Podcast
Questions and Answers
What percentage of thoracic outlet syndrome (TOS) cases is related to vascular compression?
What percentage of thoracic outlet syndrome (TOS) cases is related to vascular compression?
- 10-15%
- 20-25%
- 3-5% (correct)
- 1-2%
Which of the following is the most commonly compressed neural structure in TOS?
Which of the following is the most commonly compressed neural structure in TOS?
- Lowest trunk of the brachial plexus (correct)
- Subclavian nerve
- Thoracic nerves
- Cervical nerves
What factor contributes to a higher prevalence of TOS in women compared to men?
What factor contributes to a higher prevalence of TOS in women compared to men?
- Higher physical activity levels
- Greater muscle mass
- Narrowed thoracic outlet (correct)
- Older mean age
Which type of thoracic outlet syndrome is characterized by true neurological deficits?
Which type of thoracic outlet syndrome is characterized by true neurological deficits?
What anatomical variation is responsible for most neural compression in TOS?
What anatomical variation is responsible for most neural compression in TOS?
What is the mean age range of individuals affected by thoracic outlet syndrome?
What is the mean age range of individuals affected by thoracic outlet syndrome?
Which structure is least likely to be affected in cases of thoracic outlet syndrome?
Which structure is least likely to be affected in cases of thoracic outlet syndrome?
Which of the following descriptions applies to Symptomatic TOS (sTOS)?
Which of the following descriptions applies to Symptomatic TOS (sTOS)?
What posture is commonly exhibited by individuals with thoracic outlet syndrome (TOS)?
What posture is commonly exhibited by individuals with thoracic outlet syndrome (TOS)?
Which muscle group is primarily affected when the scalenes tighten in relation to thoracic outlet syndrome?
Which muscle group is primarily affected when the scalenes tighten in relation to thoracic outlet syndrome?
What is a consequence of poor diaphragmatic usage according to the provided content?
What is a consequence of poor diaphragmatic usage according to the provided content?
What effect does a tight pectoralis minor muscle have on shoulder mechanics?
What effect does a tight pectoralis minor muscle have on shoulder mechanics?
Which of the following statements is NOT true regarding scapular stability in the context of TOS?
Which of the following statements is NOT true regarding scapular stability in the context of TOS?
What is the role of the sternocleidomastoid in relation to TOS?
What is the role of the sternocleidomastoid in relation to TOS?
Which condition can further constrict the costoclavicular space in individuals with TOS?
Which condition can further constrict the costoclavicular space in individuals with TOS?
What type of work activity is most likely to lead to a decrease in the costoclavicular space?
What type of work activity is most likely to lead to a decrease in the costoclavicular space?
What is the recommended range of active knee flexion by the 7th postoperative day?
What is the recommended range of active knee flexion by the 7th postoperative day?
What is the initial flexion range controlled by the CPM machine during the first 24 hours post-surgery?
What is the initial flexion range controlled by the CPM machine during the first 24 hours post-surgery?
Which of the following is a correct statement regarding the disadvantages of using a CPM machine?
Which of the following is a correct statement regarding the disadvantages of using a CPM machine?
What should be done if a patient has not reached the desired knee flexion by day 7?
What should be done if a patient has not reached the desired knee flexion by day 7?
Which intervention is indicated if there is an extensor lag during CPM usage?
Which intervention is indicated if there is an extensor lag during CPM usage?
What is the expected knee flexion attainment by day 14 with the use of CPM?
What is the expected knee flexion attainment by day 14 with the use of CPM?
What is indicated when a CPM machine is not available and extensor lag occurs?
What is indicated when a CPM machine is not available and extensor lag occurs?
When can unsupported weight bearing typically begin for a patient post-surgery?
When can unsupported weight bearing typically begin for a patient post-surgery?
What is the primary purpose of knee arthroplasty?
What is the primary purpose of knee arthroplasty?
Which of the following is NOT considered a contraindication for knee arthroplasty?
Which of the following is NOT considered a contraindication for knee arthroplasty?
What is the primary focus of a bi-compartmental knee replacement?
What is the primary focus of a bi-compartmental knee replacement?
What type of surgical approach is suggested for larger-chested women to relieve thoracic outlet syndrome symptoms?
