Podcast
Questions and Answers
Why should free T4 levels be assessed before a morning dose of levothyroxine?
Why should free T4 levels be assessed before a morning dose of levothyroxine?
To avoid skewed results that may result from recent levothyroxine intake.
What makes Total T4 levels unreliable for assessing thyroid function?
What makes Total T4 levels unreliable for assessing thyroid function?
Total T4 is affected by transport protein levels, which can vary in different conditions.
Why is Total T3, not the best test for primary hypothyroidism?
Why is Total T3, not the best test for primary hypothyroidism?
In primary hypothyroidism, increased conversion of T4 to T3 by MDI can preserve T3 levels, making it an insensitive measure.
What is a major limitation of free T3 assays?
What is a major limitation of free T3 assays?
What is the most common congenital endocrine disorder in childhood?
What is the most common congenital endocrine disorder in childhood?
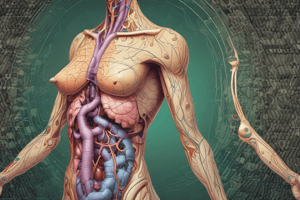
What is the primary role of thyroid hormones in the human body?
What is the primary role of thyroid hormones in the human body?
Describe the physical location of the thyroid gland in the neck.
Describe the physical location of the thyroid gland in the neck.
What are the two transcription factors that help regulate thyroid gland development?
What are the two transcription factors that help regulate thyroid gland development?
Which cells within the thyroid gland synthesize thyroid hormones, and what is their role regarding iodine?
Which cells within the thyroid gland synthesize thyroid hormones, and what is their role regarding iodine?
What is pendrin's role in the synthesis of thyroid hormones?
What is pendrin's role in the synthesis of thyroid hormones?
What is the enzyme responsible for organifying iodine?
What is the enzyme responsible for organifying iodine?
How are T3 and T4 formed in relation to MIT and DIT?
How are T3 and T4 formed in relation to MIT and DIT?
What are the percentages of circulating T4 and T3 directly produced by the thyroid gland?
What are the percentages of circulating T4 and T3 directly produced by the thyroid gland?
What are the three main features of thyroid dysgenesis?
What are the three main features of thyroid dysgenesis?
What is the key identifying feature of a TSH receptor defect, differentiating it from dysgenesis?
What is the key identifying feature of a TSH receptor defect, differentiating it from dysgenesis?
Dyshormonogenesis is typically associated with what two clinical features?
Dyshormonogenesis is typically associated with what two clinical features?
Name two common causes for transient hypothyroidism in newborns.
Name two common causes for transient hypothyroidism in newborns.
What maternal factor can cause transient hypothyroidism in a newborn?
What maternal factor can cause transient hypothyroidism in a newborn?
In central hypothyroidism, are TSH levels high or low?
In central hypothyroidism, are TSH levels high or low?
How can you differentiate between a secondary and tertiary cause of central hypothyroidism?
How can you differentiate between a secondary and tertiary cause of central hypothyroidism?
Name one genetic mutation that can cause central hypothyroidism.
Name one genetic mutation that can cause central hypothyroidism.
What is the most common cause of primary congenital hypothyroidism?
What is the most common cause of primary congenital hypothyroidism?
What are the two subtypes of thyroid dysgenesis?
What are the two subtypes of thyroid dysgenesis?
Besides a defective thyroid, what other cause can lead to primary congenital hypothyroidism?
Besides a defective thyroid, what other cause can lead to primary congenital hypothyroidism?
How is secondary congenital hypothyroidism primarily diagnosed?
How is secondary congenital hypothyroidism primarily diagnosed?
What lab findings are indicative of primary hypothyroidism?
What lab findings are indicative of primary hypothyroidism?
Why do patients with ectopic thyroid typically have reduced thyroglobulin levels?
Why do patients with ectopic thyroid typically have reduced thyroglobulin levels?
What imaging modality is most useful in identifying an ectopic thyroid?
What imaging modality is most useful in identifying an ectopic thyroid?
What maternal factor can lead to transient congenital hypothyroidism?
What maternal factor can lead to transient congenital hypothyroidism?
List three symptoms of congenital hypothyroidism in newborns.
