Podcast
Questions and Answers
Thoracic Outlet Syndrome (TOS) primarily involves the compression or entrapment of which neurovascular structure?
Thoracic Outlet Syndrome (TOS) primarily involves the compression or entrapment of which neurovascular structure?
- Sciatic nerve
- Brachial plexus (correct)
- Vagus nerve
- Femoral nerve
Neuropraxia, a common consequence of Thoracic Outlet Syndrome, is best described as which of the following?
Neuropraxia, a common consequence of Thoracic Outlet Syndrome, is best described as which of the following?
- A mild form of nerve injury characterized by temporary nerve conduction block. (correct)
- Progressive degeneration of the myelin sheath of nerve fibers.
- Irreversible compression of the spinal cord.
- Permanent nerve damage due to complete nerve severance.
Which anatomical structures define the boundaries of the interscalene triangle, a common site of compression in Thoracic Outlet Syndrome?
Which anatomical structures define the boundaries of the interscalene triangle, a common site of compression in Thoracic Outlet Syndrome?
- Sternocleidomastoid, clavicle, and first rib
- Anterior scalene, middle scalene, and first rib (correct)
- Pectoralis minor, coracoid process, and humerus
- Trapezius, posterior scalene, and second rib
Besides the interscalene triangle, where else can compression occur in Thoracic Outlet Syndrome?
Besides the interscalene triangle, where else can compression occur in Thoracic Outlet Syndrome?
Which combination of bony structures contributes to defining one of the main compression sites in Thoracic Outlet Syndrome?
Which combination of bony structures contributes to defining one of the main compression sites in Thoracic Outlet Syndrome?
A patient reports numbness and tingling in their hand, especially when sleeping with their elbow flexed. Which anatomical structure is MOST likely affected by this sleeping position?
A patient reports numbness and tingling in their hand, especially when sleeping with their elbow flexed. Which anatomical structure is MOST likely affected by this sleeping position?
A patient presents with symptoms of pain, numbness, and tingling in the upper extremity. After postural assessment, palpation, and range of motion testing, which muscle would be MOST relevant to assess for weakness contributing to thoracic outlet syndrome?
A patient presents with symptoms of pain, numbness, and tingling in the upper extremity. After postural assessment, palpation, and range of motion testing, which muscle would be MOST relevant to assess for weakness contributing to thoracic outlet syndrome?
A patient reports pain and paresthesia in the medial aspect of their forearm and hand. Which condition should be included in the differential diagnosis?
A patient reports pain and paresthesia in the medial aspect of their forearm and hand. Which condition should be included in the differential diagnosis?
Which intervention is MOST appropriate for a patient exhibiting signs of apical breathing pattern?
Which intervention is MOST appropriate for a patient exhibiting signs of apical breathing pattern?
A patient's symptoms are aggravated by carrying heavy items on their shoulder. Which structure is MOST likely involved?
A patient's symptoms are aggravated by carrying heavy items on their shoulder. Which structure is MOST likely involved?
What is the MOST appropriate initial treatment strategy for a patient presenting with suspected venous thoracic outlet syndrome?
What is the MOST appropriate initial treatment strategy for a patient presenting with suspected venous thoracic outlet syndrome?
A patient presents with a positive Adson's test. Which muscle group should be PRIORITY when initiating manual therapy?
A patient presents with a positive Adson's test. Which muscle group should be PRIORITY when initiating manual therapy?
A patient has decreased lateral flexion and rotation of the cervical spine. Which soft tissue structure is MOST likely contributing to THOS?
A patient has decreased lateral flexion and rotation of the cervical spine. Which soft tissue structure is MOST likely contributing to THOS?
A patient reports clumsiness and decreased dexterity in their hand, along with colour and temperature changes. Which of the following structures is MOST likely involved in these symptoms?
A patient reports clumsiness and decreased dexterity in their hand, along with colour and temperature changes. Which of the following structures is MOST likely involved in these symptoms?
A patient is diagnosed with thoracic outlet syndrome related to pec minor hypertonicity. Which of the following is an appropriate home exercise?
A patient is diagnosed with thoracic outlet syndrome related to pec minor hypertonicity. Which of the following is an appropriate home exercise?
Compression of the medial cord in thoracic outlet syndrome (TOS) primarily affects which nerve distribution?