What type of surgical approach is suggested for larger-chested women to relieve thoracic outlet syndrome symptoms?
Which exercise should be practiced during the preoperative rehabilitation phase?
Which exercise should be practiced during the preoperative rehabilitation phase?
What does postoperative rehabilitation after knee arthroplasty focus on in the initial stages?
What does postoperative rehabilitation after knee arthroplasty focus on in the initial stages?
Which type of fixation is NOT a classification used for knee arthroplasty?
Which type of fixation is NOT a classification used for knee arthroplasty?
What action should be taken on the first day post-operation to minimize pressure sores?
What action should be taken on the first day post-operation to minimize pressure sores?
What is the rationale for performing quadriceps sets hourly during the early postoperative stage?
What is the rationale for performing quadriceps sets hourly during the early postoperative stage?
How long should overhead activities and lifting be avoided after knee arthroplasty?
How long should overhead activities and lifting be avoided after knee arthroplasty?
Which symptoms are specifically associated with upper plexus involvement in neurogenic thoracic outlet syndrome?
Which symptoms are specifically associated with upper plexus involvement in neurogenic thoracic outlet syndrome?
What determines the initial position of the knee in patients who do not use a CPM machine post-surgery?
What determines the initial position of the knee in patients who do not use a CPM machine post-surgery?
Which of these classifications pertains to knee arthroplasty based on the portion of the knee being replaced?
Which of these classifications pertains to knee arthroplasty based on the portion of the knee being replaced?
What distinguishes compressors from releasers in thoracic outlet syndrome?
What distinguishes compressors from releasers in thoracic outlet syndrome?
What is a primary symptom that may be alleviated by using the Cyriax release maneuver for thoracic outlet syndrome?
What is a primary symptom that may be alleviated by using the Cyriax release maneuver for thoracic outlet syndrome?
Which activity is allowed from Day 2 after surgery if there is no CPM machine used?
Which activity is allowed from Day 2 after surgery if there is no CPM machine used?
What are ankle pumps intended to achieve during the early postoperative stage?
What are ankle pumps intended to achieve during the early postoperative stage?
Which symptom is commonly observed in patients experiencing venous thoracic outlet syndrome?
Which symptom is commonly observed in patients experiencing venous thoracic outlet syndrome?
What does a uni-compartmental knee replacement aim to replace?
What does a uni-compartmental knee replacement aim to replace?
What is a key symptom of arterial thoracic outlet syndrome?
What is a key symptom of arterial thoracic outlet syndrome?
Which symptom is indicative of true thoracic outlet syndrome?
Which symptom is indicative of true thoracic outlet syndrome?
In which situation would a patient likely be classified as experiencing releasers symptoms?
In which situation would a patient likely be classified as experiencing releasers symptoms?
Which of the following signs is indicative of lower plexus involvement in thoracic outlet syndrome?
Which of the following signs is indicative of lower plexus involvement in thoracic outlet syndrome?
What is a distinguishing feature of disputed neurogenic thoracic outlet syndrome?
What is a distinguishing feature of disputed neurogenic thoracic outlet syndrome?
Flashcards
Neurological Thoracic Outlet Syndrome (nTOS)
Neurological Thoracic Outlet Syndrome (nTOS)
The most common type of TOS, affecting the nerves of the brachial plexus. This type is further divided into true and disputed neurological TOS.
Vascular Thoracic Outlet Syndrome (vTOS)
Vascular Thoracic Outlet Syndrome (vTOS)
A rarer form of TOS where blood vessels are compressed, mainly affecting the subclavian artery or vein.
True Neurological TOS (tTOS)
True Neurological TOS (tTOS)
A condition where neurological deficits, like muscle weakness or atrophy, are present due to brachial plexus compression.
