Podcast
Questions and Answers
What type of trauma involves injuries from road traffic accidents?
What type of trauma involves injuries from road traffic accidents?
- Thermal trauma
- Iatrogenic trauma
- Penetrating trauma
- Accidental trauma (correct)
Which of the following is a direct effect of thoracic trauma?
Which of the following is a direct effect of thoracic trauma?
- Infarction
- Pneumonia
- Acute respiratory distress syndrome
- Flail chest (correct)
Which injury is associated with penetrating thoracic trauma?
Which injury is associated with penetrating thoracic trauma?
- Fracture rib
- Pneumothorax
- Hemothorax
- Laceration of the lung (correct)
What type of trauma is characterized by injuries from sharp objects, such as knives or swords?
What type of trauma is characterized by injuries from sharp objects, such as knives or swords?
Which of the following complications can occur as a delayed effect of thoracic trauma?
Which of the following complications can occur as a delayed effect of thoracic trauma?
What is a potential effect on the chest wall due to thoracic trauma?
What is a potential effect on the chest wall due to thoracic trauma?
Which type of thoracic trauma can result from a fall from a height?
Which type of thoracic trauma can result from a fall from a height?
Which of the following best describes an immediate effect of mediastinal injury?
Which of the following best describes an immediate effect of mediastinal injury?
Which procedure is NOT typically performed to clear airway obstruction?
Which procedure is NOT typically performed to clear airway obstruction?
What is the first step in the resuscitation phase of thoracic trauma management?
What is the first step in the resuscitation phase of thoracic trauma management?
Which of the following is a life-threatening thoracic injury?
Which of the following is a life-threatening thoracic injury?
Which mnemonic is used for neurological assessment in trauma patients?
Which mnemonic is used for neurological assessment in trauma patients?
What is the purpose of the Extended FAST (eFAST) examination?
What is the purpose of the Extended FAST (eFAST) examination?
Which of the following is NOT considered a method for stabilizing the chest wall?
Which of the following is NOT considered a method for stabilizing the chest wall?
What is indicated by the presence of massive hemothorax?
What is indicated by the presence of massive hemothorax?
What imaging technique is used primarily for assessing blood around the heart after trauma?
What imaging technique is used primarily for assessing blood around the heart after trauma?
Which of the following is NOT considered a potential life-threatening injury?
Which of the following is NOT considered a potential life-threatening injury?
What is the primary purpose of a tertiary survey in trauma cases?
What is the primary purpose of a tertiary survey in trauma cases?
What is the typical clinical presentation of surgical emphysema?
What is the typical clinical presentation of surgical emphysema?
In the context of rib fractures, what is a common complication that can arise?
In the context of rib fractures, what is a common complication that can arise?
Which imaging technique is primarily used for diagnosing rib fractures?
Which imaging technique is primarily used for diagnosing rib fractures?
What is one of the general effects of rib fractures on respiratory function?
What is one of the general effects of rib fractures on respiratory function?
What is the appropriate initial treatment approach for surgical emphysema?
What is the appropriate initial treatment approach for surgical emphysema?
Which type of trauma can lead to mediastinal emphysema?
Which type of trauma can lead to mediastinal emphysema?
What is the primary treatment approach for flail chest?
What is the primary treatment approach for flail chest?
Which type of rib fracture is associated with a higher risk of injury to the brachial plexus or subclavian vessels?
Which type of rib fracture is associated with a higher risk of injury to the brachial plexus or subclavian vessels?
What is the mechanism by which hypoxaemia occurs in flail chest?
What is the mechanism by which hypoxaemia occurs in flail chest?
Which of the following is NOT typically included in the investigations for flail chest?
Which of the following is NOT typically included in the investigations for flail chest?
What is the paradoxical movement in flail chest?
What is the paradoxical movement in flail chest?
What prevention strategy can help reduce the incidence of injuries leading to flail chest?
What prevention strategy can help reduce the incidence of injuries leading to flail chest?
Which type of flail chest is considered the least dangerous?
Which type of flail chest is considered the least dangerous?
In cases of rib fractures, which condition might occur if adequate pulmonary toilet is not performed?
In cases of rib fractures, which condition might occur if adequate pulmonary toilet is not performed?
What is a common method for stabilizing the external chest wall in emergencies?
What is a common method for stabilizing the external chest wall in emergencies?
Which condition is characterized by the presence of air in the pleural cavity?
Which condition is characterized by the presence of air in the pleural cavity?
What type of pneumothorax is typically caused by a rupture of an apical bleb?
