Podcast
Questions and Answers
What percentage of traumatic deaths is thoracic trauma directly responsible for?
What percentage of traumatic deaths is thoracic trauma directly responsible for?
- 15%
- 30%
- 25%
- 20% (correct)
Which type of trauma has a higher percentage of being managed without surgical intervention?
Which type of trauma has a higher percentage of being managed without surgical intervention?
- Heart trauma
- Skeletal trauma
- Blunt trauma (correct)
- Penetrating trauma
What is a primary characteristic of blunt thoracic injuries?
What is a primary characteristic of blunt thoracic injuries?
- Immediate need for surgical intervention
- Forces distributed over a large area (correct)
- Forces concentrated in a small area
- Localized damage to organs
Which classification of chest injuries includes damage to the diaphragm?
Which classification of chest injuries includes damage to the diaphragm?
What mechanism is commonly associated with penetrating thoracic injuries?
What mechanism is commonly associated with penetrating thoracic injuries?
How many deaths do chest injuries account for annually in the United States?
How many deaths do chest injuries account for annually in the United States?
Which type of injury leads the statistics in thoracic trauma as the second leading cause of trauma deaths?
Which type of injury leads the statistics in thoracic trauma as the second leading cause of trauma deaths?
What is the main purpose of ventilation in the respiratory system?
What is the main purpose of ventilation in the respiratory system?
Which of the following conditions is NOT a result of impairments in cardiac output?
Which of the following conditions is NOT a result of impairments in cardiac output?
What is a classic symptom of clavicular fractures?
What is a classic symptom of clavicular fractures?
In assessing a patient with potential pleural injury, which finding would indicate significant respiratory distress?
In assessing a patient with potential pleural injury, which finding would indicate significant respiratory distress?
Which physiological process involves the exchange of oxygen and carbon dioxide?
Which physiological process involves the exchange of oxygen and carbon dioxide?
What is a common cause of rib fractures in elderly patients?
What is a common cause of rib fractures in elderly patients?
What is indicated by the presence of narrowed pulse pressure in a patient?
What is indicated by the presence of narrowed pulse pressure in a patient?
Which of the following assessment findings may suggest a mediastinal injury?
Which of the following assessment findings may suggest a mediastinal injury?
What management strategy is often used for significant airway obstruction?
What management strategy is often used for significant airway obstruction?
What is a primary consequence of mediastinal shift in tension pneumothorax?
What is a primary consequence of mediastinal shift in tension pneumothorax?
Which of the following is considered a late sign of tension pneumothorax?
Which of the following is considered a late sign of tension pneumothorax?
What is the most critical step in managing tension pneumothorax?
What is the most critical step in managing tension pneumothorax?
Which of the following findings is NOT typically associated with tension pneumothorax?
Which of the following findings is NOT typically associated with tension pneumothorax?
When should pleural decompression be performed in a patient suspected of tension pneumothorax?
When should pleural decompression be performed in a patient suspected of tension pneumothorax?
What is one of the critical assessment findings of an open pneumothorax?
What is one of the critical assessment findings of an open pneumothorax?
In the management of an open pneumothorax, which step is crucial to ensure proper airway and ventilation?
In the management of an open pneumothorax, which step is crucial to ensure proper airway and ventilation?
How does tension pneumothorax primarily occur?
How does tension pneumothorax primarily occur?
What is a common complication that can arise if a tension pneumothorax is not treated immediately?
What is a common complication that can arise if a tension pneumothorax is not treated immediately?
Which of the following symptoms is directly associated with a tension pneumothorax?
Which of the following symptoms is directly associated with a tension pneumothorax?
What should be monitored during the management of a patient with an open pneumothorax?
What should be monitored during the management of a patient with an open pneumothorax?
Which injury mechanism is associated with tension pneumothorax?
Which injury mechanism is associated with tension pneumothorax?
Why is it vital to apply an occlusive dressing in the management of an open pneumothorax?