Disputed / non-specific / Symptomatic TOS (sTOS)
Disputed / non-specific / Symptomatic TOS (sTOS)
Signup and view all the flashcards
Brachial Plexus Compression
Brachial Plexus Compression
Signup and view all the flashcards
Cervical Rib
Cervical Rib
Signup and view all the flashcards
Interscalene Triangle
Interscalene Triangle
Signup and view all the flashcards
Costoclavicular Space
Costoclavicular Space
Signup and view all the flashcards
Fibrous Bands in TOS
Fibrous Bands in TOS
Signup and view all the flashcards
Posture and TOS
Posture and TOS
Signup and view all the flashcards
Muscle Imbalance in TOS
Muscle Imbalance in TOS
Signup and view all the flashcards
Scalene Muscle and TOS
Scalene Muscle and TOS
Signup and view all the flashcards
Pectoralis Minor Muscle and TOS
Pectoralis Minor Muscle and TOS
Signup and view all the flashcards
Weak Scapular Muscles and TOS
Weak Scapular Muscles and TOS
Signup and view all the flashcards
Pelvic Muscle Imbalance and TOS
Pelvic Muscle Imbalance and TOS
Signup and view all the flashcards
Cervical Rib and TOS
Cervical Rib and TOS
Signup and view all the flashcards
What are the symptoms of neurogenic thoracic outlet syndrome?
What are the symptoms of neurogenic thoracic outlet syndrome?
Signup and view all the flashcards
Where does the pain typically radiate when the upper brachial plexus is involved?
Where does the pain typically radiate when the upper brachial plexus is involved?
Signup and view all the flashcards
Where does the pain typically radiate when the lower brachial plexus is involved?
Where does the pain typically radiate when the lower brachial plexus is involved?
Signup and view all the flashcards
What are the characteristics of 'True' Neurological TOS?
What are the characteristics of 'True' Neurological TOS?
Signup and view all the flashcards
What are the characteristics of 'Disputed' Neurological TOS?
What are the characteristics of 'Disputed' Neurological TOS?
Signup and view all the flashcards
Who are considered 'Compressors' in TOS?
Who are considered 'Compressors' in TOS?
Signup and view all the flashcards
Who are considered 'Releasers' in TOS?
Who are considered 'Releasers' in TOS?
Signup and view all the flashcards
What are the symptoms of venous thoracic outlet syndrome?
What are the symptoms of venous thoracic outlet syndrome?
Signup and view all the flashcards
Knee Arthroplasty
Knee Arthroplasty
Signup and view all the flashcards
Uni-compartmental Knee Arthroplasty
Uni-compartmental Knee Arthroplasty
Signup and view all the flashcards
Bi-compartmental Knee Arthroplasty
Bi-compartmental Knee Arthroplasty
Signup and view all the flashcards
Tri-compartmental Knee Arthroplasty
Tri-compartmental Knee Arthroplasty
Signup and view all the flashcards
Un-constrained Knee Arthroplasty
Un-constrained Knee Arthroplasty
Signup and view all the flashcards
Semi-constrained Knee Arthroplasty
Semi-constrained Knee Arthroplasty
Signup and view all the flashcards
Fully-constrained Knee Arthroplasty
Fully-constrained Knee Arthroplasty
Signup and view all the flashcards
Cemented Knee Arthroplasty
Cemented Knee Arthroplasty
Signup and view all the flashcards
Cementless Knee Arthroplasty
Cementless Knee Arthroplasty
Signup and view all the flashcards
Bi-compartmental Knee Replacement
Bi-compartmental Knee Replacement
Signup and view all the flashcards
Tri-compartmental Knee Replacement
Tri-compartmental Knee Replacement
Signup and view all the flashcards
Uni-compartmental Knee Replacement
Uni-compartmental Knee Replacement
Signup and view all the flashcards
Isometric Quadriceps Exercises
Isometric Quadriceps Exercises
Signup and view all the flashcards
Ankle Pumps
Ankle Pumps
Signup and view all the flashcards
Gluteal Sets
Gluteal Sets
Signup and view all the flashcards
Upper Extremity Exercises
Upper Extremity Exercises
Signup and view all the flashcards
Straight Leg Raise (SLR)
Straight Leg Raise (SLR)
Signup and view all the flashcards
Extensor Lag
Extensor Lag
Signup and view all the flashcards
CPM
CPM
Signup and view all the flashcards
How long is the CPM machine used for?
How long is the CPM machine used for?
