Podcast
Questions and Answers
During which period of development does the thyroid gland typically complete its bilobular structure?
During which period of development does the thyroid gland typically complete its bilobular structure?
- First trimester
- Postnatal period
- Third trimester (correct)
- Second trimester
Which anatomical structure connects the two main lobes of the thyroid gland?
Which anatomical structure connects the two main lobes of the thyroid gland?
- Trachea
- Isthmus (correct)
- Pyramidal lobe
- Larynx
What type of cells primarily compose the follicles within the thyroid gland?
What type of cells primarily compose the follicles within the thyroid gland?
- Nerve cells
- Connective tissue cells
- Adipocytes
- Epithelial cells (correct)
How does the epithelial cell height in thyroid follicles change with gland activity?
How does the epithelial cell height in thyroid follicles change with gland activity?
Which cells produce calcitonin?
Which cells produce calcitonin?
What is the primary mechanism by which dietary iodide is taken up into thyroid follicular cells?
What is the primary mechanism by which dietary iodide is taken up into thyroid follicular cells?
Which enzyme oxidizes iodide (I-) to iodine (I2) in the thyroid hormone synthesis process?
Which enzyme oxidizes iodide (I-) to iodine (I2) in the thyroid hormone synthesis process?
What precursors are coupled by thyroid peroxidase to form triiodothyronine (T3) and tetraiodothyronine (T4)?
What precursors are coupled by thyroid peroxidase to form triiodothyronine (T3) and tetraiodothyronine (T4)?
In what form are thyroid hormones primarily stored in the colloid of the thyroid follicles?
In what form are thyroid hormones primarily stored in the colloid of the thyroid follicles?
Which hormone causes endocytosis and proteolysis of the thyroglobulin-hormone complex?
Which hormone causes endocytosis and proteolysis of the thyroglobulin-hormone complex?
Which of the following thyroid hormones is more biologically active?
Which of the following thyroid hormones is more biologically active?
How are thyroid hormones mainly transported in the plasma?
How are thyroid hormones mainly transported in the plasma?
Where does the deiodination of T4 to T3 primarily occur?
Where does the deiodination of T4 to T3 primarily occur?
Which hormone inhibits the release of thyrotropin releasing hormone (TRH) from the hypothalamus as part of a negative feedback loop?
Which hormone inhibits the release of thyrotropin releasing hormone (TRH) from the hypothalamus as part of a negative feedback loop?
What effect does thyroid-stimulating hormone (TSH) have on iodide pumps in thyroid follicular cells?
What effect does thyroid-stimulating hormone (TSH) have on iodide pumps in thyroid follicular cells?
Within the cell, where do thyroid hormones exert their effects after binding to thyroid receptors (TR)?
Within the cell, where do thyroid hormones exert their effects after binding to thyroid receptors (TR)?
What is the effect of thyroid hormones on oxygen consumption in most tissues?
What is the effect of thyroid hormones on oxygen consumption in most tissues?
What is the primary effect of thyroid hormones on plasma cholesterol levels?
What is the primary effect of thyroid hormones on plasma cholesterol levels?
What is the effect of thyroid hormones on gluconeogenesis and glycogenolysis in the liver?
What is the effect of thyroid hormones on gluconeogenesis and glycogenolysis in the liver?
How do thyroid hormones affect skeletal growth and maturation?
How do thyroid hormones affect skeletal growth and maturation?
Which of the following processes is enhanced by thyroid hormones in adipocytes?
Which of the following processes is enhanced by thyroid hormones in adipocytes?
Which tissues or organs do not show increased oxygen consumption in response to thyroid hormones?
Which tissues or organs do not show increased oxygen consumption in response to thyroid hormones?
What is the status of protein synthesis and degradation when thyroid hormone levels are low?
What is the status of protein synthesis and degradation when thyroid hormone levels are low?
Which of the following describes thyroid gland development?
Which of the following describes thyroid gland development?
What is the primary reason for individuals with an underactive thyroid gland to feel cold?
What is the primary reason for individuals with an underactive thyroid gland to feel cold?
Flashcards
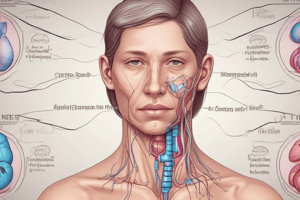
Thyroid Gland Development
Thyroid Gland Development
Appears early, develops ~4 weeks after conception as an epithelial invagination of the tongue, moves down the neck forming a bilobular structure by the 3rd trimester.
