Podcast
Questions and Answers
What does it mean that the vascular system is a 'closed-loop' system?
What does it mean that the vascular system is a 'closed-loop' system?
- It only transports blood in one direction
- It allows blood to leave and re-enter the system freely
- Blood flows only to the heart and lungs
- Blood circulates within vessels without leaving the system (correct)
What gas does the vascular system primarily remove from tissues?
What gas does the vascular system primarily remove from tissues?
- Hydrogen (H₂)
- Methane (CH₄)
- Nitrogen (N₂)
- Carbon Dioxide (CO₂) (correct)
Which essential function does the vascular system serve for cells?
Which essential function does the vascular system serve for cells?
- Supplying cells with nutrients absorbed from the digestive system (correct)
- Filtering waste products
- Generating energy directly in the bloodstream
- Transmitting nerve signals
For what processes are proteins and amino acids transported by the vascular system important?
For what processes are proteins and amino acids transported by the vascular system important?
How does the vascular system assist in immune defense?
How does the vascular system assist in immune defense?
What role do arteries play in the circulatory system?
What role do arteries play in the circulatory system?
What is the function of capillaries in the vascular system?
What is the function of capillaries in the vascular system?
Which statement accurately describes venules?
Which statement accurately describes venules?
How do arterioles differ from arteries?
How do arterioles differ from arteries?
What is the primary function of veins in the circulatory system?
What is the primary function of veins in the circulatory system?
Which layer of a blood vessel is responsible for anchoring it to surrounding tissues?
Which layer of a blood vessel is responsible for anchoring it to surrounding tissues?
What is the primary role of the Internal Elastic Lamina in the tunica interna?
What is the primary role of the Internal Elastic Lamina in the tunica interna?
What occurs during vasoconstriction in blood vessels?
What occurs during vasoconstriction in blood vessels?
What component of the tunica media allows for changes in the diameter of blood vessels?
What component of the tunica media allows for changes in the diameter of blood vessels?
Which layer of a blood vessel contains both elastic and collagen fibers?
Which layer of a blood vessel contains both elastic and collagen fibers?
Which artery is considered an elastic artery?
Which artery is considered an elastic artery?
What is the primary reason that elastic arteries have large diameters?
What is the primary reason that elastic arteries have large diameters?
What component in the tunica media of elastic arteries provides elasticity?
What component in the tunica media of elastic arteries provides elasticity?
What occurs in elastic arteries when the heart ventricles contract?
What occurs in elastic arteries when the heart ventricles contract?
How do elastic arteries assist in maintaining blood flow during relaxation of the heart?
How do elastic arteries assist in maintaining blood flow during relaxation of the heart?
The ability of elastic arteries to act as a 'pressure reservoir' is primarily due to which characteristic?
The ability of elastic arteries to act as a 'pressure reservoir' is primarily due to which characteristic?
What is the key function of elastic fibers in elastic arteries?
What is the key function of elastic fibers in elastic arteries?
What happens to elastic arteries during the relaxation phase of the heart cycle?
What happens to elastic arteries during the relaxation phase of the heart cycle?
What is the primary role of muscular arteries in the circulatory system?
What is the primary role of muscular arteries in the circulatory system?
Which of the following components is abundant in the tunica media of muscular arteries?
Which of the following components is abundant in the tunica media of muscular arteries?
What mechanism allows blood to continue flowing in the case of a blockage in an area with arterial anastomoses?
What mechanism allows blood to continue flowing in the case of a blockage in an area with arterial anastomoses?
What defines the term 'vascular tone' in relation to muscular arteries?
What defines the term 'vascular tone' in relation to muscular arteries?
Why do muscular arteries lack significant recoil capability compared to elastic arteries?
Why do muscular arteries lack significant recoil capability compared to elastic arteries?
Which of the following correctly describes the tunica externa of muscular arteries?
Which of the following correctly describes the tunica externa of muscular arteries?
Which statement best explains why muscular arteries are known as 'distributing arteries'?
Which statement best explains why muscular arteries are known as 'distributing arteries'?
In terms of structure, how do muscular arteries differ from elastic arteries?
In terms of structure, how do muscular arteries differ from elastic arteries?
What is a key reason arterioles are referred to as 'resistance vessels'?
What is a key reason arterioles are referred to as 'resistance vessels'?
What is the typical diameter range of arterioles?
What is the typical diameter range of arterioles?
How do arterioles effectively control the blood flow into capillary beds?
How do arterioles effectively control the blood flow into capillary beds?
Which structure serves as the direct connection between arterioles and capillary beds?
Which structure serves as the direct connection between arterioles and capillary beds?
What is the primary function of pre-capillary sphincters located at capillary entry points?
What is the primary function of pre-capillary sphincters located at capillary entry points?
What does vasomotion refer to in the context of arterioles?
What does vasomotion refer to in the context of arterioles?
What types of signals can influence the phenomenon of vasomotion in arterioles?
What types of signals can influence the phenomenon of vasomotion in arterioles?
Which of the following best describes the role of the smooth muscle in arterioles?
Which of the following best describes the role of the smooth muscle in arterioles?
What is the diameter range of capillaries?
What is the diameter range of capillaries?
What structural feature enables capillaries to effectively exchange gases and nutrients?
What structural feature enables capillaries to effectively exchange gases and nutrients?