What type of pneumothorax is typically caused by a rupture of an apical bleb?
Which method is NOT used for airway suctioning in patients with respiratory distress?
Which method is NOT used for airway suctioning in patients with respiratory distress?
When should mechanical ventilation be considered according to blood gas levels?
When should mechanical ventilation be considered according to blood gas levels?
What is the primary purpose of incentive spirometry?
What is the primary purpose of incentive spirometry?
Which imaging technique is commonly used to diagnose a fractured sternum?
Which imaging technique is commonly used to diagnose a fractured sternum?
What classification of pneumothorax is associated with iatrogenic causes?
What classification of pneumothorax is associated with iatrogenic causes?
Flashcards are hidden until you start studying
Study Notes
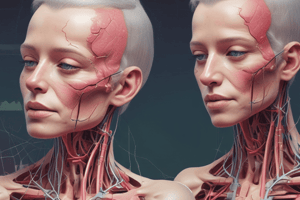
Types of Thoracic Trauma
- Accidental, Iatrogenic, Chemical, Thermal, Barotrauma, and Blast Injuries
- Accidental Trauma
- Blunt trauma: Road traffic accidents (RTA), falls from a height, trauma by blunt objects
- Penetrating trauma: Stab wounds by knife, sword, or sharp objects
- Iatrogenic Trauma
- Occurs from medical interventions
- Chemical Trauma
- Exposure to toxic chemicals
- Thermal Trauma
- Burns or heat-related injuries
- Barotrauma and Blast Injuries
- Pressure changes from explosions or mechanical ventilation
Effects of Thoracic Trauma
- Immediate Effects
- Chest wall: Fracture ribs, Flail chest, Fracture sternum
- Pleura: Pneumothorax, Hemothorax, Chylothorax
- Lung: Contusion, Laceration, Hematoma
- Mediastinum: Traumatic asphyxia, Pneumomediastinum
- Tracheobronchial injury, Oesophageal trauma, Diaphragmatic trauma
- Heart and Great Vessels: Pericardial injury, Haemopericardium, Myocardial contusion, Cardiac rupture, Coronary injury, Injury of great vessels
- Thoracic duct injury
- Delayed Effects or Complications
- Pulmonary: Atelectasis, Acute respiratory distress syndrome, pneumonia, infarction, lung abscess, AV- fistulae, bronchial stenosis, organized hematoma
- Pleural: Empyema, clotted hemothorax, fibrothorax, bronchopleural fistula, chylothorax, diaphragmatic hernias
- Mediastinum: Mediastinitis, Pericarditis
- Vascular: Thromboembolism, Pseudoaneurysm, air embolism
Pathophysiology of Thoracic Trauma
- Injury to the chest wall can lead to disruption of the pleural cavity, lung parenchyma, and mediastinum
- This can cause air and blood to accumulate in the pleural space, resulting in pneumothorax, hemothorax, or hemopneumothorax
- The injury can also damage the lung itself, leading to contusions, lacerations, and hematomas
- Damage to the mediastinum can lead to traumatic asphyxia, pneumomediastinum, and injury to the great vessels
- Injury to the heart and great vessels can cause pericardial tamponade, myocardial contusion, and cardiac rupture
Primary Survey: Resuscitation Phase
- ABCDE (Airway, Breathing, Circulation, Disability, Exposure)
- Airway: Ensure a patent airway by:
-
Suctioning is a critical procedure used to clear the airway of secretions, blood, or foreign materials that can obstruct normal breathing. This technique is essential in emergency and critical care settings, particularly for patients who are unable to adequately clear their airways due to reduced consciousness, respiratory illness, or mechanical ventilation. The procedure involves the use of a suction device, which can be either manual or automated, to remove the impediments from the trachea or oral cavity. Effective suctioning requires proper technique to minimize trauma to the tissues and prevent complications such as hypoxia or bradycardia. It is vital to monitor the patient's oxygen saturation and heart rate during and after suctioning to ensure their safety and response to the procedure. Proper indications for suctioning include a visible obstruction, abnormal breath sounds such as wheezing or gurgling, and signs of respiratory distress. After suctioning, it is important to reassess the airway and breathing status to determine if further interventions are needed.
In summary, suctioning plays a vital role in airway management and is essential for ensuring adequate ventilation in patients with compromised respiratory function.