List three symptoms of congenital hypothyroidism in newborns.
What are three criteria, according to the text, for a disorder to qualify for neonatal screening?
What are three criteria, according to the text, for a disorder to qualify for neonatal screening?
Why are thyroid functions assessed after 72 hours of life in newborns?
Why are thyroid functions assessed after 72 hours of life in newborns?
What is the preferred initial test for congenital hypothyroidism, according to the text?
What is the preferred initial test for congenital hypothyroidism, according to the text?
Beyond 14 days, what permanent impact is associated with congenital hypothyroidism if left untreated?
Beyond 14 days, what permanent impact is associated with congenital hypothyroidism if left untreated?
What condition is indicated when a patient has elevated T3, T4, and TSH levels, despite the presence of peripheral hypothyroidism?
What condition is indicated when a patient has elevated T3, T4, and TSH levels, despite the presence of peripheral hypothyroidism?
What enzyme, if unusually active, can cause thyroxine-unresponsive hypothyroidism?
What enzyme, if unusually active, can cause thyroxine-unresponsive hypothyroidism?
An MCT8 defect presents with severe fetal-onset hypothyroidism, high T3, and low T4, what is this condition also known as?
An MCT8 defect presents with severe fetal-onset hypothyroidism, high T3, and low T4, what is this condition also known as?
What range of TSH levels is characteristic of isolated thyrotropinemia, given normal FT4 levels?
What range of TSH levels is characteristic of isolated thyrotropinemia, given normal FT4 levels?
In individuals with Trisomy 21, what is the typical finding in terms of T4 levels and TSH levels?
In individuals with Trisomy 21, what is the typical finding in terms of T4 levels and TSH levels?
What is the typical TSH level presented in transient hypothyroxinemia of prematurity?
What is the typical TSH level presented in transient hypothyroxinemia of prematurity?
What clinical picture can dopamine use result in, in relation to thyroid hormones?
What clinical picture can dopamine use result in, in relation to thyroid hormones?
Infants with congenital hypothyroidism are usually born at what stage of gestation?
Infants with congenital hypothyroidism are usually born at what stage of gestation?
Flashcards
What is the function of thyroid hormones?
What is the function of thyroid hormones?
Thyroid hormones play a crucial role in regulating growth, development, metabolism, and body temperature.
Where is the thyroid gland located?
Where is the thyroid gland located?
The thyroid gland is located in the front of the neck, below the Adam's apple.
What are the parts of the thyroid gland?
What are the parts of the thyroid gland?
The thyroid gland is composed of two lobes connected by a bridge called the isthmus.
How does the thyroid gland develop?
How does the thyroid gland develop?
Signup and view all the flashcards
What proteins regulate thyroid gland development?
What proteins regulate thyroid gland development?
Signup and view all the flashcards
What are follicular cells and their function?
What are follicular cells and their function?
Signup and view all the flashcards
What transports iodine into the thyroid follicular cells?
What transports iodine into the thyroid follicular cells?
Signup and view all the flashcards
Which enzymes are involved in iodine organification?
Which enzymes are involved in iodine organification?
Signup and view all the flashcards
Congenital Hypothyroidism (CH)
Congenital Hypothyroidism (CH)
Signup and view all the flashcards
Thyroid Hormone
Thyroid Hormone
Signup and view all the flashcards
Free T4
Free T4
Signup and view all the flashcards
Thyrotoxicosis
Thyrotoxicosis
Signup and view all the flashcards
Thyroid Scan
Thyroid Scan
Signup and view all the flashcards
Thyroid Dyshormonogenesis
Thyroid Dyshormonogenesis
Signup and view all the flashcards
Thyroid Dysgenesis
Thyroid Dysgenesis
Signup and view all the flashcards
Ectopic Thyroid
Ectopic Thyroid
Signup and view all the flashcards
TSH Test
TSH Test
Signup and view all the flashcards
Primary Hypothyroidism
Primary Hypothyroidism
Signup and view all the flashcards
Secondary Hypothyroidism
Secondary Hypothyroidism
Signup and view all the flashcards
Transient Hypothyroidism
Transient Hypothyroidism
Signup and view all the flashcards
Thyroglobulin
Thyroglobulin
Signup and view all the flashcards
Agenesis
Agenesis
Signup and view all the flashcards
TSH Receptor Defect
TSH Receptor Defect
Signup and view all the flashcards
Dyshormonogenesis
Dyshormonogenesis
Signup and view all the flashcards
Sodium-Iodine Symporter (NIS) Defect
Sodium-Iodine Symporter (NIS) Defect
Signup and view all the flashcards
TPO Deficiency
TPO Deficiency
Signup and view all the flashcards
Tertiary Hypothyroidism
Tertiary Hypothyroidism
Signup and view all the flashcards
What are common symptoms of congenital hypothyroidism in newborns?