Capillaries connect which two types of blood vessels?
Capillaries connect which two types of blood vessels?
What is the primary function of capillary beds?
What is the primary function of capillary beds?
Microcirculation refers specifically to blood flow through which structures?
Microcirculation refers specifically to blood flow through which structures?
From which structure do capillary beds branch off?
From which structure do capillary beds branch off?
What role does a thoroughfare channel serve in a capillary network?
What role does a thoroughfare channel serve in a capillary network?
Which of the following is NOT a primary function of capillaries?
Which of the following is NOT a primary function of capillaries?
Which capillary type is characterized by having the smallest permeability, only permitting water and ions to pass through?
Which capillary type is characterized by having the smallest permeability, only permitting water and ions to pass through?
In which specific location are continuous capillaries predominantly found due to their selective permeability?
In which specific location are continuous capillaries predominantly found due to their selective permeability?
What structural feature of fenestrated capillaries enhances their permeability?
What structural feature of fenestrated capillaries enhances their permeability?
Fenestrated capillaries are most commonly found in which of the following locations?
Fenestrated capillaries are most commonly found in which of the following locations?
What allows sinusoid capillaries to facilitate the exchange of larger substances, including blood cells?
What allows sinusoid capillaries to facilitate the exchange of larger substances, including blood cells?
Where are sinusoid capillaries typically located?
Where are sinusoid capillaries typically located?
Which capillary type is expected in tissues requiring minimal and selective permeability, such as the central nervous system?
Which capillary type is expected in tissues requiring minimal and selective permeability, such as the central nervous system?
What drives the diffusion process for moving substances between the blood and tissues?
What drives the diffusion process for moving substances between the blood and tissues?
Which pathways allow water-soluble substances to move through capillary walls?
Which pathways allow water-soluble substances to move through capillary walls?
Lipid-soluble substances can cross the endothelial cells of capillaries because they are:
Lipid-soluble substances can cross the endothelial cells of capillaries because they are:
Why are plasma proteins generally unable to pass through most capillaries?
Why are plasma proteins generally unable to pass through most capillaries?
In which type of capillary can plasma proteins pass due to an increased permeability?
In which type of capillary can plasma proteins pass due to an increased permeability?
What is the main purpose of the blood-brain barrier (BBB)?
What is the main purpose of the blood-brain barrier (BBB)?
The blood-brain barrier is formed primarily due to which structural adaptation of brain capillaries?
The blood-brain barrier is formed primarily due to which structural adaptation of brain capillaries?
Which process primarily allows the movement of substances from blood into tissues?
Which process primarily allows the movement of substances from blood into tissues?
What mechanism is initially used to bring materials from blood plasma into endothelial cells during transcytosis?
What mechanism is initially used to bring materials from blood plasma into endothelial cells during transcytosis?
Which type of molecules primarily depend on transcytosis to cross capillary walls?
Which type of molecules primarily depend on transcytosis to cross capillary walls?
What is the final stage in the process of transcytosis that allows substances to enter the surrounding tissue?
What is the final stage in the process of transcytosis that allows substances to enter the surrounding tissue?
Why is transcytosis particularly significant in the context of the blood-brain barrier?
Why is transcytosis particularly significant in the context of the blood-brain barrier?
What is the primary purpose of transcytosis in capillaries?
What is the primary purpose of transcytosis in capillaries?
What primarily drives bulk flow in the circulatory system?
What primarily drives bulk flow in the circulatory system?
What is the primary purpose of filtration in the capillaries?
What is the primary purpose of filtration in the capillaries?
What condition can result from an imbalance between filtration and reabsorption?
What condition can result from an imbalance between filtration and reabsorption?
What drives fluid movement from the interstitial fluid back into the capillaries during reabsorption?
What drives fluid movement from the interstitial fluid back into the capillaries during reabsorption?
Where does reabsorption predominantly occur in the capillary network?
Where does reabsorption predominantly occur in the capillary network?
What important process is directly promoted by Blood Hydrostatic Pressure (BHP) in the capillaries?
What important process is directly promoted by Blood Hydrostatic Pressure (BHP) in the capillaries?
What is the typical range of Blood Hydrostatic Pressure (BHP) from the arterial end to the venous end of capillaries?
What is the typical range of Blood Hydrostatic Pressure (BHP) from the arterial end to the venous end of capillaries?
What best explains the minimal role of Interstitial Fluid Hydrostatic Pressure (IFHP) in opposing filtration?
What best explains the minimal role of Interstitial Fluid Hydrostatic Pressure (IFHP) in opposing filtration?
Which pressure is generated by proteins in the interstitial fluid and assists in drawing water out of capillaries?
Which pressure is generated by proteins in the interstitial fluid and assists in drawing water out of capillaries?
What primarily drives the process of reabsorption in the capillaries?
What primarily drives the process of reabsorption in the capillaries?
What does a positive Net Filtration Pressure (NFP) at the arterial end of a capillary indicate?
What does a positive Net Filtration Pressure (NFP) at the arterial end of a capillary indicate?
Which two pressures are primarily responsible for promoting fluid reabsorption into capillaries?
Which two pressures are primarily responsible for promoting fluid reabsorption into capillaries?
Calculate the Net Filtration Pressure (NFP) at the venous end of a capillary given BHP = 16 mmHg, IFOP = 1 mmHg, BCOP = 26 mmHg, and IFHP = 0 mmHg.
