Podcast
Questions and Answers
What is the main role of thyroid cells in iodine metabolism?
What is the main role of thyroid cells in iodine metabolism?
- Transporting iodine to other endocrine glands
- Producing calcitonin for calcium regulation
- Absorbing iodine for thyroid hormone synthesis (correct)
- Excreting iodine from the body
Which of the following best describes the function of thyrotropin-releasing hormone (TRH)?
Which of the following best describes the function of thyrotropin-releasing hormone (TRH)?
- Stimulating the pituitary gland to release TSH (correct)
- Regulating calcium metabolism in the thyroid gland
- Inhibiting the release of thyroid-stimulating hormone (TSH)
- Directly stimulating the thyroid gland to produce T3 and T4
A deficiency in what substance would directly impair the thyroid’s ability to produce its hormones?
A deficiency in what substance would directly impair the thyroid’s ability to produce its hormones?
- Calcium
- Sodium
- Potassium
- Tyrosine (correct)
How do catecholamines influence the regulation of thyrotropin-releasing hormone (TRH)?
How do catecholamines influence the regulation of thyrotropin-releasing hormone (TRH)?
If a patient's thyroid gland is surgically removed, what compensatory mechanism would initially be triggered in a healthy individual?
If a patient's thyroid gland is surgically removed, what compensatory mechanism would initially be triggered in a healthy individual?
What is the functional significance of microvilli on follicular cells within the thyroid gland?
What is the functional significance of microvilli on follicular cells within the thyroid gland?
Why is the measurement of both T3 and T4 recommended for a more accurate thyroid evaluation?
Why is the measurement of both T3 and T4 recommended for a more accurate thyroid evaluation?
In a patient suspected of hyperthyroidism, what would be the expected TSH and Free T4 (FT4) levels?
In a patient suspected of hyperthyroidism, what would be the expected TSH and Free T4 (FT4) levels?
Which of the following best describes the advantage of using a third-generation TSH assay over earlier versions?
Which of the following best describes the advantage of using a third-generation TSH assay over earlier versions?
What is the primary limitation of relying solely on a TSH-centered strategy for evaluating thyroid function?
What is the primary limitation of relying solely on a TSH-centered strategy for evaluating thyroid function?
How does non-thyroidal illness (NTI) typically affect TSH levels during the acute phase of the illness?
How does non-thyroidal illness (NTI) typically affect TSH levels during the acute phase of the illness?
What information about thyroid nodules can be obtained from conducting a thyroid ultrasound?
What information about thyroid nodules can be obtained from conducting a thyroid ultrasound?
What is the primary purpose of performing a T3 uptake test?
What is the primary purpose of performing a T3 uptake test?
Which condition is suggested by the euthyroid hyperthyroxinemia result pattern of increased serum T4 and normal TSH?
Which condition is suggested by the euthyroid hyperthyroxinemia result pattern of increased serum T4 and normal TSH?
What is the significance of “delayed reflexes” as a diagnostic indicator?
What is the significance of “delayed reflexes” as a diagnostic indicator?
What is the goal of intentional TSH suppression using thyroxine in patients with thyroid cancer?
What is the goal of intentional TSH suppression using thyroxine in patients with thyroid cancer?
How long should clinicians typically wait after initiating or adjusting thyroxine dosage before re-testing TSH levels?
How long should clinicians typically wait after initiating or adjusting thyroxine dosage before re-testing TSH levels?
When monitoring a pregnant individual, what thyroid function test is temporarily suppressed during the first trimester of pregnancy?
When monitoring a pregnant individual, what thyroid function test is temporarily suppressed during the first trimester of pregnancy?
In the context of the TRH stimulation test, what does a prompt increase in TSH suggest?
In the context of the TRH stimulation test, what does a prompt increase in TSH suggest?
A patient presents with low T4 and increased TSH levels. How would you describe this condition?
A patient presents with low T4 and increased TSH levels. How would you describe this condition?
Flashcards
Thyroid Gland
Thyroid Gland
Small, butterfly-shaped gland in the anterior neck, consisting of two lobes connected by an isthmus.
Thyroid Follicles
Thyroid Follicles
Functional units of the thyroid, lined by epithelial cells and filled with colloid.
TRH Definition
TRH Definition
Modified tripeptide hormone that stimulates the pituitary to release TSH.