What are common symptoms of congenital hypothyroidism in newborns?
Signup and view all the flashcards
What screening test is used to diagnose congenital hypothyroidism in newborns?
What screening test is used to diagnose congenital hypothyroidism in newborns?
Signup and view all the flashcards
What can happen if congenital hypothyroidism is not detected and treated early?
What can happen if congenital hypothyroidism is not detected and treated early?
Signup and view all the flashcards
Why is neonatal screening for congenital hypothyroidism important?
Why is neonatal screening for congenital hypothyroidism important?
Signup and view all the flashcards
What is the preferred test to assess thyroid function, and why is it not always used for newborns?
What is the preferred test to assess thyroid function, and why is it not always used for newborns?
Signup and view all the flashcards
Multiple Pituitary Hormone Deficiency
Multiple Pituitary Hormone Deficiency
Signup and view all the flashcards
Thyroxine Unresponsive Hypothyroidism
Thyroxine Unresponsive Hypothyroidism
Signup and view all the flashcards
MCT8 Defect
MCT8 Defect
Signup and view all the flashcards
Isolated Thyrotropinemia
Isolated Thyrotropinemia
Signup and view all the flashcards
Trisomy 21 and Thyroid Function
Trisomy 21 and Thyroid Function
Signup and view all the flashcards
Transient Hypothyroxinemia of Prematurity
Transient Hypothyroxinemia of Prematurity
Signup and view all the flashcards
Non-Thyroidal Illness and Thyroid Function
Non-Thyroidal Illness and Thyroid Function
Signup and view all the flashcards
Congenital Hypothyroidism and Birth
Congenital Hypothyroidism and Birth
Signup and view all the flashcards
Study Notes
Thyroid Disorders in Children
- Thyroid disorders are a significant concern in children, affecting growth, development, and metabolism.
- The thyroid gland is located in the middle of the neck, beneath the thyroid cartilage.
- The gland comprises two lobes, an isthmus, and sometimes a pyramidal lobe. These lobes originate from different embryonic sources.
- Thyroid hormones (T3 and T4) are crucial for regulating growth, development, metabolism, and body temperature. They are synthesized within the follicular cells of the thyroid gland.
- Iodine uptake is the first step in thyroid hormone synthesis. Iodine is transported into the follicular cell by a sodium-iodide transporter.
- Inorganic iodine is then transported to the basolateral surface by the protein pendrin, and organified by the enzymes thyroid peroxidase (TPO) and Dual oxidase 2 (Duox2).
- Organified iodine is incorporated into thyroglobulin, combining with tyrosine to form monoiodotyrosine (MIT) and diiodotyrosine (DIT).
- Two DIT molecules fuse to create thyroxine (T4), while one DIT and one MIT combine to form triiodothyronine (T3).
- Ninety percent of circulating T4 and 20-30% of T3 is directly produced by the thyroid gland. Remaining T3 is generated from peripheral conversion of T4 by the enzyme monodeiodinase I (MDI).
- Free T4 and T3 circulate bound to proteins (TBG, albumin, transthyretin).
- T4 is primarily bound to TBG, while T3 binds to all three.
- Thyroid hormone metabolism involves the conversion of T4 to T3, and their inactivation to reverse T3 (rT3) and T2 by type 3 MDI in target tissues.
- T3 is the active thyroid hormone, entering cells and binding to intracellular receptors to regulate gene expression.
- Thyroid hormone production and release in the body is controlled by TSH, secreted by pituitary thyrotropes acting on TSH receptors. This regulates iodine uptake, organification, coupling, and hormone release. Also regulates follicular development.
