Podcast
Questions and Answers
What is the term used to describe advanced hypothyroidism?
What is the term used to describe advanced hypothyroidism?
- Myxoedema (correct)
- Hashimoto disease
- Thyroid hormone resistance
- Graves disease
What is the main cause of primary hyperthyroidism in adults?
What is the main cause of primary hyperthyroidism in adults?
- Iodine deficiency
- Graves disease (correct)
- Hashimoto disease
- Thyroid hormone resistance
What is the result of secondary hypothyroidism?
What is the result of secondary hypothyroidism?
- Increased thyroid hormone release
- Increased TSH secretion
- Decreased thyroid hormone release
- Decreased TSH secretion (correct)
What is the term used to describe the condition where patients present with signs and symptoms of hypothyroidism without a decrease in circulating thyroid hormone levels?
What is the term used to describe the condition where patients present with signs and symptoms of hypothyroidism without a decrease in circulating thyroid hormone levels?
What is the primary function of the adrenal cortex?
What is the primary function of the adrenal cortex?
What is the cause of secondary hyperthyroidism?
What is the cause of secondary hyperthyroidism?
What is the result of Hashimoto disease?
What is the result of Hashimoto disease?
What is the result of Graves disease?
What is the result of Graves disease?
At physiologic levels, T4 is relatively inactive because:
At physiologic levels, T4 is relatively inactive because:
What percentage of plasma T4 and T3 is bound to thyroxine-binding globulin (TBG)?
What percentage of plasma T4 and T3 is bound to thyroxine-binding globulin (TBG)?
Which of the following hormones stimulates the production of TSH?
Which of the following hormones stimulates the production of TSH?
What is the half-life of T3?
What is the half-life of T3?
What is the result of deficient thyroid hormone secretion?
What is the result of deficient thyroid hormone secretion?
What percentage of each hormone circulates in its free form?
What percentage of each hormone circulates in its free form?
What is the main function of thyroxine-binding globulin (TBG)?
What is the main function of thyroxine-binding globulin (TBG)?
Which of the following thyroid hormones binds more tightly to binding proteins?
Which of the following thyroid hormones binds more tightly to binding proteins?
What is the primary catecholamine secreted by the medulla?
What is the primary catecholamine secreted by the medulla?
What is the effect of cortisol on protein metabolism in muscle?
What is the effect of cortisol on protein metabolism in muscle?
What percentage of glucocorticoids are protein-bound in plasma?
What percentage of glucocorticoids are protein-bound in plasma?
What is the effect of oestrogen treatment on plasma CBG levels?
What is the effect of oestrogen treatment on plasma CBG levels?
What is the main stimulus to cortisol secretion?
What is the main stimulus to cortisol secretion?
What is the effect of increased plasma cortisol levels on CRH secretion?
What is the effect of increased plasma cortisol levels on CRH secretion?
What is the characteristic of cortisol levels in the diurnal rhythm?
What is the characteristic of cortisol levels in the diurnal rhythm?
What is the effect of stress on CRH secretion?
What is the effect of stress on CRH secretion?
Where is TRH synthesized?
Where is TRH synthesized?
What is the role of thyroglobulin in thyroid hormone synthesis?
What is the role of thyroglobulin in thyroid hormone synthesis?
What is the result of TSH receptor activation on thyroid follicular epithelial cells?
What is the result of TSH receptor activation on thyroid follicular epithelial cells?
What is the primary source of circulating T3?
What is the primary source of circulating T3?
What is the role of thyroid peroxidase in thyroid hormone synthesis?
What is the role of thyroid peroxidase in thyroid hormone synthesis?
What is the ratio of T4 to T3 in the plasma?
What is the ratio of T4 to T3 in the plasma?
Where does the majority of peripheral deiodination of T4 to form T3 occur?
Where does the majority of peripheral deiodination of T4 to form T3 occur?
What is the term for the process of iodine binding to carbon 3 or 5 of the tyrosine residues on thyroglobulin?
What is the term for the process of iodine binding to carbon 3 or 5 of the tyrosine residues on thyroglobulin?
What is the primary function of aldosterone in the body?
What is the primary function of aldosterone in the body?
What stimulates aldosterone production in the adrenal glands?
What stimulates aldosterone production in the adrenal glands?
What is the name of the syndrome caused by overproduction of cortisol?
What is the name of the syndrome caused by overproduction of cortisol?
What percentage of Cushing's syndrome cases are caused by pituitary adenoma?
What percentage of Cushing's syndrome cases are caused by pituitary adenoma?
What is the name of the syndrome caused by overproduction of aldosterone?
What is the name of the syndrome caused by overproduction of aldosterone?
What is the name of the enzyme produced by the kidney in response to decreased blood volume?
What is the name of the enzyme produced by the kidney in response to decreased blood volume?