Calculate the Net Filtration Pressure (NFP) at the venous end of a capillary given BHP = 16 mmHg, IFOP = 1 mmHg, BCOP = 26 mmHg, and IFHP = 0 mmHg.
Which pressures lead to fluid movement out of the capillaries during filtration?
Which pressures lead to fluid movement out of the capillaries during filtration?
What does a negative NFP at the venous end of a capillary signify?
What does a negative NFP at the venous end of a capillary signify?
What percentage of the fluid filtered out of capillaries is typically reabsorbed?
What percentage of the fluid filtered out of capillaries is typically reabsorbed?
How many liters of fluid are typically filtered out of capillaries into surrounding tissues each day?
How many liters of fluid are typically filtered out of capillaries into surrounding tissues each day?
What is the main function of the lymphatic system regarding excess fluid?
What is the main function of the lymphatic system regarding excess fluid?
Which of the following accurately describes edema?
Which of the following accurately describes edema?
Of the 20 liters of fluid filtered out daily, how many liters are reabsorbed back into the capillaries?
Of the 20 liters of fluid filtered out daily, how many liters are reabsorbed back into the capillaries?
What is the primary function of venules?
What is the primary function of venules?
Which of the following accurately describes postcapillary venules?
Which of the following accurately describes postcapillary venules?
As venules increase in size, which ability do they lose?
As venules increase in size, which ability do they lose?
What is the approximate diameter range of postcapillary venules?
What is the approximate diameter range of postcapillary venules?
During physical activity, how do the elastic walls of venules assist the circulatory system?
During physical activity, how do the elastic walls of venules assist the circulatory system?
What is the primary reason veins have thinner walls compared to arteries?
What is the primary reason veins have thinner walls compared to arteries?
Which layer of the vein contains the most connective tissue?
Which layer of the vein contains the most connective tissue?
What allows veins to hold varying volumes of blood effectively?
What allows veins to hold varying volumes of blood effectively?
Which anatomical feature is absent in veins but present in arteries?
Which anatomical feature is absent in veins but present in arteries?
Why are there more veins than arteries in the human body?
Why are there more veins than arteries in the human body?
What percentage of the body’s blood volume is typically found in the veins at any given time?
What percentage of the body’s blood volume is typically found in the veins at any given time?
Which feature of veins allows for minimal resistance to blood flow?
Which feature of veins allows for minimal resistance to blood flow?
What is the primary role of venous valves within the vascular system?
What is the primary role of venous valves within the vascular system?
Which layer of the vein wall is responsible for the formation of venous valves?
Which layer of the vein wall is responsible for the formation of venous valves?
Why are veins considered capacitance vessels?
Why are veins considered capacitance vessels?
What mechanism causes blood to pool in the veins, leading to varicose veins?
What mechanism causes blood to pool in the veins, leading to varicose veins?
How does prolonged standing or sitting contribute to the development of varicose veins?
How does prolonged standing or sitting contribute to the development of varicose veins?
Which of the following factors is NOT associated with an increased risk of developing varicose veins?
Which of the following factors is NOT associated with an increased risk of developing varicose veins?
Which type of veins are primarily affected by varicose veins?
Which type of veins are primarily affected by varicose veins?
What is the approximate percentage of adults that suffers from varicose veins?
What is the approximate percentage of adults that suffers from varicose veins?
What occurs when both the proximal and distal valves in a vein are open?
What occurs when both the proximal and distal valves in a vein are open?
What function does the proximal valve serve during muscle relaxation?
What function does the proximal valve serve during muscle relaxation?
What happens to the distal valve after muscle relaxation?
What happens to the distal valve after muscle relaxation?
Which statement best describes the role of the skeletal muscle pump?
Which statement best describes the role of the skeletal muscle pump?
In which part of the body is the skeletal muscle pump particularly important for promoting blood flow?
In which part of the body is the skeletal muscle pump particularly important for promoting blood flow?
What is the result of inhalation on the diaphragm's movement?
What is the result of inhalation on the diaphragm's movement?
What role does increased abdominal pressure during inhalation play?
What role does increased abdominal pressure during inhalation play?
What occurs in the thoracic and abdominal cavities during exhalation?
What occurs in the thoracic and abdominal cavities during exhalation?
What is the primary mechanism preventing blood from flowing backward during exhalation?
What is the primary mechanism preventing blood from flowing backward during exhalation?
What is the main function of the respiratory pump?
What is the main function of the respiratory pump?
What is the primary determinant of cardiac output in terms of its formula?
What is the primary determinant of cardiac output in terms of its formula?
If blood viscosity increases, what effect does it have on vascular resistance?
If blood viscosity increases, what effect does it have on vascular resistance?
Which two factors primarily influence the distribution of cardiac output?
Which two factors primarily influence the distribution of cardiac output?
What is the role of blood pressure in the circulatory system?
What is the role of blood pressure in the circulatory system?
Which factors are important in determining vascular resistance?
Which factors are important in determining vascular resistance?
What primarily causes blood pressure to drop as blood moves through the circulatory system?
What primarily causes blood pressure to drop as blood moves through the circulatory system?
Which type of blood vessel experiences the highest blood pressure?
Which type of blood vessel experiences the highest blood pressure?