Compression of the medial cord in thoracic outlet syndrome (TOS) primarily affects which nerve distribution?
Which of the following is the MOST likely presentation of neurogenic thoracic outlet syndrome (nTOS)?
Which of the following is the MOST likely presentation of neurogenic thoracic outlet syndrome (nTOS)?
Edema in the dorsum of the hand and cyanosis are MOST indicative of which type of thoracic outlet syndrome (TOS)?
Edema in the dorsum of the hand and cyanosis are MOST indicative of which type of thoracic outlet syndrome (TOS)?
A patient presents with coldness and pallor in the affected extremity. Which type of thoracic outlet syndrome (TOS) is MOST likely?
A patient presents with coldness and pallor in the affected extremity. Which type of thoracic outlet syndrome (TOS) is MOST likely?
Which anatomical structure, when overgrown, can lead to compression in the thoracic outlet, specifically affecting structures closest to the plexus?
Which anatomical structure, when overgrown, can lead to compression in the thoracic outlet, specifically affecting structures closest to the plexus?
A patient reports symptoms consistent with TOS that started after habitually carrying a heavy bag on one shoulder. Which compression site is MOST likely contributing to their symptoms?
A patient reports symptoms consistent with TOS that started after habitually carrying a heavy bag on one shoulder. Which compression site is MOST likely contributing to their symptoms?
A patient with TOS reports their symptoms are reproduced when they are sleeping with their arms in an overhead position. Which compression site is MOST likely involved?
A patient with TOS reports their symptoms are reproduced when they are sleeping with their arms in an overhead position. Which compression site is MOST likely involved?
During the examination of a patient, which finding would suggest that compression is NOT occurring at the interscalene triangle?
During the examination of a patient, which finding would suggest that compression is NOT occurring at the interscalene triangle?
Froment's sign, indicative of weakness in adductor pollicis, is MOST likely observed in which type of TOS?
Froment's sign, indicative of weakness in adductor pollicis, is MOST likely observed in which type of TOS?
Which of the following factors is MOST likely to contribute to the insidious onset of thoracic outlet syndrome (TOS)?
Which of the following factors is MOST likely to contribute to the insidious onset of thoracic outlet syndrome (TOS)?
A patient presents with sensory changes in the fifth digit and the medial half of the fourth digit on both the palm and dorsum of the hand. Which nerve is MOST likely involved?
A patient presents with sensory changes in the fifth digit and the medial half of the fourth digit on both the palm and dorsum of the hand. Which nerve is MOST likely involved?
Which of the following is NOT a typical symptom associated with arterial thoracic outlet syndrome (aTOS)?
Which of the following is NOT a typical symptom associated with arterial thoracic outlet syndrome (aTOS)?
Which nerve roots contribute to the formation of the lateral cord of the brachial plexus?
Which nerve roots contribute to the formation of the lateral cord of the brachial plexus?
Which of the following muscles is NOT directly related to a known compression site in thoracic outlet syndrome (TOS)?
Which of the following muscles is NOT directly related to a known compression site in thoracic outlet syndrome (TOS)?
Which of the following statements accurately describes a key difference between nerve root compression and cord compression in the context of TOS?
Which of the following statements accurately describes a key difference between nerve root compression and cord compression in the context of TOS?
Flashcards
Thoracic Outlet Syndrome (TOS)
Thoracic Outlet Syndrome (TOS)
Compression of neurovascular tissues of the brachial plexus.
Neuropraxia
Neuropraxia
Usually a mild nerve injury due to compression.
Interscalene Triangle Borders
Interscalene Triangle Borders
Anterior scalene, Middle scalene, and Rib 1.