Why is it vital to apply an occlusive dressing in the management of an open pneumothorax?
What does the presence of tachycardia indicate in a patient with an open pneumothorax?
What does the presence of tachycardia indicate in a patient with an open pneumothorax?
What should be established before positive-pressure ventilation in managing open pneumothorax?
What should be established before positive-pressure ventilation in managing open pneumothorax?
What is a common cause of pneumothorax related to rib fractures?
What is a common cause of pneumothorax related to rib fractures?
What is the management strategy for circulation in cases where pulmonary contusion is suspected?
What is the management strategy for circulation in cases where pulmonary contusion is suspected?
What physiological mechanism primarily causes a closed pneumothorax?
What physiological mechanism primarily causes a closed pneumothorax?
Which of the following is NOT a part of the management for sternal fractures?
Which of the following is NOT a part of the management for sternal fractures?
In adult blunt chest trauma, the incidence of closed pneumothorax is approximately:
In adult blunt chest trauma, the incidence of closed pneumothorax is approximately:
What should be monitored if a patient exhibits signs of pneumothorax?
What should be monitored if a patient exhibits signs of pneumothorax?
What is the expected outcome for small tears in the lung associated with pneumothorax?
What is the expected outcome for small tears in the lung associated with pneumothorax?
What is the primary effect of the 'paper-bag effect' during a closed pneumothorax scenario?
What is the primary effect of the 'paper-bag effect' during a closed pneumothorax scenario?
Which strategy is crucial for psychological support during the management of thoracic injuries?
Which strategy is crucial for psychological support during the management of thoracic injuries?
What respiratory complication can result from a closed pneumothorax?
What respiratory complication can result from a closed pneumothorax?
Flashcards
Thoracic Trauma Deaths
Thoracic Trauma Deaths
More than 20% of traumatic deaths are due to chest injuries.
Blunt Thoracic Injury
Blunt Thoracic Injury
Chest injury from forces distributed over a large area, including deceleration and compression.
Penetrating Thoracic Injury
Penetrating Thoracic Injury
Chest injury from forces concentrated on a small area, often harming organs along the object's path.
Chest Injury Management
Chest Injury Management
Signup and view all the flashcards
Leading Cause of Trauma Deaths
Leading Cause of Trauma Deaths
Signup and view all the flashcards
Types of Thoracic Injuries
Types of Thoracic Injuries
Signup and view all the flashcards
Mechanism of injury
Mechanism of injury
Signup and view all the flashcards
Open injuries
Open injuries
Signup and view all the flashcards
Closed injuries
Closed injuries
Signup and view all the flashcards
Cardiovascular injuries
Cardiovascular injuries
Signup and view all the flashcards
Clavicle Fracture
Clavicle Fracture
Signup and view all the flashcards
Rib Fractures
Rib Fractures
Signup and view all the flashcards
Tachypnea
Tachypnea
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Respiration
Respiration
Signup and view all the flashcards
Assessment findings
Assessment findings
Signup and view all the flashcards
Pneumothorax
Pneumothorax
Signup and view all the flashcards
Closed pneumothorax
Closed pneumothorax
Signup and view all the flashcards
Blunt chest trauma
Blunt chest trauma
Signup and view all the flashcards
Penetrating chest trauma
Penetrating chest trauma
Signup and view all the flashcards
High-concentration oxygen
High-concentration oxygen
Signup and view all the flashcards
Fractured rib