What event occurs during systolic blood pressure measurements?
What event occurs during systolic blood pressure measurements?
How is diastolic blood pressure best defined?
How is diastolic blood pressure best defined?
What generates blood pressure in the circulatory system?
What generates blood pressure in the circulatory system?
Which formula correctly calculates Mean Arterial Pressure (MAP)?
Which formula correctly calculates Mean Arterial Pressure (MAP)?
What is the normal range for Mean Arterial Pressure (MAP) values?
What is the normal range for Mean Arterial Pressure (MAP) values?
Which factor would likely lead to a decrease in MAP?
Which factor would likely lead to a decrease in MAP?
What is the minimum Mean Arterial Pressure (MAP) generally required for adequate organ perfusion?
What is the minimum Mean Arterial Pressure (MAP) generally required for adequate organ perfusion?
Why is Mean Arterial Pressure (MAP) a better indicator of organ perfusion compared to systolic or diastolic pressure alone?
Why is Mean Arterial Pressure (MAP) a better indicator of organ perfusion compared to systolic or diastolic pressure alone?
Which factor has the most significant impact on vascular resistance due to its influence on the interaction between blood and vessel walls?
Which factor has the most significant impact on vascular resistance due to its influence on the interaction between blood and vessel walls?
What can be concluded about the relationship between blood vessel length and vascular resistance?
What can be concluded about the relationship between blood vessel length and vascular resistance?
What physiological process would result in narrowing blood vessels?
What physiological process would result in narrowing blood vessels?
How does dehydration influence blood viscosity and vascular resistance?
How does dehydration influence blood viscosity and vascular resistance?
What effect does vasodilation have on the diameter of blood vessels and vascular resistance?
What effect does vasodilation have on the diameter of blood vessels and vascular resistance?
What is the main reason blood flow velocity decreases in capillaries compared to larger vessels?
What is the main reason blood flow velocity decreases in capillaries compared to larger vessels?
How does blood flow velocity change as it returns to the heart through larger veins?
How does blood flow velocity change as it returns to the heart through larger veins?
Circulation time is primarily defined as the duration for which a drop of blood travels through which specific pathway?
Circulation time is primarily defined as the duration for which a drop of blood travels through which specific pathway?
What is the approximate circulation time for a drop of blood in a healthy adult?
What is the approximate circulation time for a drop of blood in a healthy adult?
In which segment of the vascular system is blood flow velocity at its peak?
In which segment of the vascular system is blood flow velocity at its peak?
What is the reason for the largest cross-sectional area occurring in capillaries?
What is the reason for the largest cross-sectional area occurring in capillaries?
Where does blood flow velocity reach its highest point?
Where does blood flow velocity reach its highest point?
Why is blood flow velocity lowest in the capillaries?
Why is blood flow velocity lowest in the capillaries?
What happens to blood velocity as it travels from capillaries to venules and veins?
What happens to blood velocity as it travels from capillaries to venules and veins?
In which blood vessel does the cross-sectional area not reach its maximum?
In which blood vessel does the cross-sectional area not reach its maximum?
What happens to blood pressure when heart rate increases?
What happens to blood pressure when heart rate increases?
Which mechanism primarily influences systemic vascular resistance?
Which mechanism primarily influences systemic vascular resistance?
What effect does vasoconstriction have on blood pressure?
What effect does vasoconstriction have on blood pressure?
How does blood volume impact blood pressure?
How does blood volume impact blood pressure?
Which system primarily manages long-term blood pressure regulation through blood volume control?
Which system primarily manages long-term blood pressure regulation through blood volume control?
What is the effect of heart rate on blood pressure?
What is the effect of heart rate on blood pressure?
Which factor primarily influences systemic vascular resistance?
Which factor primarily influences systemic vascular resistance?
What mechanism quickly adjusts blood pressure in the body?
What mechanism quickly adjusts blood pressure in the body?
How does vasoconstriction affect blood pressure?
How does vasoconstriction affect blood pressure?
Which organ primarily manages long-term regulation of blood pressure through blood volume control?
Which organ primarily manages long-term regulation of blood pressure through blood volume control?
What is the primary function of the Cardiovascular Center (CVC)?
What is the primary function of the Cardiovascular Center (CVC)?
Which group of neurons within the CVC is involved in controlling heart rate, contractility, and blood vessel diameter?
Which group of neurons within the CVC is involved in controlling heart rate, contractility, and blood vessel diameter?
What effect does the cardioinhibitory response of the CVC have on the heart?
What effect does the cardioinhibitory response of the CVC have on the heart?
What is primarily adjusted by the CVC's vasomotor center?
What is primarily adjusted by the CVC's vasomotor center?
What is a key role of the Cardiovascular Center (CVC) in relation to homeostasis?
What is a key role of the Cardiovascular Center (CVC) in relation to homeostasis?
Which brain region primarily governs emotions that influence heart rate and blood pressure?
Which brain region primarily governs emotions that influence heart rate and blood pressure?
Which sensory receptor detects changes in blood pressure and provides feedback to the cardiovascular control center?
Which sensory receptor detects changes in blood pressure and provides feedback to the cardiovascular control center?
What physiological factors does the hypothalamus influence in relation to the cardiovascular control center?
What physiological factors does the hypothalamus influence in relation to the cardiovascular control center?