TSH definition
TSH definition
Signup and view all the flashcards
Graves' Disease
Graves' Disease
Signup and view all the flashcards
T3 Thyrotoxicosis
T3 Thyrotoxicosis
Signup and view all the flashcards
Primary Hypothyroidism
Primary Hypothyroidism
Signup and view all the flashcards
Second Generation TSH Assay
Second Generation TSH Assay
Signup and view all the flashcards
Free T4
Free T4
Signup and view all the flashcards
Non-Thyroidal Illness (NTI)
Non-Thyroidal Illness (NTI)
Signup and view all the flashcards
Primary Hyperthyroidism
Primary Hyperthyroidism
Signup and view all the flashcards
Secondary Hypothyroidism
Secondary Hypothyroidism
Signup and view all the flashcards
Tertiary Hypothyroidism
Tertiary Hypothyroidism
Signup and view all the flashcards
TBG
TBG
Signup and view all the flashcards
Commoon RIA Test
Commoon RIA Test
Signup and view all the flashcards
Goiter Definition
Goiter Definition
Signup and view all the flashcards
T3 Uptake
T3 Uptake
Signup and view all the flashcards
Conflicting TSH and FT4 levels
Conflicting TSH and FT4 levels
Signup and view all the flashcards
Study Notes
- Thyroid cells are solely responsible for iodine absorption
- Iodine combines with tyrosine, an amino acid
- This combination produces triiodothyronine (T3) and thyroxine (T4)
- T3 and T4 are discharged into the bloodstream to regulate metabolism
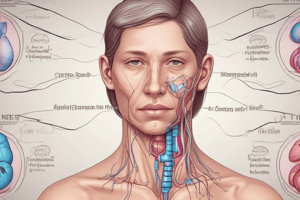
Normal Thyroid Gland
- A small, butterfly-shaped gland
- Composed of two lobes that are connected by an isthmus
- Located in the anterior neck, hugging the trachea around the 2nd to 3rd tracheal rings or C5-C7 vertebrae
- Produces 80% T4 and 20% T3
- Function units are called follicles, which can vary in size and are lined by epithelial cells surrounding a colloid space
- Function is to uptake iodine and convert it into thyroid hormones like thyroxine (T4) and triiodothyronine (T3)
- Follicle cells are lined by epithelial cells ranging from simple cuboidal to simple columnar
- Weighs 15 to 25 g
- Consists of two lobes connected by a narrow isthmus
- Divided into lobules, each composed of 20 to 40 follicles separated by connective tissue
- Follicles are ring-shaped structures where a single cell band of follicular cells surrounds a closed cavity that contains colloid, thyroid hormone, thyroglobulin (Tg), and glycoproteins
- Follicular cells have microvilli that extend into the colloid, for iodination, exocytosis, and the initial phase of hormone secretion
- Parafollicular or C cells synthesize and secrete calcitonin, a hormone important for calcium metabolism
- Under the control of the pituitary gland
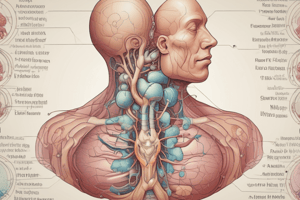
Regulators of Thyroid Gland Function
- Thyrotropin-Releasing Hormone (TRH) is regulated by the Hypothalamus
- Is a modified tripeptide derived from a large prepro-TRH molecule
- Acts on the production of pituitary hormones, especially prolactin
- Found in the hypothalamus, brain, C cells of the thyroid gland, β cells of the pancreas, myocardium, prostate, testis and spinal cord
- Neuron bodies producing TRH are innervated by catecholamine
- Leptin plays a significant role in the regulation of the TRH regulating appetite
- Somatostatin-containing axons
Thyroid-Stimulating Hormone (TSH)
- Pituitary Hormone
- Glycoprotein consisting of two monocovalently linked α and β subunits
- α subunit has the same amino acid sequences as LH, FSH, and human chorionic gonadotropin (hCG)
- β subunit carries specific information to the binding receptors for expression of hormonal activities
- Radioimmunoassay for measuring TSH was first developed in 1965
First Generation Assay
- Did not have sufficient sensitivity to distinguish normal TSH levels from suppressed levels in Primary Hyperthyroidism
Second Generation Immunomeric TSH Method
- Used in the mid 1980s
- Uses monoclonal or polyclonal antibodies
- Improved sensitivity to 0.1 to 0.2 mU/L
Third Generation Assay
- Now in common use.