Fractured rib
Signup and view all the flashcards
Pulmonary contusion
Pulmonary contusion
Signup and view all the flashcards
Ventilation/perfusion mismatch
Ventilation/perfusion mismatch
Signup and view all the flashcards
Airway and Ventilation
Airway and Ventilation
Signup and view all the flashcards
Intra-abdominal injuries
Intra-abdominal injuries
Signup and view all the flashcards
Open Pneumothorax
Open Pneumothorax
Signup and view all the flashcards
Occlude the wound
Occlude the wound
Signup and view all the flashcards
Tension Pneumothorax
Tension Pneumothorax
Signup and view all the flashcards
Mediastinal shift
Mediastinal shift
Signup and view all the flashcards
Positive-pressure ventilation
Positive-pressure ventilation
Signup and view all the flashcards
Ventilatory dysfunction
Ventilatory dysfunction
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Associated injuries
Associated injuries
Signup and view all the flashcards
Respiratory distress
Respiratory distress
Signup and view all the flashcards
Tension Pneumothorax Signs
Tension Pneumothorax Signs
Signup and view all the flashcards
Tension Pneumothorax Management
Tension Pneumothorax Management
Signup and view all the flashcards
Tension Pneumothorax vs. Pneumothorax
Tension Pneumothorax vs. Pneumothorax
Signup and view all the flashcards
Needle Thoracostomy
Needle Thoracostomy
Signup and view all the flashcards
Study Notes
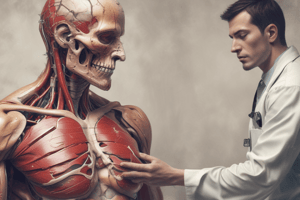
Thoracic Trauma
- Thoracic trauma is responsible for over 20% of all traumatic deaths, regardless of mechanism.
- Approximately 16,000 deaths occur annually in the United States due to chest injuries.
- Chest injuries are the second leading cause of trauma deaths each year.
- Most thoracic injuries (90% of blunt and 70-85% of penetrating trauma) are manageable without surgery.
Classifications of Chest Injuries
- Skeletal injury: Damage to bones of the chest.
- Pulmonary injury: Damage to the lungs (e.g., collapsed lung).
- Heart and great vessel injury: Damage to the heart or major blood vessels.
- Diaphragmatic injury: Damage to the diaphragm.
Mechanism of Injury
- Blunt thoracic injuries: Forces distributed over a large area, including deceleration and compression.
- Penetrating thoracic injuries: Forces concentrated over a small area, along the path of the penetrating object.
Injury patterns
- Open injuries: Injuries with a break in the skin.
- Closed injuries: Injuries without a break in the skin.
Injury Patterns-Specific Types
- Cardiovascular
- Pleural and pulmonary
- Mediastinal
- Diaphragmatic
- Esophageal
- Penetrating cardiac trauma
- Blast injury
- Confined spaces
- Shock wave
- Thoracic cage
Thoracic Anatomy
- Skin, muscles
- Respiratory muscles: (phrenic and intercostal nerves)
- Bones: Thoracic cage, sternum, thoracic spine
- Trachea
- Bronchi
- Lungs
Vascular Anatomy
- Heart: Ventricles, atria, valves and pericardium.
- Arteries: Aorta, carotid, subclavian, intercostal
- Veins: Superior vena cava, inferior vena cava, subclavian, internal jugular
- Pulmonary: Arteries & Veins
Mediastinum
- The area between the lungs
- Contains the heart, trachea, venae cavae, pulmonary arteries, aorta, esophagus, and lymph nodes.
Thoracic Physiology
- Ventilation: Mechanical process of moving air into and out of the lungs.
- Respiration: Exchange of oxygen and carbon dioxide between the outside atmosphere and the body's cells.
Pathophysiology of Thoracic Trauma-Cardiac Output
- Impairments in cardiac output: Blood loss, increased intrapleural pressures, blood in the pericardial sac, myocardial valve damage, or vascular disruption.
Pathophysiology of Thoracic Trauma-Gas Exchange
- Impairments in gas exchange: Atelectasis, contused lung tissue, disruption of the respiratory tract.
