Podcast
Questions and Answers
What anatomical feature contributes to a higher prevalence of thoracic outlet syndrome (TOS) in females?
What anatomical feature contributes to a higher prevalence of thoracic outlet syndrome (TOS) in females?
- Less-developed muscles (correct)
- Thicker pectoralis major
- Wider thoracic outlet
- Larger clavicle
Which site of compression is least likely to affect the brachial plexus in TOS cases?
Which site of compression is least likely to affect the brachial plexus in TOS cases?
- Sub-coracoid tunnel
- Costoclavicular space
- Thoracic aorta (correct)
- Interscalene triangle
What percentage of thoracic outlet syndrome cases are classified as vascular (vTOS)?
What percentage of thoracic outlet syndrome cases are classified as vascular (vTOS)?
- 3% (correct)
- 97%
- 25%
- 10%
In true neurological thoracic outlet syndrome (tTOS), which symptom is prominently associated?
In true neurological thoracic outlet syndrome (tTOS), which symptom is prominently associated?
Which anatomical defect is the most common cause of neural compression in TOS?
Which anatomical defect is the most common cause of neural compression in TOS?
What common postural feature is exhibited by individuals with thoracic outlet syndrome?
What common postural feature is exhibited by individuals with thoracic outlet syndrome?
Which factor is NOT a recognized cause of thoracic outlet syndrome?
Which factor is NOT a recognized cause of thoracic outlet syndrome?
How does a flexed head position contribute to thoracic outlet syndrome?
How does a flexed head position contribute to thoracic outlet syndrome?
What commonly causes thoracic outlet syndrome (TOS) related to repetitive activities?
What commonly causes thoracic outlet syndrome (TOS) related to repetitive activities?
Which diagnostic method is NOT typically used for confirming thoracic outlet syndrome?
Which diagnostic method is NOT typically used for confirming thoracic outlet syndrome?
What type of physical symptom is most indicative of neurogenic TOS?
What type of physical symptom is most indicative of neurogenic TOS?
Which finding is commonly associated with nerve conduction studies in TOS?
Which finding is commonly associated with nerve conduction studies in TOS?
What is a characteristic imaging study used to identify vascular thoracic outlet syndrome?
What is a characteristic imaging study used to identify vascular thoracic outlet syndrome?
Which statement accurately reflects the clinical presentation of thoracic outlet syndrome?
Which statement accurately reflects the clinical presentation of thoracic outlet syndrome?
Which anatomical structure is primarily affected in thoracic outlet syndrome related to muscular compression?
Which anatomical structure is primarily affected in thoracic outlet syndrome related to muscular compression?
In the context of thoracic outlet syndrome, which type of muscle involvement is most likely related to macro-trauma?
In the context of thoracic outlet syndrome, which type of muscle involvement is most likely related to macro-trauma?
What characterizes Compressors in thoracic outlet syndrome?
What characterizes Compressors in thoracic outlet syndrome?
Which symptom is NOT typically associated with venous thoracic outlet syndrome?
Which symptom is NOT typically associated with venous thoracic outlet syndrome?
In the context of disputed neurogenic TOS, what is meant by 'subjective weakness'?
In the context of disputed neurogenic TOS, what is meant by 'subjective weakness'?
Which of the following tests is used to assess for scalene muscle involvement in thoracic outlet syndrome?
Which of the following tests is used to assess for scalene muscle involvement in thoracic outlet syndrome?
What likely indicates a favorable outcome in patients experiencing nocturnal paresthesias?
What likely indicates a favorable outcome in patients experiencing nocturnal paresthesias?
What does the Roos Stress Test assess in patients with suspected thoracic outlet syndrome?
What does the Roos Stress Test assess in patients with suspected thoracic outlet syndrome?
What symptom is more commonly associated with Arterial Thoracic Outlet Syndrome?
What symptom is more commonly associated with Arterial Thoracic Outlet Syndrome?
Which test should be followed after the Roos Stress Test to further evaluate scalene muscle involvement?
Which test should be followed after the Roos Stress Test to further evaluate scalene muscle involvement?