- Allows measurement down to about 0.005 mU/L
- Provides sufficient sensitivity for the vast majority of clinical applications
- The ATA recommends this assay be able to quantitate TSH in the 0.010 to 0.020 mU/L range on an interassay results
Fourth Generation Assay
- Developed recently
- Sensitivity of 0.0004 mU/L
- Not widely available
- Serum TSH is <0.004 mIU/L in patients with severe hyperthyroidism
Functional Sensitivity
- Defined by ATA as the point at which the interassay precision has a coefficient of variation equal to less than 20%
TSH Assay
- Can identify virtually all instances of hyperthyroidism and hypothyroidism
- Exceptions are damage to the hypothalamus or pituitary gland, thyroid hormone resistance, or interference with normal functioning of the HPT axis due to medication
TSH Normal Results
- Approximately 0.5 and 5.0 mIU/L in most laboratories
Hyperthyroid Patients
- Have suppressed TSH values, except for individuals who have hyperthyroidism caused by TSH-producing tumors or other diseases such as pituitary resistance to thyroid hormone
Subclinical Hyperthyroidism
- Defined by the presence of low TSH with normal levels of T4 and T3
Subclinical Hypothyroidism
- Describe patients with elevated TSH but with normal levels of T4, T3 and FT4
Nonthyroidal Illness (NTI)
- Patients tend to have low TSH results during their acute illness
- TSH rises to within or above the reference range with resolution of the underlying illness
- TSH levels turn to normal once the acute illness has resolved
- These medications suppress TSH: glucagon, opioids, glucocorticoids and dopamine
TSH-Centered Strategy Limitations
- Assumes hypothalamic-pituitary function is intact and normal
- Assumes patient is stable without recent hyperthyroidism or hypothyroidism therapy
- The serum TSH result can be misleading if the above criteria are not met.
Confirming Thyroid Dysfunction
- Measure FT4 with or without total T4, in addition to TSH
Serum Free T3 and TSH
- Are appropriate to patients suspected of hyperthyroidism with a normal to low-normal T4 (T3 thyrotoxicosis)
Free T4 and Free T3
- Serum
Pituitary Gland
- Regulated by the hypothalamus
- Produces TRH to stimulate pituitary gland to release TSH
- Under control of the Pituitary Gland:
- When thyroid hormone level is low, the pituitary gland produces TSH
- TSH stimulates the thyroid gland to produce more hormones
- This raises the level in the blood, and the pituitary senses this, causing decreased TSH production
Commonly Used Thyroid Tests
- Measurement of serum thyroid hormones by radioimunoassay (RIA)
Serum T4
- Most used thyroid test
- Reflects the amount of thyroxine in the blood
- Thyroxine (T4) represents 80% of thyroid hormone and generally represent overall function of the gland
- Good measure of thyroid function if patient does not take any type of thyroid medication
Thyroxine (T4)
- After release from thyroid follicles, Thyroxine will bind to proteins in the blood
- The thyroid-binding globulin, albumin or thyretin
- Can be measured by immunoassay
- Reference Range: 5 to 12.5 ug/dL in adults (slightly lower results in certain pediatric age groups)
- Thyroxine measurements are often used along with TSH (can be important in interpreting TSH results)
Primary Hypothyroidism
- Low T4, Increased TSH
Primary Hyperthyroidism
- Elevated T4 and T3, Decreased TSH
T4 Thyrotoxicosis
- Elevated Serum T4, Serum T3 within reference range or low
- Can occur in patients with iodine-induced thyrotoxicosis or patients in beta blockers
Factors Affecting Thyroid Tests
- Amiodarone
- Large doses of steroids
- Thyrotoxic patients with NTI
T3 Thyrotoxicosis
- Suppressed TSH, Normal to low-normal T4 and High T3
- More common in a toxic nodule
Low T4 and T3 Syndrome
- Low T4, Low T3
- Severe nonthyroidal illness
- Associated with poor prognosis
- Adaptive response to reduce metabolic demands and conserve protein stores
- Thought to arise from a maladjusted central inhibition of TRH
Euthyroid Hyperthyroxinemia
- Increased Serum T4, Normal TSH
- Increased binding proteins as may be seen with certain drugs (e.g., estrogen)
- Medical conditions (e.g., liver disease)
- Hospitalized for psychiatric illness and in patients with familial dysalbuminemia
T3 Uptake (T3-UP) Test
- Assess T4 measurement by checking binding sites
- Measure unoccupied binding sites of all proteins
- Saturate available binding sites with 3 and measure the unbound 3
Free Thyroxine Index (FTI)
Patient’s Total T4) X (T3-UP of the Patient)/(Mean T3-UP of the Reference Population)
- Reference Range: 5.4 to 9.7
- Estimate of the free T4 concentration
- Largely replaced by the direct measurement of Free T4 by immunoassay, dialysis or ultrafiltration
Serum T3
- Represent 20%