Assessment Findings - Pulse
- Pulse deficit: Reduced pulse strength
- Tachycardia: Increased heart rate
- Bradycardia: Decreased heart rate
Assessment Findings - Blood Pressure
- Narrowed pulse pressure: Reduced difference between systolic and diastolic pressures
- Hypertension: Elevated blood pressure
- Hypotension: Low blood pressure
- Pulsus paradoxus: Decrease in systolic blood pressure during inspiration
Assessment Findings - Respiratory Rate
- Tachypnea: Increased respiratory rate
- Bradypnea: Decreased respiratory rate
- Labored breathing: Increased respiratory effort
- Retractions: Visible inward movement of the chest during breathing
- Other respiratory distress: Additional signs of respiratory difficulty
Assessment Findings - Skin
- Diaphoresis: Excessive sweating
- Pallor: Paleness
- Cyanosis: Bluish discoloration of the skin
- Open wounds: Visible breaks in the skin
- Ecchymosis: Bruising
- Other evidence of trauma: Additional signs of injury
Assessment Findings - Neck
- Trachea position: Check for displacement.
- Subcutaneous emphysema: Presence of air in the tissues under the skin.
- Jugular venous distension: Swelling in the neck veins
- Penetrating wounds: Open injuries to the neck.
Assessment Findings - Chest
- Contusions: Bruises on chest wall
- Tenderness: Pain when touched
- Asymmetry: Unequal sides
- Lung sounds: Check for presence, quality, and location of breath sounds.
- Absent or decreased breath sounds: Reduced or missing breath sounds.
- Bilateral breath sounds: Normal breath sounds on both sides.
- Bowel sounds in hemothorax: Unusual bowel sounds in the chest cavity.
- Abnormal percussion findings: Checking for unusual sounds/qualities. (e.g. hyperresonance-air, hyporesonance-fluid)
Assessment Findings - ECG
- ST/T wave elevation or depression
- Conduction disturbances
- Rhythm disturbances
History
- Dyspnea
- Chest pain
- Associated symptoms
- Symptoms before incident
- Past cardiac/respiratory disease
- Motor vehicle crash restraint use
Thoracic Trauma Treatment-Airway and Ventilation
- High-concentration oxygen.
- Positive-pressure ventilation.
- Endotracheal intubation
- Needle cricothyrotomy
- Surgical cricothyrotomy
- Pleural decompression
- Occlude open wounds
- Stabilize chest wall
Thoracic Trauma Treatment-Circulation
- Manage cardiac dysrhythmias.
- Intravenous access
- Supportive Measures
Thoracic Trauma Treatment-Pharmacological and Nonpharmacological
- Analgesics
- Antidysrhythmics
- Stabilize chest wall
- Needle thoracostomy
- Tube thoracostomy (in-hospital management)
- Pericardiocentesis (in-hospital management)
Clavicular Fractures
- Common causes: Falling, contact sports.
- Signs and symptoms: Pain, point tenderness, deformity
- Treatment: Sling and swathe or strap immobilisation
- Complications: Injury to subclavian vein/artery, hematoma, or venous thrombosis.
Rib Fractures
- Incidence: Less common in adults, more often in elderly. Significant force needed to fracture ribs.
- Common reasons: Fall, impact trauma to the chest.
- Pathophysiology: Blunt trauma - bowing. Respiratory restriction from pain and splinting. Intercostal nerve/vascular damage important. Associated complications include rupture of the aorta, tracheal/bronchial tree injury or vascular trauma.
- Morbidity/Mortality: Can lead to associated pulmonary or cardiovascular injury if severe or multiple fractures.
- Management: Airway and ventilation (high oxygen, positive pressure ventilation). Encourage coughing. Pharmacological: Analgesics. Nonpharmacological: Splinting.