Chemoreceptors send signals to the cardiovascular control center based on the levels of which substances in the blood?
Chemoreceptors send signals to the cardiovascular control center based on the levels of which substances in the blood?
Which type of receptor provides feedback on body position and movement to the cardiovascular control center during physical activity?
Which type of receptor provides feedback on body position and movement to the cardiovascular control center during physical activity?
Which nerves are primarily responsible for sending signals of the parasympathetic pathway to the heart?
Which nerves are primarily responsible for sending signals of the parasympathetic pathway to the heart?
What is the impact of the parasympathetic pathway on heart rate?
What is the impact of the parasympathetic pathway on heart rate?
How do vasomotor nerves affect blood pressure?
How do vasomotor nerves affect blood pressure?
Which pathway utilizes cardiac accelerator nerves to influence heart function?
Which pathway utilizes cardiac accelerator nerves to influence heart function?
What overall effect does the sympathetic pathway have on blood pressure?
What overall effect does the sympathetic pathway have on blood pressure?
What physiological role do baroreceptors play in the body?
What physiological role do baroreceptors play in the body?
Which action is taken by baroreceptors when blood pressure decreases?
Which action is taken by baroreceptors when blood pressure decreases?
Which of the following substances do chemoreceptors primarily monitor in the blood?
Which of the following substances do chemoreceptors primarily monitor in the blood?
What response is triggered by chemoreceptors when blood carbon dioxide levels increase?
What response is triggered by chemoreceptors when blood carbon dioxide levels increase?
Where are proprioceptors primarily located in the body?
Where are proprioceptors primarily located in the body?
What is the primary location of the carotid sinus?
What is the primary location of the carotid sinus?
What is the main purpose of the carotid sinus reflex?
What is the main purpose of the carotid sinus reflex?
Which cranial nerve is responsible for transmitting signals from the carotid sinus baroreceptors to the cardiovascular center?
Which cranial nerve is responsible for transmitting signals from the carotid sinus baroreceptors to the cardiovascular center?
What physiological change occurs when blood pressure increases in the carotid sinus?
What physiological change occurs when blood pressure increases in the carotid sinus?
The baroreceptors involved in the aortic reflex are located in which area?
The baroreceptors involved in the aortic reflex are located in which area?
Which cranial nerve transmits impulses from the aortic baroreceptors to the cardiovascular center?
Which cranial nerve transmits impulses from the aortic baroreceptors to the cardiovascular center?
What is the primary function of the aortic reflex?
What is the primary function of the aortic reflex?
Both the carotid sinus and aortic reflexes are crucial for what overall function?
Both the carotid sinus and aortic reflexes are crucial for what overall function?
What does the baroreceptor response entail when blood pressure decreases?
What does the baroreceptor response entail when blood pressure decreases?
Which mechanism primarily increases in response to low blood pressure?
Which mechanism primarily increases in response to low blood pressure?
What is the physiological effect of vasoconstriction on blood pressure?
What is the physiological effect of vasoconstriction on blood pressure?
How do baroreceptors react to elevated blood pressure?
How do baroreceptors react to elevated blood pressure?
What is the overall response to high blood pressure in terms of heart rate and cardiac output?
What is the overall response to high blood pressure in terms of heart rate and cardiac output?
What physiological change is indicated by low levels of oxygen in the blood?
What physiological change is indicated by low levels of oxygen in the blood?
Which type of condition is indicated by high levels of hydrogen ions (H⁺) in the blood?
Which type of condition is indicated by high levels of hydrogen ions (H⁺) in the blood?
How do chemoreceptors respond to detected hypoxia, acidosis, or hypercapnia?
How do chemoreceptors respond to detected hypoxia, acidosis, or hypercapnia?
Which effect does sympathetic stimulation have in response to chemoreceptor activity?
Which effect does sympathetic stimulation have in response to chemoreceptor activity?
Where are chemoreceptors predominantly located in the body?
Where are chemoreceptors predominantly located in the body?
Which changes in blood chemistry indicate hypoxia, acidosis, and hypercapnia?
Which changes in blood chemistry indicate hypoxia, acidosis, and hypercapnia?
Where are the chemoreceptors that detect changes in blood chemistry primarily located?
Where are the chemoreceptors that detect changes in blood chemistry primarily located?
Upon detecting hypoxia, acidosis, or hypercapnia, chemoreceptors signal which center in the brainstem?
Upon detecting hypoxia, acidosis, or hypercapnia, chemoreceptors signal which center in the brainstem?
What effect does activation of the vasomotor center have on heart function?
What effect does activation of the vasomotor center have on heart function?
How does vasoconstriction affect blood flow?
How does vasoconstriction affect blood flow?
What is a result of increased heart rate, cardiac output, and vasoconstriction?
What is a result of increased heart rate, cardiac output, and vasoconstriction?
What is the function of increased blood pressure in response to hypoxia and hypercapnia?
What is the function of increased blood pressure in response to hypoxia and hypercapnia?
What is the overall goal of the body’s response mechanism to blood chemistry changes?
What is the overall goal of the body’s response mechanism to blood chemistry changes?
What triggers the Renin-Angiotensin-Aldosterone (RAA) system?
What triggers the Renin-Angiotensin-Aldosterone (RAA) system?
What is the function of renin in the RAA system?
What is the function of renin in the RAA system?