(oral, nasopharyngeal, nasotracheal)
-
Oral or nasal airway
-
Endotracheal or endobronchial tube
-
Cricothyroidotomy
-
Tracheostomy
-
Bronchoscopy
-
- Breathing: Manage respiratory distress by:
- Oxygen inhalation
- Close chest wall defects (open pneumothorax)
- Expand lung by intercostal tube drainage (ICTD)
- Stabilize chest wall
- Blood gas analysis
- Mechanical Ventilation
-
Circulation: Manage circulatory compromise by:
- Large-bore venous access is essential for administering blood products, medications, and fluids in emergencies. It facilitates rapid fluid resuscitation and can be used for blood sampling and monitoring central venous pressure.
- The CVP (Central Venous Pressure) line is typically inserted into a central vein, allowing for accurate measurement of heart function and venous return while also providing access for therapies.
- Volume resuscitation
- Stop bleeding through interventions such as intercostal tube drainage (ICTD) and thoracotomy procedures.
-
- It is important to evaluate for any underlying conditions that could lead to circulatory compromise. Take into account potential causes such as cardiac tamponade, which should be promptly identified and treated, as it can severely impact the patient's hemodynamic stability.
- Disability/Neurologic Assessment: Assess neurological status using:
- AVPU (alert, verbal stimuli response, painful stimuli response, or unresponsive)
- Glasgow Coma Scale
- Exposure and Environmental Control: Undress the patient and cover them with warm blankets to prevent hypothermia
- Airway: Ensure a patent airway by:
Immediate Life-Threatening Injuries
- Airway obstruction
- Tension pneumothorax
- Open pneumothorax
- Massive hemothorax
- Cardiac tamponade
- Massive flail chest
Secondary Survey
- More thorough examination and investigations should be performed after the primary survey
- Chest X-ray
- CT scan
- MRI
- Ultrasound (FAST & eFAST)
- Focused Assessment with Sonography for Trauma (FAST): Rapid bedside ultrasound examination for blood around the heart (pericardial effusion) or abdominal organs (hemoperitoneum) after trauma
- Extended FAST (eFAST): Examination of both lungs using bilateral anterior thoracic sonography in addition to FAST
- ECHO (Echocardiography)
- Angiography
- Upper GIT Studies
Potential Life-Threatening Injuries
- Cardiac contusion
- Deceleration aortic injury
- Tracheo-bronchial rupture
- Diaphragmatic rupture
- Oesophageal perforation
- Pulmonary contusion
Tertiary Survey
- Serial assessments and examinations should be performed to identify missed injuries and related problems
- Delayed diagnosis can occur in up to 10% of cases
Thoracic Cage Injuries
- Surgical Emphysema
- Presence of air in subcutaneous tissue due to surgical causes or infection
- Etiology:
- Fractured rib injuring underlying lung
- Tracheobronchial tears
- Penetrating chest injury and open pneumothorax
- Mediastinal emphysema
- Ruptured oesophagus
- After intercostal tube insertion
- Presentation:
- Presence of air under the skin with crackling sensation (subcutaneous crepitation)
- Localized or rapidly progressive
- Treatment:
- Usually resolves spontaneously
- Identify and manage the underlying cause
- Evacuation with needles, skin incisions, or subcutaneous catheters if extensive
- Fracture Ribs
- Etiology:
- Direct violence
- Indirect violence
- Muscular violence
- Effects:
- Severe pain, decreased respiratory movements, ineffective coughing, Atelectasis, pneumonia
- Injury of underlying pleura and lung
- Injury of intercostal bundle
- Clinical Picture:
- Severe pain
- Localized tenderness
- Crepitus
- Surgical emphysema
- Look for associated Hemopneumothorax
- Diagnosis:
- Plain chest X-ray (Rib view)
- Multi-slice CT scan (Skeleton view)
- Treatment:
- Systemic analgesics
- Intercostal nerve block (fracture of less than 4 ribs)
- Epidural analgesia (in fracture of more than 4 ribs)
- Avoid binders, tape, or strapping
- Complications:
- First rib fracture may be associated with brachial plexus or subclavian vessels injury
- Lower ribs fracture may be associated with trauma to the spleen or liver
- Etiology:
- Flail Chest
- Definition: Paradoxical movement of a segment of chest wall due to fractures of three or more ribs broken in two or more places
- Etiology: Severe blunt trauma
- Types: Anterior, Lateral, Posterior, Flail Sternum
- Pathophysiology:
- Hypoxaemia due to:
- Underlying pulmonary contusion
- Pain of rib fractures
- Associated hemopneumothorax or cardiac trauma
- Hypoventilation of the underlying lung from paradoxical respiration
- Mediastinal flutter with kink of great vessels
- Pendulum-like movement of dead space air
- Hypoxaemia due to:
- Presentation:
- Severe blunt trauma