What is the primary site of angiotensin-converting enzyme (ACE) activity?
What is the primary site of angiotensin-converting enzyme (ACE) activity?
What is the effect of increased plasma potassium levels on aldosterone production?
What is the effect of increased plasma potassium levels on aldosterone production?
Flashcards are hidden until you start studying
Study Notes
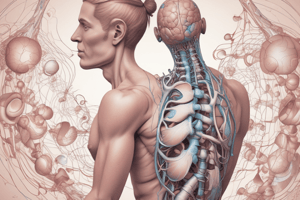
Thyroid Hormone Synthesis
- Thyroglobulin (Tg) plays a crucial role in the synthesis and storage of thyroid hormone.
- Tg is a glycoprotein containing multiple tyrosine residues, which serves as a scaffold for thyroid hormone synthesis.
- Iodine binds to carbon 3 or 5 of the tyrosine residues on Tg, resulting in the formation of monoiodinated tyrosine (MIT) and diiodinated tyrosine (DIT) residues.
- The coupling of iodinated tyrosine residues, either of 2 DIT residues or of 1 MIT and 1 DIT residue, is catalyzed by the enzyme thyroid peroxidase (TPO) to form triiodothyronine (T3) or tetraiodothyronine (T4).
Thyroid Hormone Release and Regulation
- The thyroid gland releases more T4 than T3, resulting in 40-fold higher plasma concentrations of T4.
- Most of the circulating T3 is formed peripherally by deiodination of T4, a process that involves the removal of iodine from carbon 5 on the outer ring of T4.
- T4 acts as a prohormone for T3, and its deiodination occurs predominantly in the liver, kidney, and thyroid follicular epithelial cells.
- Thyroid hormone synthesis is regulated by the hypothalamic-pituitary-thyroid axis, with TSH being the main stimulator of thyroid hormone synthesis.
Thyroid Hormone Binding and Metabolism
- Most of the plasma T4 and T3 is protein bound, mainly to thyroxine-binding globulin (TBG) and, to a lesser extent, transthyretin and albumin.
- A small fraction of each hormone (0.03% of T4 and 0.3% of T3) circulates in its free form, which is the physiologically active form.
- T4 has a lower metabolic clearance rate and a longer half-life (7 days) than T3 (1 day) due to its tighter binding to binding proteins.
Disorders of the Thyroid Gland
- Hypothyroidism is characterized by insufficient thyroid hormone action, resulting in weight gain, myopathy, menstrual disturbances, and other symptoms.
- Two main types of hypothyroidism are distinguished: primary hypothyroidism (disease of the thyroid gland) and secondary hypothyroidism (decreased TSH secretion).
- Hyperthyroidism is characterized by excessive functional activity of the thyroid gland, resulting in weight loss, tachycardia, nervousness, anxiety, and difficulty sleeping.
- The most common cause of primary hyperthyroidism in adults is Graves' disease, an autoimmune thyroid disease.
Adrenal Gland Hormones
- The adrenal gland consists of two distinct tissues: the outer cortex and the inner medulla.
- The cortex secretes glucocorticoids, mineralocorticoids, and sex steroid hormones, while the medulla secretes catecholamines, principally adrenaline.
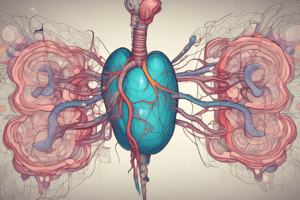
Glucocorticoid Secretion
- Glucocorticoids have widespread metabolic effects on carbohydrate, fat, and protein metabolism.
- In the liver, cortisol stimulates gluconeogenesis, amino acid uptake and degradation, and ketogenesis.
- In adipose tissue, cortisol increases lipolysis, and in muscle, it increases proteolysis and amino acid release.
Regulation of Glucocorticoid Secretion
- The main stimulus to cortisol secretion is ACTH, which is regulated by negative feedback control, stress, and the diurnal rhythm of plasma cortisol.
- The hypothalamic-pituitary-adrenal axis is the main regulatory system controlling cortisol secretion.
Aldosterone Secretion
- The principal physiological function of aldosterone is to conserve Na+, mainly by facilitating Na+ reabsorption and reciprocal K+ or H+ secretion in the distal renal tubule.
- The renin-angiotensin system is the most important system controlling aldosterone secretion.
- Aldosterone production is stimulated by the renin-angiotensin system, which is activated in response to changes in blood volume, renal perfusion pressure, and plasma K+ levels.
Adrenocortical Hyperfunction
- Hyperfunction of the adrenal cortex can lead to overproduction of cortisol (Cushing's syndrome) or aldosterone (Conn's syndrome).
- Cushing's syndrome can be ACTH-dependent or ACTH-independent, and is caused by tumors that release either ACTH or cortisol.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.