Which enzyme is responsible for converting angiotensin I to angiotensin II?
Which enzyme is responsible for converting angiotensin I to angiotensin II?
How does angiotensin II primarily affect blood vessels?
How does angiotensin II primarily affect blood vessels?
What is the mechanism through which aldosterone raises blood pressure?
What is the mechanism through which aldosterone raises blood pressure?
What physiological response triggers the release of epinephrine and norepinephrine?
What physiological response triggers the release of epinephrine and norepinephrine?
What effect do epinephrine and norepinephrine have on blood pressure?
What effect do epinephrine and norepinephrine have on blood pressure?
In the context of the ‘fight or flight’ response, what roles do epinephrine and norepinephrine play?
In the context of the ‘fight or flight’ response, what roles do epinephrine and norepinephrine play?
What is the main function of Antidiuretic Hormone (ADH)?
What is the main function of Antidiuretic Hormone (ADH)?
What physiological condition triggers the release of Atrial Natriuretic Peptide (ANP)?
What physiological condition triggers the release of Atrial Natriuretic Peptide (ANP)?
Which of the following correctly describes how ANP reduces blood volume?
Which of the following correctly describes how ANP reduces blood volume?
ADH's effect on blood pressure primarily occurs through which mechanism?
ADH's effect on blood pressure primarily occurs through which mechanism?
What is the overall role of ANP in relation to blood pressure regulation?
What is the overall role of ANP in relation to blood pressure regulation?
What is the primary function of autoregulation in blood vessels?
What is the primary function of autoregulation in blood vessels?
What mechanism does the myogenic response utilize?
What mechanism does the myogenic response utilize?
What occurs to blood vessels during a vasoconstriction response?
What occurs to blood vessels during a vasoconstriction response?
Which of the following substances is primarily responsible for inducing vasodilation?
Which of the following substances is primarily responsible for inducing vasodilation?
How do endothelins affect blood vessels in the context of autoregulation?
How do endothelins affect blood vessels in the context of autoregulation?
What is the effect of warming on blood vessels?
What is the effect of warming on blood vessels?
What happens to the diameter of blood vessels when there is a rise in blood pressure as part of the myogenic response?
What happens to the diameter of blood vessels when there is a rise in blood pressure as part of the myogenic response?
Which response occurs during autoregulation to match blood flow to a tissue's metabolic needs?
Which response occurs during autoregulation to match blood flow to a tissue's metabolic needs?
What effect does an increase in blood volume primarily have on cardiac function?
What effect does an increase in blood volume primarily have on cardiac function?
What is the effect of sympathetic impulses from the adrenal medulla on the heart?
What is the effect of sympathetic impulses from the adrenal medulla on the heart?
Which mechanism is responsible for enhancing venous return?
Which mechanism is responsible for enhancing venous return?
How does increased blood viscosity affect systemic vascular resistance?
How does increased blood viscosity affect systemic vascular resistance?
Which factor contributes to an increase in systemic vascular resistance by expanding the vascular network?
Which factor contributes to an increase in systemic vascular resistance by expanding the vascular network?
What is the result of vasoconstriction on mean arterial pressure (MAP)?
What is the result of vasoconstriction on mean arterial pressure (MAP)?
What combination results in a significant rise in mean arterial pressure (MAP)?
What combination results in a significant rise in mean arterial pressure (MAP)?
What is the primary goal of regulating mean arterial pressure (MAP)?
What is the primary goal of regulating mean arterial pressure (MAP)?
Flashcards are hidden until you start studying
Study Notes
The Vascular System: A Closed Loop
- The vascular system is a closed-loop system, meaning that blood circulates within vessels without leaving the system.
- The vascular system is responsible for transporting oxygen to tissues and removing carbon dioxide.
Functions of the Vascular System
- Nutrient delivery: The vascular system delivers nutrients absorbed from the digestive system to cells throughout the body.
- Protein and amino acid transport: These molecules are essential for growth, repair, and metabolic processes.
- Immune response: The vascular system transports white blood cells to fight infections.
- Blood pressure regulation: The vascular system regulates blood volume to maintain blood pressure.
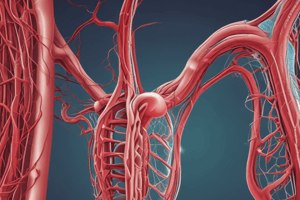
Blood Vessels
- Arteries transport blood away from the heart.
- Arterioles are smaller arteries.
- Capillaries are branches of arterioles.
- Venules are formed from the collection of capillaries.
- Veins return blood back to the heart.
Structure of Blood Vessels
-
Tunica Interna is the innermost layer of a blood vessel, and is in direct contact with blood.
- Endothelium is the single layer of epithelial cells that lines the vessel, providing a smooth surface to minimize friction for blood flow.
- Basement membrane is a thin layer of extracellular matrix that anchors the endothelium to the underlying tunica media.
- Internal elastic lamina is a layer of elastic fibers that provides elasticity to the vessel, allowing it to stretch and return to its original shape.
-
Tunica Media is the middle layer of a blood vessel and is primarily composed of smooth muscle cells.
- Smooth muscle cells regulate the diameter of the vessel’s lumen by contracting and relaxing. Contraction narrows the lumen, known as vasoconstriction, while relaxation widens the lumen called vasodilation.