- Sometimes the diseased thyroid gland will start producing very high levels of T3 but still produce normal level of T4
- Measurement of both hormones provide an even more accurate evaluation of thyroid function
Triiodothyronine (T3)
- Generally measured by immunoassay
- Reference Interval: 60 to 160 ug/dL (0.9 to 2.46 nmol/L)
- T3 is much less bound to serum protein than T4; thus, a relatively greater proportion of T3 than T3 exists in the free, diffusible state
- Elevated TBG will cause elevated T3
- Measurement of Serum T3 is not useful in evaluating patients suspected of having hypothyroidism because serum T3 levels are within the reference interval in 15% to 30% of hypothyroid patients
- Serum T3 concentrations are low in cord blood but increase rapidly during the first hours of life
- Administration of T3 results in a peak within 2 to 4 hours
- Serum T3 levels do not show a peak in patients treated daily with T4
- Total T3 concentrations are measured by competitive immunoassay methods that are now mostly nonisotopic and use enzymes, fluorescence, or chemiluminescence molecules as signals
Total T3 Measurement
- Is helpful in confirming the diagnosis of hyperthyroidism, especially in patients with no or minimally elevated T4 or ambiguous clinical manifestation
Serum T3 Levels
- Can be in the reference range or low in patients with hyperthyroidism if there is coexistent NTI
- Or if patients are on drugs that decrease the conversion of T4 to T3 (e.g., propranolol, amiodarone)
T3 Thyrotoxicosis
- Elevated Serum T3 but normal T4 and free T4
- Heterogenous group with no distinctive signs or symptoms
- Most patients have Graves' disease
- May also occur in patients with other causes of hyperthyroidism such as: Toxic nodular goiter or Toxic adenoma
- About 1% to 4% of thyrotoxic patients have T3 thyrotoxicosis, except in regions of iodine deficiency, where it is more common
Thyroid Binding Globulin (TBG)
- Most of the thyroid hormones in blood are attached to TBG
- If there is excess or deficiency, it alters T3 or T4 measurement
- Does not affect action of hormone
- If with normal thyroid function + unexplained high or low T4 or T3 → may be due to an increase/decrease of TBG
- Causes no problem except falsely elevating/lowering the T4 level → misdiagnosed as hyperthyroid/hypothyroid
Thyroxine-Binding Globulin (TBG)
- The main serum carrier protein for both T4 and T3
- Measurement may be helpful in patients who have serum T4 and T3 levels that do not agree with other laboratory parameters of thyroid function
- Measured by immunoassay
- Range: 13 to 39 ug/dL (150 to 360 nmol/L) in healthy individuals
- Inherited abnormalities include: complete of partial deficiency
Pituitary Production of TSH
- Measured by immunoradiometric Assay (IRMA)
- Normally: Low level of TSH are sufficient to keep normal thyroid gland functioning properly
- Early Hypothyroidism – TSH become elevated even though T3 and T4 may still be within "normal" range
- Rise in TSH represent the Pituitary response to a drop in circulating thyroid hormone and can be a first indication of Thyroid Gland failure
- TSH is usually used in combination with T4 and T3
TRH Stimulation Test
- Helpful in the diagnosis of patients with confusing Thyroid function test
- Involves determining basal TSH level administer bolus of TRH and measures TSH 15 to 30 minutes after
- Normal is:
- Baseline TSH (5 or less)
- Give TRH to increase TSH up to 10-20
Primary Hyperthyroidism
- TS are low. TRH causes little to no rise in TSH
Primary Hypothyroidism
- TRH causes a prompt increase in TSH to compensate
Secondary Hypothyroidism
- TRH causes no increase in TSH
Tertiary Hypothyroidism
- TRH causes delayed (1-2 hours) increase in TSH
Iodine Uptake Scan
- Measure how much iodine is taken up by the thyroid gland (RAI uptake)
- The test is performed by giving a dose of radioactive iodine, the iodine is concentrated in the thyroid gland and the amount of iodine that goes into the thyroid gland that can be measured is by a "thyroid uptake"
- Hypothyroid patients take up too little iodine
- Hyperthyroid patients take up too much iodine
Thyroid Scan
- Measure how well the thyroid gland is functioning
- Require giving a radioisotope to the thyroid gland
Technetium (Radioisotope)
- Will be concentrated by the thyroid gland
- Will not measure iodine uptake
- Usually done at the same time that the iodine uptake test is performed
- Used for identifying nodules, measure the size of the goiter prior to treatment, in the follow-up of thyroid cancer patients after surgery and for locating thyroid tissue outside the neck
- Identify where nodules are hot or cold. Increased hormone uptake is hot nodule. Decreased uptake is cold nodule. A malignant 1 nodules is 1 in10 chance to be malignent.