- TSH secretion controlled by the hypothalamic hormone, TRH (thyrotropin-releasing hormone).
- Thyroid function assessment in a child includes clinical evaluation and assessment of thyroid function and structure. A full history and examination are important.
- Common symptoms of hypothyroidism in children include weakness, lethargy, weight gain, somnolence, facial puffiness, decreased performance, and decreased activity/ hypotonia.
- Symptoms of hyperthyroidism in children include weight loss, anxiety, tremors, eye protrusion, neck swelling, and the presence of type 1 diabetes mellitus or celiac disease.
- Thyroid examination typically assesses size, mobility, and consistency. The presence of a goiter may indicate further testing.
- Thyroid function tests—TSH, T4, and potentially T3—are used to evaluate thyroid dysfunction. Free T4 is a more consistent indicator than total T4.
- Congenital hypothyroidism (CH) is the most common congenital endocrine disorder in childhood and is largely preventable. It is defined as thyroid hormone deficiency present at birth, with approximately 1 case per 1500 live births.
- Causes of CH include thyroid dysgenesis, dyshormonogenesis, TSH resistance, transient hypothyroidism, and peripheral hypothyroidism.
- Secondary (central) hypothyroidism arises from pituitary or hypothalamic abnormalities, characterized by low/inappropriately normal TSH with low free T4. Causes include CNS insult, tumor, radiation, or trauma.
- Primary hypothyroidism is diagnosed by the presence of elevated TSH levels with low or normal T4 levels. Common causes include ectopic thyroid, genetic defects, or dyshormonogenesis.
- Treatment for hypothyroidism typically involves levothyroxine replacement therapy, with careful monitoring of free T4 and TSH levels. Dose adjustment is often necessary.
Acquired Hypothyroidism
- Subclinical hypothyroidism is frequently experienced by adolescents.
- Causes of acquired hypothyroidism include chronic lymphocytic (Hashimoto's) thyroiditis, iodine deficiency, medications and post-radiation or ablative (radioiodine therapy or surgery).
- Symptoms, physical examination, and investigations aid in diagnosis.
Thyrotoxicosis in Children
- Thyrotoxicosis, while rare in children is important to identify. It generally is characterized by an increased production of thyroid hormones, leading to clinical manifestations like weight loss, hyperdefection (often associated with increased urination-polyuria) , tremors, anxiety, irritability, and worsening school performance.
- Causes of thyrotoxicosis include TSH receptor activating mutations, toxic thyroid nodules, toxic multinodular goiter, subacute lymphocytic (granulomatous) thyroiditis, and acute thyroiditis.
- Graves' disease is a common cause of thyrotoxicosis, predominantly in females affecting most children who present with symptoms.
- Diagnosing thyrotoxicosis involves identifying the cause, evaluating complications, and considering a comprehensive clinical and laboratory evaluation, including thyroid function tests (TFTs), erythrocyte sedimentation rate (ESR), and potentially antibodies (e.g., TSH receptor antibodies).
- Management strategies for thyrotoxicosis may include antithyroid drugs, radioactive iodine, or surgery, adjusting the strategy based on child characteristics.
- Monitoring is critical; after treatment the thyroid profile needs to monitored for 6 weeks and then monthly to ensure proper response to the treatment and prevent complications.
Congenital Hypothyroidism (CH) Assessment
- Evaluation of newborns for hypothyroidism (neonatal screening) is essential.
- Screening for CH typically involves measuring TSH levels—high TSH levels suggest a need for further evaluation.
- Typical presentation involves certain signs and symptoms and physical characteristics if diagnosed at an early age or later ages.
- Confirmation of the diagnosis involves assessing underlying factors. If no improvement or the disorder is prolonged, confirmatory medical procedures may be required.
Monitoring of Thyroid Function
- Monitoring of thyroid hormone levels (free T4 and TSH) is vital throughout treatment to maintain appropriate levels.
- Adjustments to medication doses are typically needed to maintain the proper target levels of free thyroxine. This requires accurate tracking and frequent dosage adjustments.
- Persistent monitoring of thyroid function tests is essential after treatment, with appropriate dosage adjustments.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.