-
Tunica Externa is the outermost layer of a blood vessel and is primarily composed of connective tissue.
- Collagen fibers provide structural support and flexibility.
- Elastic fibers provide elasticity, allowing the vessel to stretch and return to its original shape.
- Vasa vasorum are small blood vessels that supply blood to the walls of larger vessels, particularly the tunica externa.
Elastic Arteries
- The pulmonary trunk is classified as an elastic artery
- Elastic arteries have the largest diameters among blood vessels, allowing them to carry large volumes of blood
- Elastic fibers (lamellae) in the tunica media allow elastic arteries to stretch and recoil
- Elastic arteries expand to store mechanical energy during ventricular contraction
- Elastic arteries recoil during ventricular relaxation, helping to push blood forward
- The function of elastic arteries as a "pressure reservoir" is due to their ability to store mechanical energy when stretched and release it during relaxation
- The primary role of elastic fibers in the walls of elastic arteries is to allow stretching and recoiling with each heartbeat
Muscular Arteries
- Tunica Media: Primarily composed of smooth muscle cells, which are responsible for vasoconstriction and vasodilation.
- Function: Muscular arteries are distributing arteries, delivering blood to various organs and regions.
- Tunica Externa: Contains elastic longitudinal fibers, which provide support and flexibility.
- Vascular Tone: The state of partial contraction maintained by muscular arteries to regulate blood pressure and ensure a steady flow.
- Anastomoses: Connections between arterial branches, providing alternate routes for blood flow in case of blockage.
- Collateral Circulation: The flow of blood through alternate pathways established by anastomoses when a primary pathway is blocked.
- Recoil capability: Muscular arteries do not recoil like elastic arteries because they lack elastic fibers in the tunica media.
Arterioles: Resistance Vessels
- Arterioles are called "resistance vessels" because they directly regulate blood pressure and flow to capillary beds.
- The diameter of arterioles is typically 15–300 micrometers.
- Arterioles control blood flow into capillary beds by adjusting their diameter through smooth muscle contraction and relaxation.
- Metarterioles connect arterioles directly to capillary beds.
- Pre-capillary sphincters regulate blood flow within tissues and organs by controlling the entrance of capillary beds.
- Vasomotion is the intermittent contraction and relaxation of arteriole smooth muscle, which adjusts blood flow.
- Vasomotion is influenced by neural, hormonal, and chemical signals.
Capillary Structure and Function
- Capillaries are the smallest blood vessels with a diameter of approximately 5–10 micrometers.
- Capillaries have thin walls consisting only of an endothelial layer and a basement membrane, which enables efficient exchange of gases, nutrients, and waste products.
- Capillaries connect arterioles and venules.
- The extensive network formed by capillaries around body cells is essential for ensuring adequate oxygen and nutrient supply and waste removal.
Microcirculation
- Microcirculation refers to the flow of blood from metarterioles through capillaries to venules.
- A capillary bed provides an extensive surface area for exchange and branches from a metarteriole.
- A thoroughfare channel allows blood to travel directly from an arteriole to a venule, bypassing capillaries.
Capillary Types and Permeability
- Continuous capillaries have the least permeability.
- They allow only small molecules such as water and ions to pass through.
- They are commonly found in the blood-brain barrier where a controlled and selective exchange is needed.
- Fenestrated capillaries have increased permeability due to pores in their endothelial cells.
- These pores (fenestrations) allow larger molecules to pass through.
- They are typically found in areas requiring rapid filtration or absorption, such as kidneys, intestines, and endocrine glands.
- Sinusoid capillaries are highly permeable and allow for the exchange of large substances, including blood cells.
- This is due to their large fenestrations, wide shape, and incomplete basement membrane.
- They are found in locations like liver, spleen, and bone marrow, where large molecules and even cells need to pass through.
Capillary Exchange
- Diffusion - primary method of substance movement between blood and tissues, driven by concentration gradients.
- Water-soluble substances can pass through capillary walls via intercellular clefts and fenestrations.
- Lipid-soluble substances can move directly through endothelial cells, compatible with lipid bilayer of cell membranes.
- Plasma proteins are unable to pass through most capillaries due to their size, being too large for capillary structures.
- Sinusoids are highly permeable capillaries that allow passage of plasma proteins due to larger openings.
- Blood-brain barrier (BBB) is critical to restrict diffusion in the brain, ensuring only selective substances pass.
- Tight junctions between endothelial cells of brain capillaries form the structural foundation for the BBB.
Transcytosis
-
Transcytosis is a process that transports substances through endothelial cells using vesicles.
-
During transcytosis, materials from blood plasma initially enter the endothelial cell through endocytosis.
-
Large, lipid-insoluble molecules primarily utilize transcytosis to cross capillary walls.
-
The final step in transcytosis that allows substances to enter surrounding tissue is exocytosis.
-
Proteins and certain hormones are examples of substances that typically use transcytosis to cross capillary walls.
Transcytosis's Role in the Blood-Brain Barrier
- Transcytosis in the blood-brain barrier is crucial because it selectively transports large molecules.
Transcytosis in Capillaries
- The primary function of transcytosis in capillaries is to move large, lipid-insoluble molecules across capillary walls.
Bulk Flow: Pressure Driven Fluid Movement
- Bulk flow refers to the movement of fluids and solutes through a system based on pressure gradients. It is essential for the exchange of fluids and solutes between blood and tissues.