Neurovascular Compression
Neurovascular Compression
Signup and view all the flashcards
Costoclavicular space borders
Costoclavicular space borders
Signup and view all the flashcards
TOS Symptoms
TOS Symptoms
Signup and view all the flashcards
Elbow Flexion & Sleep
Elbow Flexion & Sleep
Signup and view all the flashcards
Overhead Postures
Overhead Postures
Signup and view all the flashcards
C-Spine ROM Restriction
C-Spine ROM Restriction
Signup and view all the flashcards
TOS Muscle Imbalances
TOS Muscle Imbalances
Signup and view all the flashcards
Ulnar Nerve Compression
Ulnar Nerve Compression
Signup and view all the flashcards
Scalene Treatment
Scalene Treatment
Signup and view all the flashcards
Pec Minor Treatment
Pec Minor Treatment
Signup and view all the flashcards
Venous Symptom Treatment
Venous Symptom Treatment
Signup and view all the flashcards
TOS - ADL Modifications
TOS - ADL Modifications
Signup and view all the flashcards
Cervical Rib
Cervical Rib
Signup and view all the flashcards
Brachial Plexus Roots
Brachial Plexus Roots
Signup and view all the flashcards
Brachial Plexus Trunks
Brachial Plexus Trunks
Signup and view all the flashcards
Brachial Plexus Divisions
Brachial Plexus Divisions
Signup and view all the flashcards
Brachial Plexus Cords
Brachial Plexus Cords
Signup and view all the flashcards
Brachial Plexus Branches
Brachial Plexus Branches
Signup and view all the flashcards
nTOS Affected Area
nTOS Affected Area
Signup and view all the flashcards
nTOS Sensory Symptoms
nTOS Sensory Symptoms
Signup and view all the flashcards
Anterior Scalene Syndrome
Anterior Scalene Syndrome
Signup and view all the flashcards
Costoclavicular Syndrome
Costoclavicular Syndrome
Signup and view all the flashcards
Pec Minor Syndrome
Pec Minor Syndrome
Signup and view all the flashcards
Study Notes
- Study notes for Class 3
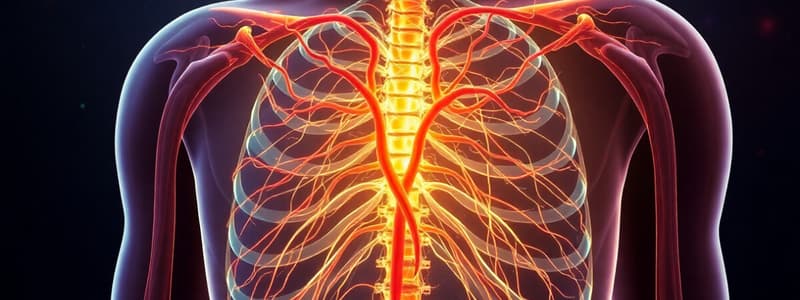
Thoracic Outlet Syndrome (TOS)
- Involves compression or entrapment of neurovascular tissues of the brachial plexus, usually neuropraxia.
- There are 3 main compression sites:
- Interscalene triangle (anterior, middle scalene, and rib 1).
- Clavicle and first rib (clavicle, rib 1, scapula).
- Coracoid process and pec minor (coracoid process, pectoralis minor, ribs 2-4).
- A 4th compression site can occur in the presence of a cervical rib.
- Cervical Rib: An anatomical anomaly where an overgrown C7 transverse process resembles a rib, attaching from C7 to rib 1.
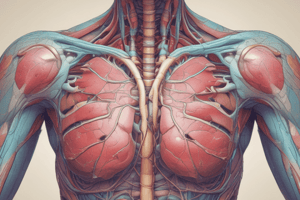
Brachial Plexus Anatomy
- Roots: C5-C8 & T1.
- Trunks: Superior, Middle, Inferior.
- Divisions: Anterior, Posterior.
- Cords: Lateral (C5-C7), Posterior (C5-T1), Medial (C8-T1).
- Branches: Musculocutaneous (lateral cord), Axillary (posterior cord), Radial (posterior cord), Median (lateral & medial cords), Ulnar (medial cord) and 11 other nerves.
Structural/Congenital Factors Contributing to TOS
- Cervical rib
- Sprengel deformity
- Scoliosis Acquired factors:
- Postural considerations
- Repetitive use (crutches, overhead movements)
- Clavicle/rib fractures
- Trauma (whiplash, dislocations)
- Hypertrophied muscles, short muscles
- Edema
Pathophysiology & Symptoms
- Nerve involvement leads to pain (local and referred), sensory loss or changes, and subtle motor weakness (not flaccidity), most common presentation.
- Vein compression causes edema (especially on the dorsum of the hand) and cyanosis.
- Artery compression results in coldness in extremities, pallor, and trophic changes (if severe).
- The medial cord (C8-T1, terminating in the ulnar nerve) is the most commonly compressed part of the brachial plexus in TOS.