Signup and view all the flashcards
Manipulation under Anesthesia
Manipulation under Anesthesia
Signup and view all the flashcards
Fixed Flexion Deformity
Fixed Flexion Deformity
Signup and view all the flashcards
Quadriceps Lag
Quadriceps Lag
Signup and view all the flashcards
Water Therapy
Water Therapy
Signup and view all the flashcards
Active Assisted Knee Flexion
Active Assisted Knee Flexion
Signup and view all the flashcards
Study Notes
Achilles Tendinopathy/Tendinosis/Tendinopathy
- Refers to a combination of pathological changes affecting the Achilles tendon, usually due to overuse and chronic stress.
- Can occur in athletes and non-athletes.
- May or may not be associated with an Achilles tendon tear.
- Lack of flexibility or a stiff Achilles tendon increases the risk of injury.
- The thickest and strongest tendon in the body.
- Originates from the gastrocnemius and soleus muscles, inserting on the calcaneal tuberosity.
- Approximately 15 cm (6 inches) long.
- Experiences stress of 3.9 times body weight during walking and 7.7 times body weight during running.
- Surrounded by a paratenon (connective tissue sheath) instead of a synovial sheath.
- Paratenon provides the major blood supply to the tendon.
- Blood supply comes distally from intraosseous vessels (calcaneus) and proximally from intramuscular branches.
- A relative avascular zone exists 2-6 cm from the calcaneal insertion, making it vulnerable to degeneration and injury.
- Blood supply is evident at the muscle-tendon junction and tendon-bone insertion.
- Vascular density is greatest proximally and least in the midportion of the tendon.
- Tendon injuries are commonly associated with repetitive impact loading from running and jumping.
- Either the tendon or paratenon (or both) can become inflamed, resulting in tendonitis or peritendinitis.
- Tendinopathy is a common overuse injury caused by repetitive energy storage and release with excessive compression. This can lead to a sudden injury or a rupture.
- Commonly called Achilles tendonitis, but more accurately described as tendinosis (not inflammation).
- Classified into insertional (within 2 cm of insertion) and mid-substance/noninsertional (2-6 cm proximal to insertion).
Causes of Achilles Tendonitis
- Overuse injury with forces within the physiological range, but repeated with poor recovery time, causing fatigue and increasing susceptibility to micro-tearing.
- Sudden loading of excessive force, especially with eccentric motion, causing damage.
- Insufficient flexibility in the gastrocnemius and soleus muscles, increasing strain on the tendon and causing micro-tears.
- Muscle weakness in the gastrocnemius and soleus which results in micro-tears and inflammation of the Achilles tendon.
- Joint restrictions (e.g., pes cavus) in the talocrural or subtalar joints decrease shock absorption and adaptability to uneven terrain.
- Excessive pronation leads to internal tibial rotation, drawing the Achilles tendon medially (whipping action) and contributing to overuse degeneration and inflammation or small tears, particularly in the medial aspect.
- Systemic diseases such as diabetes, lupus, and gout are associated with tendon weakness.
- Corticosteroid injections can cause tendon rupture and are controversial.
- Poor footwear (too small, worn-out, poor heel counter) reduces rear foot stability and shock absorption.
- Running on unyielding or uneven surfaces.
Physical Examination and Findings
- Morning pain is a hallmark symptom.
- Diffuse pain in or around the back of the ankle and heel, aggravated by activity (especially uphill running or stair climbing).
- Pain is relieved somewhat by wearing higher-heeled shoes or boots.
- Recent increase in activity levels or changes in footwear is often reported by patients.
- Observable, palpable edema and thickening of the Achilles tendon (A-P and M-L).
- Painful and prominent lumps or nodules within the tendon.
- Crepitus during plantar and dorsiflexion, detected through arc sign.
Diagnosis
- Diagnosis uses history, symptom behavior, clinical tests, ultrasound (for tendons, water content, collagen integrity and bursal swelling), X-rays (for bone changes, calcification), and MRI (for surgery planning).
- X-rays visualize calcification in the tendon (insertional) or midportion (severe noninsertional) tendinopathy.