Thyroid Ultrasound
- Obtain images of the thyroid gland and identify nodules
- Cannot tell if a nodule is benign or malignant
- Allows accurate measurement of the nodule size
- Aids in performing Thyroid Needle Biopsy
Thyroid Needle Biopsy
- Provide definitive information
Thyroid Function Test Recommendations
- Commonly ordered tests are TSH, FT4, and FT3
- Asymptomatic patients are not screened for thyroid dysfunction because there is low likelihood of thyroid disease, but may still be tested if there are symptoms and risk factors
- TSH is used as the sole test of thyroid function in most situations as a more sensitive indicator
When to Test
- Clinical assessment and judgment remain paramount
- Initial testing for thyroid dysfunction should be based on clinical suspicion
Signs and Symptoms of Thyroid Disease
- Hypothyroidism includes Goiter, Delayed reflexes, Fatigue, Family History, Weight gain, and intolerance to cold
- Hyperthyroidism includes Goiter, Thyroid bruit, lid lag, Proptosis, Fatigue, Family History, Weight loss, and intolerance to heat
Study by Bandolier in 1997
- Showed that in patients with high suspicion, 78% had thyroid disease and in patients with intermediate symptoms, 2.9% suffered from thyroid disease
Appropriate to Test only TSH?
- There are conditions wherein it is inappropriate to test for TSH only
Central (Secondary) Hypothyroidism
- Pituitary failure:
- Request TSH and FT4
- Result will be a normal TSH with decreased FT4
Non-Compliance with Replacement Therapy
- Elevated TSH. Request TSH and FT4
- Result will be a discordant serum value (high TSH/ high FT4)
Early Stages of Therapy
- During early stages of therapy, testing TSH alone is inappropriate
- During the first 2 months of treatment, the thyroid is still unstable
- TSH has not reached equilibrium and measuring FT4 becomes a more reliable test
Combination Results
- High Irregular /SubclinicalPrimary TSH use ofthyroxine hypothyroidism hypothyroidism
- Normal Amiodarone/T4 under (problem inNormalto slight Thyroiditselft TSH pituitaryhypothyroidism replacement increased hypothyroidism
- Drugs Severe, Drugs. Pituitary to slight thyroiditis Hypothyroidism.
- TSH and FT 4 should be normal and the range is broad and this does not include non-thyroidal cases
- Non - Thyroidal illnesses
FT3 (non-thyroidal illness) is high
- Non - thyroidal cases
Thyroxine administration
1 month will make the test accurate
8 week testing period
8 week period after thyroxine
Anti-thyroids
May stay suppressed for approximately 3 to 6 months
Pregnancy tests recommendable
Because the hormones are already functioning
Thyroid cancers - Intentionally
- To cause the TSH to function less because TSH has more tumor reoccurrences
Pregnant Tests non recommends
- As they already may be suppressed
Hypothyroidism in pregnant tests, treat even at a slight increase to prevent miscarriage
Low:
- Irregularly/subclinical, primary High: -Amiordarone
- T4: administration errors
- Hypothryoid
TSH :
1st for line: assess thyroid function- More sensible primary test- A4 metabolic activity
FT4 with FT3 with little testing specificity
If on thyroxine treatment is needed:
6.8 weeks as to what to 8. Long is not what the lab has to test to 6. Every change in the dose requires 6-8 weeks 7. If dose is the result
TSH administration should be followed after 2-48 weeks for stability in results
- Monitor TSH with thyroid anti-medication medication (3-6) -Recheck the TSH every 1-2 weeks till stabilization -Then recheck again every 8 weeks for stability
If TSh is under 0.5 with hyper-thyroidism suspected
- Test or retest will show a normal result
- A follow up test is given for the FT3 because an abnormality might be located there with the F4 test with show it normal
Hypo FT4
-If low, replace thyroid and let retest
- Is an elevated increase after with hypo due to TSH
FT4
Thyroid tests in the first trimeters of pregnancy are not recommended due to the effects of chorionic administration stimulating hormone stimulation
-Nonthyroid
- Test: for acute illnesses as well
- Measure Thyroid : Cancer
Cancer from hormones
- Cause more sensitivity than needed -So treatment in the long run happens TSH measures : - Metablollic and free
To high with thyroxine T3-FT:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.