Multiple Rib Fractures-Assessment Findings
- Localized pain
- Pain aggravated by movement, breathing, coughing
- Point tenderness
- Pointing to affected area on chest (palpated)
- Crepitus/audible crunch
- Splinting during respiration
Multiple Rib Fractures-Causes of Complications
- Atelectasis: Blockage from trauma, reduced breathing causing part of lungs to collapse
- Hypoventilation: Inadequate breathing/lower airflow
- Inadequate cough: Reduced capacity to cough/remove secretions
- Pneumonia: Infection of the lung tissue
Rib Fractures - Management
- Airway and ventilation: high concentration oxygen and positive pressure ventilation may be necessary
- Encourage coughing and deep breathing
- Pharmacological: analgesics; avoid broad spectrum antibiotics in this scenario.
- Nonpharmacological: Splinting
- Consider transport mode, facility
Flail Chest
- Incidence: Multiple rib fractures that result in a free-floating chest wall segment. High-speed impacts common cause.
- Most common causes: vehicular crashes; falls from heights; industrial accidents; or assault. Birth trauma is less frequent.
- Morbidity/Mortality: 20% to 40% of associated injuries can result in death if in an advanced age with or when other significant and severe injuries are present. Mortality increased with advanced age, seven or more fractured ribs, three or more associated injuries, shock, or head injury or brain damage.
- Pathophysiology: Two or more adjacent ribs fractured in two or more places. Direct impact typically causes the fracture. Disruption will result in reduced lung function as a result of respiratory inadequacy. Intra-thoracic, internal thoracic injury typically causes compression of the uninjured lung.
- Assessment Findings: Pleuritic chest pain; pain/splinting on affected side; tachypnea; respiratory distress; chest wall contusion; paradoxical chest wall movement; crepitus (cracking/grating sound when palpating and breathing); tachycardia; possible bundle branch block on ECG.
- Management: Airway and ventilation (high-concentration oxygen and positive-pressure ventilation may be necessary to reverse the paradoxical chest wall movement, restore tidal volume, and assist breathing if necessary); Monitor closely for pneumothorax, and possible intubation if needed.
Sternal Fractures
- Incidence: 5-8% of blunt chest trauma patients. High-force trauma typically involved in causing this.
- Common causes: Deceleration injuries, steering wheel, dashboard impacts; direct blows, massive crush injuries; and severe hyperflexion of the thoracic cage.
- Morbidity/Mortality: High association with associated myocardial or lung injury, may be substantial. 25-45% mortality risk dependent on degree of injury.
- Pathophysiology: Associated injuries including pulmonary and myocardial contusion; flail chest.
- Management: Airway and ventilation (high concentration oxygen and positive pressure ventilation may be needed). Circulation (restrict fluids if pulmonary contusion suspected). Nonpharmacologic (allowing chest wall splinting).
Pulmonary Injury (Pneumothorax)
- Incidence: 10-30% in blunt chest trauma; almost 100% in penetrating chest trauma
- Pathophysiology: Air enters pleural space (between lung and chest wall), resulting in collapse or reduced lung expansion (often caused by fractured rib).
- Assessment Findings: Tachypnea, respiratory distress, absent or decreased breath sounds on the affected side, hyperresonance, decreased chest wall movement, dyspnea, chest pain(referred), slight pleuritic chest pain.
- Closed pneumothorax: May occur in absences of rib fractures, result of sudden increase in intrathoracic pressure, (e.g., "paper bag effect"); small tear self-seal but larger may progress), trachea shifted towards affected side
- Open pneumothorax: Usually a penetrating injury to the chest wall. Air can enter/leave pleural space.
- Management: (Closed) Airway/ventilation, high concentration oxygen; (Closed):positive-pressure ventilation if respiration rate is <12 or > 28 breaths per minute; Ventilation assistance(bag-valve mask if needed); Non-pharmacological: Needle thoracostomy. If possible, transport in the position of comfort. Transport considerations mode/facility
- Morbidity/Mortality: Severity directly related to wound size and potentially life-threatening if hypoventilation results in hypoxemia.
Tension Pneumothorax
- Associated Injuries: Penetrating injury to chest, blunt trauma; penetration from a fractured rib. Many other causes.