Differential Diagnosis
- Plantar fasciitis
- Calcaneal fracture stress
- Heel pad syndrome
- Haglund deformity
- Sever's disease
- Posterior Ankle Impingement
- Medial Tendinopathy
- Retrocalcaneal Bursitis
- Sural Nerve
- Lumbar Radiculopathy
- Ankle OA
- Deep vein thrombosis
- Partial Achilles Tendon Rupture
Treatment and Management
- Aims for optimizing foot biomechanics, controlling symptoms (pain, swelling, inflammation), protecting the inflamed tendon, and enhancing tendon healing and muscle activity balance.
- Conservative management:
- Medication (NSAIDs)
- Physical therapy (RICE, cross-training, and specific exercises)
- Corticosteroid injections (use cautiously, risk of rupture)
- Platelet-Rich Plasma (PRP) injections
- Surgical management is considered if conservative approaches fail.
- Physical therapy includes:
- Implementing RICE (Rest, Ice, Compression, Elevation)
- Orthotics (heel lifts, specialized braces)
- Taping
- Gentle stretching of tight gastrocnemius/soleus complex.
- Isometric-loaded exercises (e.g., heel raises) to strengthen tendons, progressing to more challenging exercises with weight.
- Cross-training on opposite ankle
- Specific positions to reduce pressure on the affected area
- Physiotherapy treatments (e.g soft tissue mobilization)
- The physician may recommend using a walking boot for a short period in case of severe pain.
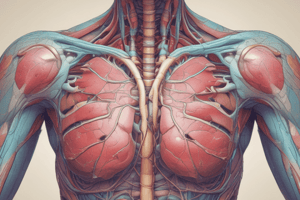
Thoracic Outlet Syndrome (TOS)
- Compression of neurovascular structures (nerves, blood vessels) exiting the thoracic outlet.
- Outlet is bordered by the first rib, clavicle, upper border of the scapula, and sternum.
- Marked by the anterior scalene, middle scalene, and subclavian vasculature/neurovascular bundle.
- The thoracic outlet is both confined and dynamic.
- Symptoms are often controversial and depend on whether the nerves, blood vessels, or both are compressed.
- Typical findings include:
- Numbness or tingling in the arm or fingers.
- Pain or aches in neck, shoulder, arm, or hand.
- Arm fatigue with activity.
- Weakening grip.
- Typical findings include:
- Causes of TOS often are anatomical defects:
- Extra rib located above first rib.
- Cervical ribs (0.5-0.6% pop., 50-80% bilateral)
- Fibromuscular bands connected to cervical ribs (most neural compression cause).
- Poor posture, causing shortening of the sternocleidomastoid muscle, thereby creating a shortened scalene and pectoralis muscle grouping, which leads to improper head-neck alignment.
- Injuries or repetitive activities (e.g., typing, heavy lifting).
- Classifications:
- Vascular (vTOS):
- Color changes in hands, or fingers (cyanosis)
- Hand or arm pain and swelling
- Pulsating lump near collarbone.
- Cold hands or fingers.
- Hand and arm pain (claudication pain)
- Neurological (nTOS): (includes true and disputed types of nTOS)
- Vascular (vTOS):
- Diagnostic procedures include electrophysiological studies and imaging.
- Treatment involves physical therapy (mobilization, stretching), activity modification, and potentially surgery if conservative measures are unsuccessful.
Rehabilitation After Knee Arthroplasty
. Preoperative rehab includes measuring pain, swelling, functional ability, range of motion, and muscle strength. Patients are trained to use assistive devices like walkers or crutches, along with practicing isometric exercises, like quadriceps.
. Postoperative rehab includes deep breathing, ankle pumps, upper extremity exercises(e.g., moving the patella up and down), frequent quadriceps exercises, and attempts at SLR (straight leg raises) after the first two days if not contraindicated.
. Two main forms of management are used: No CPM or CPM. No CPM includes maintaining the knee in an extended position, using pressure bandages, and splints. CPM uses a continuous passive motion machine to actively exercise the knee post-surgery.
. The types of exercises used to rehabilitate the knee after surgery include isometric, active, and resisted exercises and are tailored to each patient's needs and determined by the surgeon.
. The rehabilitation process after knee arthroplasty varies based on the specific type of prosthesis (cemented or cemented-less, and the specific situation of each patient.
. Proprioception training, walking/stair climbing, and avoidance of twisting, jumping and running are crucial to consider in patient rehabilitation programs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.