Thyroid Gland Anatomy
Thyroid Gland Anatomy
Two lobes (20-25g) on either side of the trachea, below the larynx, connected by the isthmus. Often 'butterfly-shaped' and has a pyramidal lobe.
Thyroid Histology
Thyroid Histology
The height epithelial cells varies depending on activity: inactive cells are flattened with large colloidal mass, active cells are columnar with small colloidal lumen.
Iodide and Hormone Synthesis
Iodide and Hormone Synthesis
Signup and view all the flashcards
T3 and T4 Formation
T3 and T4 Formation
Signup and view all the flashcards
Thyroglobulin (TG)
Thyroglobulin (TG)
Signup and view all the flashcards
Thyroid Hormone Transport
Thyroid Hormone Transport
Signup and view all the flashcards
Thyroid Hormone Metabolism
Thyroid Hormone Metabolism
Signup and view all the flashcards
TRH (Thyrotrophin Releasing Hormone)
TRH (Thyrotrophin Releasing Hormone)
Signup and view all the flashcards
TSH (Thyroid Stimulating Hormone)
TSH (Thyroid Stimulating Hormone)
Signup and view all the flashcards
Mechanism of T3 Action
Mechanism of T3 Action
Signup and view all the flashcards
Calorigenesis
Calorigenesis
Signup and view all the flashcards
Carbohydrate Metabolism
Carbohydrate Metabolism
Signup and view all the flashcards
Central Nervous System role
Central Nervous System role
Signup and view all the flashcards
Study Notes
- Thyroid hormones are the focus of the material
Thyroid Gland Development
- The thyroid gland appears very early in life
- Development begins ~4 weeks post-conception via tongue epithelial invagination
- It moves down the neck, forms a bilobular structure, and completes by the 3rd trimester
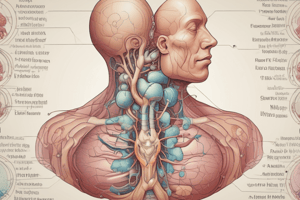
Anatomy of Thyroid Gland
- The thyroid gland comprises two 20-25g lobes on either side of the trachea, below the larynx, joined by the isthmus
- It has a 'Butterfly shape'
- A pyramidal lobe is often present
- The thyroid gland has a rich blood supply from thyroid arteries
- The autonomic nervous system innervates it
Cellular Structure of Thyroid Gland
- Distinct cellular organisation is related to its function
- It has cells arranged in follicles
- Over a million follicles exist here
- Follicles are spherical bodies of epithelial cells around the colloidal storage protein, thyroglobulin
Histology of Thyroid Gland
- Epithelial cell height differs based on gland activity
- Inactive epithelial cells are flattened with a large colloidal mass
- Active cells are columnar with a small colloidal lumen
- Epithelial cells are exocrine, absorptive and endocrine
- Larger epithelial cells lie between follicles as parafollicular C cells make calcitonin
- Connective tissue, blood vessels, and nerves form the lobule by surrounding follicle groups
Thyroid Hormone Synthesis
- Dietary iodide (I-) is uptaken from the blood by an iodide pump
- I- concentrates to 25-50 times plasma concentration, which is 600µg/g of tissue
- Thyroid Stimulating Hormone (TSH), iodine deficiency, and TSH receptor antibodies enhance iodide uptake
- The iodide pump is inhibited by I-, perchlorate (ClO4-), thiocyanate (SCN-), pertechnetate (TcO4-)
- H₂O₂ oxidizes I- from thyroid peroxidase to I₂ at the apical surface
- I₂ incorporates into tyrosyl residues covalently bound to thyroglobulin (TG) molecules at the apical border
- This forms monoiodotyrosine (MIT) and diiodotyrosine (DIT)
- Thyroid peroxidase couples MIT and DIT to form T3 (3,5,3'-triiodothyronine) and T4 (3,5,3',5'-tetraiodothyronine, thyroxine)
- T3 is the active hormone, and reverse T3 is not active
- Cells continually produce TG as secretory vesicles and exocytose it into the colloid
- Thyroid hormones are stored in the colloid until secretion
- TSH uses lysosomes of the TG-hormone complex to cause endocytosis and proteolysis
- T3 and T4 are released into the bloodstream
- Halogenases de-iodinate MIT and DIT, reusing free iodine and tyrosine
Transport of Thyroid Hormones
- T4 constitutes ~90%, and T3 constitutes ~10% of thyroid hormones, equalling to 80-100µg/day
- T3 and T4 are transported in plasma bound with thyroid-binding globulin, transthyretin, and albumin
- T3 is less avidly bound compared to T4
- Only the free hormone not bound to plasma proteins is biologically active
Metabolism of Thyroid Hormones
- In the periphery (liver/kidney), T4 de-iodinates to T3; most T3 comes from this pathway
- T4 plasma t1/2 life is 6-7 days, and T3 is 24-36 hours
- T3 is ~10 times more potent than T4