- Morbidity/Mortality: Life-threatening. Associated with profound hypoventilation, immediate threatening chest injury. Death related to delayed management if emergency intervention is delayed.
- Pathophysiology: Air leaks into the interpleural space (between lung and chest wall), increasing pressure in the chest. This compression can shift the mediastinum and impair cardiac output.
- Assessment Findings: Extreme anxiety, cyanosis, diminished/absent breath sounds on affected side, tracheal deviation, tachycardia, hypotension, increasing dyspnea; difficult ventilation while being assisted; unequal chest expansion; bulging intercostal muscles, subcutaneous emphysema; jugular distension, hyperresonance percussions.
- Management: Emergency care to reduce pressure in the pleural space. High-concentration oxygen. Potential need for positive pressure ventilation. May need intubation. Perform needle thoracostomy. Monitor for and treat/address life-threatening complications.
Hemothorax
- Incidence: Associated with pneumothorax (hemopneumothorax). Typically caused by blunt or penetrating trauma, often rib fractures.
- Morbidity/Mortality: Life threatening injury requiring urgent chest tube placement or surgery. 50% mortality if immediate (or with minimal) treatment is unavailable.
- Pathophysiology: Blood accumulates in pleural space between lung and chest wall. Compromises cardiovascular function, reduces lung function, decreases blood pressure. Hypovolemia results as blood accumulates in the pleural space.
- Assessment Findings: Tachypnea, dyspnea, cyanosis (typically not evident in shock); diminished or decreased breath sounds on the affected side, hyporesonance on affected side, hypotension, narrowed pulse pressure; tracheal deviation to unaffected side, pale, cool, moist skin.
- Management: Airway and ventilation, high-concentration oxygen/positive pressure ventilation if necessary; circulation (volume expansion, correcting hypovolemia); pharmacologic/non-pharmacologic (tube thoracostomy for managing/treating/removing blood, blood transfusions).
Hemopneumothorax
- Pathophysiology: Combination of pneumothorax and hemothorax.
- Assessment: Assessment/findings & management is the same as for hemothorax.
- Management: Management is the same as for Hemothorax.
Pulmonary Contusion
- Incidence: High incidence of blunt chest trauma (30-75% of blunt trauma patients have this). Commonly associated with rib fractures.
- Morbidity/Mortality: Potentially lethal; may be missed due to high incidence of associated injuries. Mortality: 14-20%.
- Pathophysiology: Blunt trauma to the chest can damage lung tissue resulting in bruising and leakage of blood inside the lung tissue that can affect gas exchange.
- Assessment Findings: Tachypnea, tachycardia, respiratory distress, dyspnea, cough, hemoptysis, evidence of blunt chest trauma, apprehension, cyanosis.
- Management: Airway and ventilation (high-concentration oxygen; may consider positive pressure ventilation). Circulation (restricting IV fluids if patient not low/hypovolemic).
Traumatic Asphyxia
- Incidence: Caused by a severe crushing injury to the chest (and abdomen). Causes include steering wheel injuries, conveyor belt/strap injury or a severe compression injury by a heavy object of some type.
- Pathophysiology: Results from a sudden increase in intrathoracic pressure. This pressure increase pushes blood from the right side of the heart into the veins of the upper thorax, neck, & face. The result is jugular vein engorgement and capillary rupture.
- Assessment Findings: Reddish/purple discoloration of the face and neck, (skin below the face and neck will remain pink). Jugular distension, swelling of the lips/tongue, head/neck, or hemorrhage of the conjunctiva. (subconjunctival petechiae may appear). When pressure is released hypotension may be present.
- Management: Airway and ventilation-ensure an open airway, provide adequate ventilation; circulation-IV access, expect hypotension & shock release of compression; Transport-Appropriate mode/facility.
Heart and Great Vessel Injury
- Incidence: Myocardial contusion is the most common cardiac injury after blunt chest trauma. (16-76% of patients with blunt trauma). Often a result of motor-vehicle collisions. Sternal and multiple rib fractures common.