What muscle group is primarily assessed for adaptive shortening in thoracic outlet syndrome?
What muscle group is primarily assessed for adaptive shortening in thoracic outlet syndrome?
What does a hard end-feel during cervical rotation-side bending testing indicate regarding the first rib?
What does a hard end-feel during cervical rotation-side bending testing indicate regarding the first rib?
Which symptom is associated with neurogenic thoracic outlet syndrome due to nerve compression?
Which symptom is associated with neurogenic thoracic outlet syndrome due to nerve compression?
Which position of the arm tends to exacerbate symptoms in patients with thoracic outlet syndrome?
Which position of the arm tends to exacerbate symptoms in patients with thoracic outlet syndrome?
What is a common presentation of symptoms when the lower plexus (C8, T1) is involved?
What is a common presentation of symptoms when the lower plexus (C8, T1) is involved?
Which of the following tests would best assess for first rib hypomobility?
Which of the following tests would best assess for first rib hypomobility?
What specific history could indicate clavicle malalignment during assessment?
What specific history could indicate clavicle malalignment during assessment?
What is likely a symptom of thoracic outlet syndrome when blood vessels are compressed?
What is likely a symptom of thoracic outlet syndrome when blood vessels are compressed?
What is the primary purpose of the Wright's test in assessing thoracic outlet syndrome?
What is the primary purpose of the Wright's test in assessing thoracic outlet syndrome?
Which treatment is considered after conservative management for thoracic outlet syndrome has failed?
Which treatment is considered after conservative management for thoracic outlet syndrome has failed?
In Morley’s Sign, when is tenderness in the supraclavicular fossa considered to have diagnostic value?
In Morley’s Sign, when is tenderness in the supraclavicular fossa considered to have diagnostic value?
What is the correct position of the patient when performing the Wright's test?
What is the correct position of the patient when performing the Wright's test?
Which technique is part of the physiotherapy treatment for thoracic outlet syndrome?
Which technique is part of the physiotherapy treatment for thoracic outlet syndrome?
What are the nonsteroidal anti-inflammatory drugs commonly used for in the management of thoracic outlet syndrome?
What are the nonsteroidal anti-inflammatory drugs commonly used for in the management of thoracic outlet syndrome?
In the technique for first rib self-mobilization, what is the primary action performed by the patient?
In the technique for first rib self-mobilization, what is the primary action performed by the patient?
What symptom is notably observed during the supraclavicular pressure test?
What symptom is notably observed during the supraclavicular pressure test?
Which of the following techniques focuses on unloading the neurovascular structures in the thoracic outlet before sleeping?
Which of the following techniques focuses on unloading the neurovascular structures in the thoracic outlet before sleeping?
What is a recommended sleeping position for patients suffering from TOS?
What is a recommended sleeping position for patients suffering from TOS?
Which intervention is suggested for patients with larger chests to help relieve tension in the thoracic outlet?
Which intervention is suggested for patients with larger chests to help relieve tension in the thoracic outlet?
How long should patients typically avoid overhead activities and lifting after surgery for TOS?
How long should patients typically avoid overhead activities and lifting after surgery for TOS?
What effect does consistent use of the Cyriax release technique have over time for patients with TOS?
What effect does consistent use of the Cyriax release technique have over time for patients with TOS?
What is the primary focus of postoperative physical therapy for patients recovering from surgery due to TOS?
What is the primary focus of postoperative physical therapy for patients recovering from surgery due to TOS?
Which of the following is NOT a recommended modification for improving sleep in TOS patients?
Which of the following is NOT a recommended modification for improving sleep in TOS patients?
In severe cases of TOS, which surgical procedure is mentioned as a potentially effective intervention?
In severe cases of TOS, which surgical procedure is mentioned as a potentially effective intervention?
Flashcards
Thoracic Outlet Syndrome (TOS)
Thoracic Outlet Syndrome (TOS)
A condition where nerves and blood vessels are compressed in the space between the collarbone and the first rib. This compression can cause pain, numbness, tingling, and weakness in the arm and hand.