- Neural symptoms often present in an ulnar nerve distribution (~90% of cases).
- Symptoms do not follow myotome/dermatome patterns since compression occurs at the cord level, not the root level.
- Subtle weakness & atrophy can occur in wrist flexion and ulnar deviation, adductor pollicis (positive Froment's sign), and intrinsic hand muscles.
- Sensory symptoms include changes in digit 5 and the medial half of digit 4 (both palm and dorsum), sometimes through the forearm distal to the cubital tunnel.
Clinical Presentation
- Pain in neck, shoulder, chest, upper extremity
- Altered sensation in upper extremity (day or night), usually in ulnar nerve distribution.
- Weakness in upper extremity, loss of coordination.
- Hand pain.
- Claudication, pallor, cold intolerance, cyanosis, heaviness.
- Paresthesia
Onset
- Usually insidious, but can be related to:
- Internal compression - cervical rib
- External compression - crutches
- Poor posture - hyperkyphosis, scoliosis
- Systemic disorders - RA, diabetes, hypothyroid
- Trauma/joint subluxation - whiplash
- Pregnancy - fluid retention plus postural changes
Anterior Scalene Syndrome
- Related to hypertoned/inflamed scalenes or trigger points in scalenes (a differential diagnosis).
- Can present with neural or arterial symptoms.
- Symptoms are venous if compression is not occurring at interscalene triangle
Costoclavicular Syndrome
- Related to tone/inflammation of subclavius or trigger points in subclavius (a differential diagnosis).
- Related to depressed shoulders (from heavy bags) or chronic respiratory problems.
- Can cause neural, arterial, or venous symptoms.
- Is the neurovascular compression site most likely to cause venous symptoms such as distal edema.
Pec Minor Syndrome (Hyperabduction Syndrome)
- Related to sustained or habitual overhead postures/activities (sleep position, work/labor, violin/flute).
- Overhead position stretches the neurovascular bundle between the coracoid process and pec minor tendon.
- Can cause neural, arterial, or venous symptoms.
Precaution
- Informed consent should include the possibility of symptom recreation during treatment.
- Discomfort may last 1-2 days
Compression & Sensory Symptoms (Scalenii Anticus and Medius)
- digit 5 and medial 4
- Test Postures
- Supine/Sidelying
- Tests: Adsons, Halstead's/Travell's
Costoclavicular Syndrome
- Sensory symptoms in digit 5 and medial 4
- Edema
- Positive Costoclavicular syndrome test , Eden's
Pec Minor Syndrome
- Sensory symptoms in digit 5 and medial 4.
- Edema
- Activities: Overhead postures or activities
- Wright's Test
History Taking
- Determine the exact location and nature of the symptoms i.e. pain, prickling, tingling, numbness
- Determine Quality of symptoms i.e. pain/coordination etc
- Assess ADLs and sleeping position
Obvs/Palp/Mvmt
- Postural scan
- Palpate for tenderness, hypertonic muscles, fascial restrictions
- C-Spine/GH ROM - most likely will see decreased ROM in lateral flexion and rotation
Muscle Strength Testing
- Assessing for imbalances or weakness in
- Scalenes
- Pec major/minor
- Levator scapulae
- Serratus anterior
Differential Diagnosis
- Scalenes trigger points (TrP).
- Subclavius TrP.
- Pec Minor TrP.
- Raynaud's
- Peripheral ulnar nerve compression (ulnar groove/cubital tunnel, Guyon's canal).
- Ulnar nerve tension.
- Nerve root compression (C8).
- Carpal tunnel syndrome.
- Pronator teres syndrome.
- Brachial plexus injuries.
- Tendinopathies.
Treatment
- Decompress the glitchy bits
- Scalenes (massage, MET, PIR, NMT, lateral translations, PA glides).
- Costoclavicular space (subclavius, superior glides SC joint, anterior glides SC joint, pec major).
- Pec minor (massage, supine or side-lying stretches/inhibition).
- Continue distally along the medial cord, addressing medial intermuscular septum, FCU, and hypothenar muscles.
- Treat underlying compression source.
Homecare Recommendations
- Hydrotherapy and stretches
- Diaphragmatic breathing
- ADL modifications, especially sleeping position.
- Elevate, unidirectional stroking, manual lymphatic drainage.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.