the thyroid gland by isotope scanning.
- Performed by giving radioactive iodine (131I) orally and by taking photographs of the thyroid gland.
- Hot spots on the scan indicate hyperactive areas of the gland.
- Cold spots indicate hypoactive areas.
- Thyroid scans are useful in locating ectopic thyroid tissue outside the neck (lingual or retrosternal).
Thyroid Stimulating Antibodies (TsAB)
- A family of IgG immunoglobulins, collectively known as Thyroid Stimulating Antibodies (TsAB).
- Mechanism of action includes activation of TSH receptors on the follicular cell membrane.
- Have a more protracted action than TSH (TsAB: 16 - 24 hours vs TSH: 1.5 - 3 hours).
- Responsible for most cases of thyrotoxicosis that are not due to autonomous toxic nodules.
- Serum concentrations are very low & not routinely measured.
Histological Structure of the Thyroid Gland: Thyroid Follicles
- Are the structural & functional unit,Number around 30 million, Size 0.05-0.5 mm & shape is rounded or oval.
- Lumen contains filled with colloid (Thyroglobulin).
- Wall lined by low cubical epithelial cells lying on a thin basement membrane.
- The lining cells are Follicular cells and Parafollicular cells.
- Follicular cells represent 98% of the cells which synthesis and secretion of thyroid hormones.
- Parafollicular cells represent 2% of cells and secrete calcitonin hormone which lowers serum calcium levels .
Thyroid Hormones Synthesis in the thyroid Gland
- Production of tri-iodothyronine (T3) & thyroxine (T4).
- Step 1: Trapping inorganic lodide from the blood.
- Step 2: Oxidation: via Thyroid Peroxidase enzyme (TPO), Iodide → lodine.
- Step 3: Iodination by binding of iodine to Tyrosine to form Mono-iodotyrosine (MIT) & Di-iodotyrosine (DIT).
- Step 4: Coupling where Di + Di → T4 (Tetra iodothyronine) & Mono + Di → T3 (Tri iodothyronine). Coupling occurs within the thyroglobulin molecule
- Under the control of TSH “When hormones are required”, The complex is resorbed into the cell & Thyroglobulin is broken down into T 3 & T 4 & hormones are released into blood circulation
- Thyroid hormones circulate in 2 forms where Free part is in equilibrium with the protein bound hormone mainly Thyroxin Binding Globulin (TBG) , where Bounded form represents more than 99% & Biologically active part represent lower than 1%.
- Peripheral Tissue conversions occurs by by converting of T4 to T3 in the peripheral tissue ,Where T3 Is more important, more active & quick acting (within a few hours) whereas T4 acts more slowly (4-14 days) but produces greater effect due to abundance,
Pathology: Goiter
- Definition is abnormal enlargement of the thyroid gland (“The common cause of a midline swelling in the neck").
- Thyroid swelling moves with deglutition & May present as a smooth swelling or a nodular swelling.
- Classifications include Physiological that occurs during pregnancy, Endemic usually large swelling due to to deficiency of iodine in the diet or drinking water which will leads to hypothyroidis, Toxic is of diffuse or nodular variety due to Hyperthyroidism or thyrotoxicosis showing eye symptoms such as cardiovascular system symptoms and nervous system symptoms,or Neoplastic presenting as enlargement of the gland spreading by spread by lymph vessels while either by blood which has long distance like lungs, ends of long bones, skull and vertebrae.
Complications, Management and Complications of thyroid surgery
- Complications such as Compression Effects due to The enlarged thyroid gland tends to compress the structures around such as causing Dyspnea due compression on the trachea, also Dysphagia due Esophagus compression or Hoarseness of voice due to compression om the Recurrent laryngeal nerve
- Management can be done by thyroid lobectomy, Near-total thyroidectomy or simple Total thyroidectomy where total glands gets removed
Management: Types of Thyroidectomy Surgery.
- Thyroid lobectomy: Removal of a lobe + the isthmus.
- Near-total thyroidectomy: Removal of most of the normal lobe (with conservation of small thyroid tissue "between the esophagus & trachea" on the normal side).
- Total thyroidectomy: Removal of the entire gland.
Complications of Thyroidectomy surgery.
- Can lead to accidental Injury to the recurrent laryngeal nerve during tying the inferior thyroid artery or its branches whichis often referred to as “The most feared complication” and Non-recurrent laryngeal nerve,
- Or Can lead to Parathyroid insufficiency (tetany) due to removal of parathyroid glands along with thyroid gland or Injury to the artery supplying the parathyroid glands causing atrophy of these glands.
Non-recurrent laryngeal nerve
- Is a congenital anomaly where the right recurrent laryngeal nerve may be non recurrent arising from the right vagus higher up in the neck, Incidence is 1% of all cases and can be caused by right subclavian artery has a aberrant form
- The reason for this anomaly: The right subclavian artery is aberrant where surgeon should keep it in the back of hismind while locating the nerve due potential damage during procedure.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.