Vascular Thoracic Outlet Syndrome (vTOS)
Vascular Thoracic Outlet Syndrome (vTOS)
A type of TOS where blood vessels, such as the subclavian artery and vein, are compressed.
Neurological Thoracic Outlet Syndrome (nTOS)
Neurological Thoracic Outlet Syndrome (nTOS)
A type of TOS where nerves of the brachial plexus are compressed.
True Neurological TOS (tTOS)
True Neurological TOS (tTOS)
Signup and view all the flashcards
Disputed / non-specific / Symptomatic TOS (sTOS)
Disputed / non-specific / Symptomatic TOS (sTOS)
Signup and view all the flashcards
Cervical Rib
Cervical Rib
Signup and view all the flashcards
Poor Posture and TOS
Poor Posture and TOS
Signup and view all the flashcards
Muscle Imbalances and TOS
Muscle Imbalances and TOS
Signup and view all the flashcards
Thoracic Outlet
Thoracic Outlet
Signup and view all the flashcards
Neurogenic Thoracic Outlet Syndrome (nTOS)
Neurogenic Thoracic Outlet Syndrome (nTOS)
Signup and view all the flashcards
First Rib Hypomobility
First Rib Hypomobility
Signup and view all the flashcards
Muscles Implicated in TOS
Muscles Implicated in TOS
Signup and view all the flashcards
TOS Symptoms During Specific Movements
TOS Symptoms During Specific Movements
Signup and view all the flashcards
What is Thoracic Outlet Syndrome?
What is Thoracic Outlet Syndrome?
Signup and view all the flashcards
How is TOS different after a traumatic accident?
How is TOS different after a traumatic accident?
Signup and view all the flashcards
What are some causes of TOS?
What are some causes of TOS?
Signup and view all the flashcards
What is a cervical rib?
What is a cervical rib?
Signup and view all the flashcards
How does posture affect TOS?
How does posture affect TOS?
Signup and view all the flashcards
How do muscle imbalances influence TOS?
How do muscle imbalances influence TOS?
Signup and view all the flashcards
What kind of tests are used to diagnose TOS?
What kind of tests are used to diagnose TOS?
Signup and view all the flashcards
What imaging methods help in diagnosing TOS?
What imaging methods help in diagnosing TOS?
Signup and view all the flashcards
Cyriax Release Technique
Cyriax Release Technique
Signup and view all the flashcards
True TOS
True TOS
Signup and view all the flashcards
Transaxillary Resection of the First Rib
Transaxillary Resection of the First Rib
Signup and view all the flashcards
Disputed TOS
Disputed TOS
Signup and view all the flashcards
Compressors
Compressors
Signup and view all the flashcards
Supraclavicular Scalenectomy
Supraclavicular Scalenectomy
Signup and view all the flashcards
Releasers
Releasers
Signup and view all the flashcards
Supportive Bra with Wide and Posterior-Crossing Straps
Supportive Bra with Wide and Posterior-Crossing Straps
Signup and view all the flashcards
Roos Stress Test
Roos Stress Test
Signup and view all the flashcards
Postural Re-education
Postural Re-education
Signup and view all the flashcards
Patient Education and Activity Modification
Patient Education and Activity Modification
Signup and view all the flashcards
Scalene Cramp Test
Scalene Cramp Test
Signup and view all the flashcards
Scalene Relief Test
Scalene Relief Test
Signup and view all the flashcards
Neural Mobilization
Neural Mobilization
Signup and view all the flashcards
Upper Limb Tension Tests (ULTTs)
Upper Limb Tension Tests (ULTTs)
Signup and view all the flashcards
Supportive Taping
Supportive Taping
Signup and view all the flashcards
Morley's Sign
Morley's Sign
Signup and view all the flashcards
Supraclavicular Pressure Test
Supraclavicular Pressure Test
Signup and view all the flashcards
Wright's Test
Wright's Test
Signup and view all the flashcards
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
Non-steroidal Anti-inflammatory Drugs (NSAIDs)
Signup and view all the flashcards
Botox Injections
Botox Injections
Signup and view all the flashcards
First Rib Mobilization
First Rib Mobilization
Signup and view all the flashcards
Cervical & Thoracic Mobilization
Cervical & Thoracic Mobilization
Signup and view all the flashcards
Sternoclavicular & Acromioclavicular Joint Mobilization
Sternoclavicular & Acromioclavicular Joint Mobilization
Signup and view all the flashcards
Study Notes
Thoracic Outlet Syndrome (TOS)
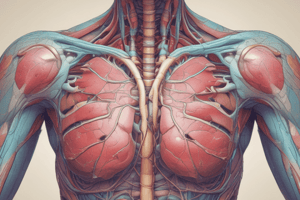
- TOS describes compression of neurovascular structures exiting the thoracic outlet.