- T3 and T4 conjugate to glucuronide or sulphate in the liver
- This results in the excretion of conjugated forms through bile
- Iodide excretes via urine or re-circulates back to the thyroid
Regulation of Thyroid Hormone Release
- The regulation gets influenced by cold, trauma, and stress
- The hypothalamus secretes TRH
- Somatostatin and dopamine inhibit the thyroid system
- The anterior pituitary secretes TSH
- T3 and T4 act as direct negative feedback on the anterior pituitary and hypothalamus
Control of Synthesis and Release
- Thyrotrophin Releasing Hormone (TRH) is a tripeptide from the hypothalamus
- TRH stimulates release of thyrotrophin or Thyroid Stimulating Hormone (TSH) from the anterior pituitary
- TRH also releases prolactin
- Synthetic TRH (Protirelin) gets administered by intravenous injection to test thyroid function
Thyroid Stimulating Hormone (TSH)
- TSH acts on specific receptors on the basal membrane
- It increases synthesis of iodide pumps and thyroglobulin
- Synthesis and secretion of T3 and T4 increases too
- Follicular epithelium and vascularity thickness increases
- Thyroid hormones, cortisol, growth hormone, oestrogens, dopamine, and somatostatin inhibit TSH release
Mechanism of Action of Thyroid Hormones
- T3 and T4 enter cells via passive diffusion or active uptake
- T4 de-iodinates to T3 or rT3
- T3 gets transported to the nucleus, plus binds to cytosolic thyroid hormone-binding protein (CTBP)
- T3 binds to thyroid receptors (TR) in the nucleus that are bound to regulatory thyroid hormone response elements (TREs)
- Thyroid hormone receptor auxiliary protein (TRAP) is necessary to stabilize TR binding to DNA
- Stimulation/inhibition occurs of target genes
- Several TR (α1-3, β1-2) exist, with different distributions, and undetermined functions
- T3 binds to membrane-associated receptors to activate Na+/K+ ATPase pump, leading to rise of glucose and amino acids
- T3 activates mitochondria to increase energy production
Physiological Actions of Thyroid Hormones
- Increase basal metabolic rate (BMR)
Calorigenesis
- Oxygen consumption increases in all tissues except the brain, spleen, testes, and anterior pituitary, thus, heat production increases
- Important for thermoregulation
- It involves synthesis of new Na+/K+ ATPase pumps in the cell membrane and direct activation of mitochondria
- It takes 4-5 days to occur
- Blockers of Na+/K+ ATPase pumps inhibit actions of thyroid hormones
Carbohydrate, Protein and Fat Metabolism
- There is a direct effect on carbohydrates that involve increased Gl glucose absorption and synthesis of metabolic enzymes
- Indirect effects sensitize tissues to insulin, catecholamines and GH
- It boosts gluconeogenesis and glycogenolysis in the liver
- This raises glucose utilization in fat, liver, and muscle cells
- Synthesis and degradation of protein balances at low thyroid hormone levels, yet degradation predominates at high levels
- Both fat synthesis and lipolysis occur
- Lipolysis is more key
- Potentiation of catecholamine activity occurs on adipocytes
- Free fatty acids oxidation and calorigenesis increases
- Plasma cholesterol decreases by increasing liver uptake through increasing LDL receptors and bile acid formation
Maturation of the Central Nervous System
- Essential for normal CNS development during foetal and early neonatal life
- T3 and T4 do not cross the placenta
- Growth of cortical and cerebellar neurones and myelination of nerve fibres result
Skeletal Growth and Maturation
- Synergistic effects occur with GH that are essential for bone growth, development, and normal stature
- Also essential for normal functioning of nervous and cardiovascular systems, Gl tract, development of teeth, skin and hair
Need for Thyroid Hormones
- Aids responses to extremes of temperature
- The body gets maintained at 37.2°C
- When the body detects low temperature, T3 and T4 immediately release from the thyroid gland
- Tissues and mitochondria use more O2, creating heat
- Underactive thyroid gland (people feel cold) is a useful symptom
Summary of Thyroid Hormones
- Thyroid gland has a location, structure and cells
- Needs I- for hormone synthesis and storage
- Regulation of synthesis and release occurs via negative feedback, TRH, TSH
- Molecular mechanism of action has nuclear and membrane receptors
- Physiological actions increase BMR and are needed for standard development
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.