- Severe chest pain of rib fractures
- Dyspnea, tachypnea, and cyanosis
- Hypotension and tachycardia
- Paradoxical movement of the flail segment
- Chest wall contusions ± surgical emphysema
- Investigations:
- Chest X-ray: Flail chest is a clinical finding, not a radiological one
- CT scan chest
- Multislice CT (MSCT) scan chest wall
- Blood gas analysis
- Prevention: Safer Automobiles, seat belts, air bag design
- Prognosis: 5-10% mortality depending on severity of injury, age, bilaterality, and number of ribs fractured
- Treatment:
-
Oxygen inhalation
-
Pain relief: Systemic analgesics, patient-controlled analgesia (PCA) machines, intercostal nerve block
-
Epidural catheter
-
Pulmonary toilet refers to a set of therapeutic interventions aimed at maintaining or improving airway patency and facilitating bronchial hygiene. This procedure is particularly important for patients who have difficulty clearing mucus or secretions from their airways due to conditions such as chronic obstructive pulmonary disease (COPD), pneumonia, or after surgical procedures that affect respiratory function. The pulmonary toilet techniques can include:
-
Chest Physiotherapy: This comprises manual techniques such as percussion and vibration to help dislodge mucus from the lungs so it can be expectorated more easily.
-
Postural Drainage: Involves positioning the patient in specific ways to allow gravity to assist in draining fluid from different areas of the lungs.
-
Incentive Spirometry: A device that encourages patients to take deep breaths, which can help expand the lungs and enhance mucus clearance.
-
Suctioning: A mechanical method used to remove secretions from the airways, especially in patients who are unable to clear mucus voluntarily.
-
Humidification: Adding moisture to the inspired air, which can help thin secretions, making it easier for patients to cough them out.
-
Medication: Use of bronchodilators and mucolytics may also form part of the pulmonary toilet strategy to loosen mucus and open up the airways.
Regular and effective pulmonary toilet is crucial to prevent complications such as atelectasis, infection, and respiratory failure, especially in patients with compromised respiratory systems.
Clearing secretions from the airways to prevent atelectasis
-
-
Stabilization:
- External chest wall stabilization by compressive dressing strapping
- CPAP (Continuous Positive Airway Pressure) by mask
- IPPV (Intermittent Positive Pressure Ventilation) by tracheal intubation and mechanical ventilation
- Internal chest wall stabilization by orthopedic devices (Judet struts or Kirschner [K-] wires)
-
- Fracture Sternum
- Transverse fractures near the manibriosternal junction
- Diagnosis:
- Lateral X-ray chest
- CT scan to exclude associated injuries
- Treatment:
- Analgesia and follow up in most cases
- IPPV, or Intermittent Positive Pressure Ventilation, is a mechanical ventilation technique that provides positive pressure breaths to patients who are unable to breathe adequately on their own. It is particularly useful in situations such as respiratory failure, severe airway obstruction, or during surgical procedures where general anesthesia is involved. With IPPV, the ventilator delivers air into the lungs through a mask or endotracheal tube at set intervals, aiding in gas exchange and preventing respiratory muscle fatigue. This method can help ensure that the body receives sufficient oxygen while also expelling carbon dioxide, thereby maintaining proper respiratory function. It is essential to monitor the patient's response to IPPV closely, as adjustments may be necessary based on their individual condition and needs.and/or operative reduction in severe cases
Pleural Space Injuries
- Pneumothorax
- Definition: Presence of air in the pleural cavity
- Etiology:
- Spontaneous:
- Primary: Ruptured apical bleb
- Secondary: Associated with preexisting lung disease (Chronic obstructive lung disease, Cystic fibrosis, Infection, Tumors, Catamenial, Miscellaneous)
- Traumatic:
- Iatrogenic: Lung biopsy, central line insertion, barotrauma, postoperative, after thoracocentesis
- Penetrating or blunt chest trauma: Disruption of tracheobronchial tree, pulmonary parenchyma, esophageal perforation, open pneumothorax
- Spontaneous:
- Types:
- Communication:
- Open Pneumothorax: Open wound in the chest wall communicating with the pleural space
- Tension Pneumothorax: One-way valve mechanism where air enters the pleural space but cannot escape
- Non-Communication:
- Simple Pneumothorax: No communication with the atmosphere
- Traumatic Pneumothorax: caused by blunt or penetrating trauma
- Communication:
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.