- The thoracic outlet is a dynamic space bordered by the first rib, clavicle, and scapula.
- Structures in the thoracic outlet include the subclavian vasculature (veins and artery) and brachial plexus.
- TOS is a controversial topic in musculoskeletal medicine and rehabilitation.
- Pain and discomfort are often due to compressed subclavian vein, artery, or brachial plexus.
- The lowest trunk of the brachial plexus (C8 and T1 nerve roots) is the most commonly compressed structure.
- TOS affects approximately 8% of the population, and is more common in women (3-4 times more) between 20-50 years (average age 30s-40s).
- Mostly affects the brachial plexus (95-98%).
- Possible compression sites include the interscalene triangle, costoclavicular space, and subcoracoid tunnel.
- Causes of TOS may include congenital defects, like extra ribs, or fibromuscular bands.
Classification of TOS
- Vascular TOS (vTOS): Accounts for approximately 3% of cases. Compression affects the vascular structures (arteries or veins).
- Neurological TOS (nTOS): Accounts for approximately 97% of cases. Compression affects the neural structures (brachial plexus) which can be further divided into:
- True Neurological TOS (TOS): Associated with definitive neurological deficits (mostly muscular atrophy).
- Disputed/Non-specific/Symptomatic TOS (STOS): Associated with TOS symptoms but with no objective neurological, electro-physical or radiological abnormalities.
- TOS causes are anatomical defects (extra ribs, or fibromuscular bands), poor posture, or trauma.
Causes
- Congenital Defects: Presence of extra ribs, or cervical ribs.
- Often bilateral
- Affects 0.5-0.6% of people
- Fibromuscular bands connected to the cervical ribs also cause neural compression.
- Poor Posture: Flexed head, depressed and anteriorly shifted shoulders, and protracted scapula contribute to decreased costoclavicular space, increased friction on neurovascular bundle in the subpectoral area, and shortening of the sternocleidomastoid. Scalenes and pectoralis tightening leads to improper head/neck alignment.
Causes (cont.)
- Trauma: Macro-trauma (e.g., motor vehicle accident (MVA)) leading to injury and scarring of the scalene muscle or microtrauma (e.g. repetitive overhead activities like sports) leading to muscle strain in the scapular stabilizers.
- Repetitive Activity: Certain activities (e.g. typing on a computer, lifting heavy objects) can contribute to TOS after years of repetitive movements.
Diagnosis
- Based on a patient history, physical examination, provocative tests, ultrasound, radiological evaluation, and electrodiagnostic evaluation.
- Diagnosis usually involves ruling out other possible causes with similar presentations, such as cervical radiculopathies and upper extremity entrapment neuropathies.
- The clinical presentation is assessed and categorized as either neurogenic (compression of the brachial plexus) or vascular (compression of the subclavian vessels).
Diagnosis (cont)
- Electrodiagnostic evaluation: Nerve conduction studies are helpful and usually reveal decreased ulnar sensory potentials, decreased median action potentials, but often normal ulnar motor and median sensory potentials. Doesn't usually present in dermatomal/myotomal pattern unless nerve roots are involved.
- Imaging Studies: Venography and arteriography are used to identify vascular TOS. Cervical spine and chest x-rays are used to identify bony abnormalities, such as cervical ribs.