- Morbidity/Mortality: Significant cause of morbidity and mortality in blunt trauma patients. Subclinical in assessment.
- Pathophysiology: Blunt force to the chest, often resulting from motor vehicle collisions or high deceleration impacts that result in an internal thoracic injury or heart/vessels injury that is easily overlooked.
- Assessment Findings: Retrosternal chest pain, ECG changes (persistent tachycardia, ST elevation/T wave inversion, right bundle branch block, atrial flutter/fibrillation, premature ventricular/atrial contractions). New cardiac murmurs, pericardial friction rub (late). Hypotension; chest wall contusion/ecchymosis.
- Management: Airway and ventilation-high concentration oxygen/possible positive pressure ventilation if necessary. Circulation-IV access and possible consideration/administration of anti-dysrhythmics/vasopressors if life threatening. Transport considerations-Appropriate mode/facility.
Pericardial Tamponade
- Incidence: Rare, less than 2% of all chest traumas. Rare in blunt trauma, more frequent in penetrating trauma/wounds.
- Morbidity/Mortality: Gunshot wounds have higher mortality. Lower mortality if isolated tamponade.
- Pathophysiology: Fluid (typically blood) accumulates in the pericardial sac, which compresses the heart resulting in decreased cardiac output.
- Assessment Findings: Tachycardia, respiratory distress, narrowed pulse pressure (with hypotension); cyanosis of head, neck, & extremities; Beck's triad (narrowing pulse pressure, neck-vein distension, muffled heart sounds), Kussmaul's sign (rise in venous pressure with inspiration).
- Management: Airway and ventilation; circulation (IV fluid challenge/treatment for shock/dehydration and hypotension). Non-pharmacological, pericardiocentesis; Transport considerations-Appropriate mode/facility; Psychological support.
Traumatic Aortic Rupture
- Incidence: 15% of all blunt trauma deaths. Trauma results from high speed impacts (e.g., motor vehicle collision), falls from significant heights, crushing injuries.
- Morbidity/Mortality: Significant cause of morbidity and mortality. 80-90% die at accident scene; 10-20% surviving the immediate hour. Often not obvious during initial assessment but high mortality due to associated injuries.
- Pathophysiology: Blunt force to the chest. Bleeding can be quickly tamponaded by the surrounding tissue.
- Assessment Findings: Upper extremity hypertension with decreased/absent femoral pulses; generalized hypertension secondary to increased sympathetic discharge; harsh systolic murmur over the pericardium or interscapular/chest wall area; paraplegia with a normal cervical/thoracic spine (rare); retrosternal or interscapular pain; dyspnea and dysphagia; and ischemic pain of extremities.
- Management: Airway and ventilation (high-concentration oxygen; ventilatory support with spinal precautions). Circulation (limited fluid replacement for normotensive patients; prevent increased pressure in remaining aortic wall tissue). Transport considerations-Appropriate mode/facility/communication.
Diaphragmatic Rupture
- Incidence: 1%- 8% of all blunt injuries. 90% of injuries are associated with high speed motor vehicle crashes.
- Pathophysiology: Blunt or penetrating trauma typically breaks the diaphragm. Intra-abdominal organs may move into the thoracic cavity, placing pressure on the lung resulting in poor venous return. Reduced venous/cardiac output/lung function. These are signs of severe/significant injury.
- Assessment Findings: Tachypnea, tachycardia, respiratory distress; dullness to percussion; bowel sounds in the affected hemithorax(abnormal); scaphoid abdomen (hollow or empty appearance); decreased breath sounds on the affected side; possible chest or abdominal pain.
- Management: Airway and ventilation (high-concentration oxygen; positive-pressure ventilation if necessary, caution as positive pressure can worsen the injury); Circulation (IV access); Non-pharmacological (avoiding Trendelenburg positioning. Transport, etc).
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.