Physical Examination
- Assessment of Respiration: Ensure correct Abdominodiaphragmatic breathing.
- Assessment of Thoracic Outlet Closer Muscles: Look for adaptability and shortening of Anterior and middle scalenes, subclavius, pectoralis minor and major muscles.
- Assessment of 1st Rib Position and Mobility: Monitor rib elevation due to scalene hypertonicity or post-fracture callus formation.
- Clavicle Position assessment: Look for prior fracture history and an abnormal callus formation or malalignment.
- Additional tests like cervical rotation-side bending, assessment of scapular position and muscle strength, and acromioclavicular and sternoclavicular joint mobility are usually performed.
Signs and Symptoms
- Present anywhere from neck, face, and occipital region to chest, shoulder, and upper extremity pain.
- Pain and symptoms worsen during arm abduction, overhead, external rotation with head rotated towards affected side.
- Symptoms depend on whether the nerves, blood vessels or both are compressed.
- Neurogenic symptoms include numbness/tingling in the arm/fingers, pain/aches in the neck, shoulder, arm or hand, arm fatigue, and weakness in grip.
- More specific symptoms depend on which nerve is implicated at the upper or lower plexus.
Signs and Symptoms (cont.)
- Vascular TOS: Cyanosis of the hand/fingers; swelling, pain, cold intolerance of hands/arms/fingers. Possible loss of pulse in the affected arm or claudication pain that worsens whilst using affected arm.
- True TOS: Pain, paresthesia (numbness/tingling), and/or weakness, often present both during the day and night and related to the level of compression.
Provocative Testing (e.g.)
- Roos Test: Triggers spontaneously experienced symptoms (pain/numbness/tingling) in the patient within 1 minute. The patient has 90 degrees of abduction with the elbow flexed, while rotating externally, and opening and closing their hands for 3 minutes.
- Scalene Cramp Test: Follow-up to the Roos test to assess scalene muscle contribution to compression. The patient turns their head toward the side of the pain, and pulls their chin into the supraclavicular fossa to cause contraction of scalene muscles. Distal radiation of pain confirms scalene involvement.
- Scalene Relief Test: To further confirm scalene involvement, the patient’s forearm is placed against their forehead on the side of affected shoulder. Increase in space between the clavicle and scalene muscles suggests improved compression.
- Upper limb tension test (ULTT) or Brachial Plexus tension or Elvey's test: Various provocative tests to evaluate brachial plexus compression.
Special Vascular Tests
- Adson's Test: Used to identify vascular compression by compressing the subclavian vessels against the scalene, producing loss of radial pulse - indicative of TOS.
- Wright's Test: Considered the optimal provocative test for assessing costoclavicular compression. Patient's shoulders are externally rotated and abduct up to 180 degrees while maintaining a posterior position and keeping elbow extended.
Treatment
- Medical Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation. Botulinum injections (Botox) into the anterior and middle scalene muscles can temporarily reduce pain and spasm.
- Surgical Management: Considered only when conservative management proves ineffective. This may include procedures like supraclavicular scalene surgery and transaxillary first rib resection if all nerve and vascular structures are completely released and when applicable.
- Physiotherapy: First rib mobilization and manipulation, mobilization of sternoclavicular/acromioclavicular joints, Glenohumeral mobilization, Cervical traction, Massage, stretching, and strengthening exercises. Patient education and activity modification.
Postoperative Physical Therapy
- Gentle neural mobilization techniques
- Overhead activities and heavy lifting are avoided for 2-4 weeks
- Exercise programs are designed to address postural abnormalities, and muscle imbalances to prevent re-occurrence of symptoms
Management (cont)
- Patient Education and Activity Modification: Avoiding positions that exacerbate symptoms and adapting work/activities as needed.
- Sleep Positioning: Avoiding sleeping on the affected side and lying on the stomach. Using pillows to support the affected arm and keep it from being abducted overhead.
- Cyriax Release Technique: Position patients with arm rests to actively unload neurovascular structures during sleeping. Gradual increase in symptoms initially, then gradually disappear.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.