- Pressure gradients are the primary driving force for bulk flow. The pressure difference between fluid compartments creates movement from high-pressure areas to low-pressure areas.
- Filtration is the process where fluids and solutes move from blood within capillaries into the interstitial fluid, a process driven by hydrostatic pressure (blood pressure) being higher at the arterial end of capillaries.
- Reabsorption is the process where fluid moves from the interstitial fluid back into capillaries largely driven by osmotic pressure from plasma proteins, which is higher at the venous end of capillaries.
- Edema can occur if there's an imbalance between filtration and reabsorption, leading to excess interstitial fluid buildup in the tissues.
Understanding the Mechanisms:
- Hydrostatic pressure refers to the pressure exerted by a fluid, in this case, the blood, against the walls of the blood vessels. It is higher at the arterial end of capillaries due to blood being pumped from the heart.
- Osmotic pressure arises from the presence of solutes within a fluid, like plasma proteins in blood. It draws water towards areas with higher solute concentration.
- The difference between hydrostatic pressure and osmotic pressure at the capillary level determines whether filtration or reabsorption dominates.
Blood Hydrostatic Pressure (BHP)
- BHP is the pressure exerted by blood against the capillary walls.
- BHP drives filtration from the capillaries into the interstitial fluid.
- BHP drops from the arterial end (~35 mmHg) to the venous end (~16 mmHg) of the capillary.
Interstitial Fluid Hydrostatic Pressure (IFHP)
- IFHP is the pressure exerted by the interstitial fluid against the outside of the capillary walls.
- IFHP is typically low (close to zero mmHg), minimally opposing filtration.
Interstitial Fluid Osmotic Pressure (IFOP)
- IFOP is created by proteins in the interstitial fluid that can't cross the capillary walls.
- IFOP draws water out of capillaries and contributes to filtration.
- IFOP is typically in the range of 0.1 to 5 mmHg.
Blood Colloid Osmotic Pressure (BCOP)
- BCOP is caused by proteins (mainly albumin) in the plasma that are too large to cross capillary walls.
- BCOP draws water back into capillaries, promoting reabsorption.
- BCOP does not contribute to filtration.
Net Filtration Pressure (NFP) and Fluid Movement
-
Net Filtration Pressure (NFP) determines the movement of fluid between capillaries and the surrounding interstitial fluid.
-
Positive NFP indicates filtration, where fluid is moving out of the capillary and into the interstitial fluid.
-
Negative NFP indicates reabsorption, where fluid is moving into the capillary from the interstitial fluid.
-
Factors influencing NFP:
- Blood Hydrostatic Pressure (BHP): The force exerted by blood against the capillary walls.
- Interstitial Fluid Hydrostatic Pressure (IFHP): The force exerted by interstitial fluid against the capillary walls.
- Blood Colloid Osmotic Pressure (BCOP): The pressure exerted by plasma proteins in the blood attracting fluid into the capillary.
- Interstitial Fluid Osmotic Pressure (IFOP): The pressure exerted by proteins in the interstitial fluid attracting fluid out of the capillary.
-
NFP Formula: NFP = (BHP + IFOP) - (BCOP + IFHP)
-
Arterial End of Capillary: Typically has a positive NFP, where filtration occurs.
-
Venous End of Capillary: Typically has a negative NFP, where reabsorption occurs.
Starling's Law and Fluid Balance
-
Starling's Law describes the balance of hydrostatic and osmotic pressures that govern fluid movement across capillary walls.
-
85% of the fluid filtered out of capillaries is reabsorbed back into the bloodstream.
-
Approximately 20 liters of fluid are filtered out of capillaries into surrounding tissues each day.
-
17 liters are reabsorbed back into the capillaries leaving 3 liters in the interstitial space.
-
The remaining 3 liters enter the lymphatic system.
The Lymphatic System
- The lymphatic system plays a crucial role in preventing fluid accumulation in tissues by collecting excess fluid and returning it to the bloodstream.
Edema
-
Edema is swelling due to excess fluid accumulation in the interstitial spaces.
-
Edema can be caused by:
- Increased blood pressure
- Low blood protein levels
- Blockages in the lymphatic system.
Venules Function
- Venules collect blood from capillaries, forming the start of the venous system.
- They are vital for returning deoxygenated blood back to the heart.
Postcapillary Venules
- Smallest venules, measuring 10–50 µm in diameter.
- Highly porous and participate in exchange processes with surrounding tissues.
- This exchange includes fluids, nutrients, and waste products.
Larger Venules
- Increase in diameter to 50–200 µm.
- Decrease in permeability due to thicker walls with more smooth muscle.
- They lose the ability to participate in exchange processes as they grow larger.
Venule Structure
- Elastic walls make them act as a blood reservoir.
- This allows them to adjust blood flow and volume in response to changing needs.
- For instance, during physical activity, venules expand to hold more blood.
Veins
- Veins are blood vessels that carry deoxygenated blood back to the heart.
- The diameter of veins ranges from 0.5 mm to 3 cm.
- Veins have thinner walls than arteries because they operate under lower pressure.
- The thickest layer in veins is the tunica externa.
- Veins have a larger lumen compared to arteries, which allows them to distend easily and hold varying volumes of blood.
- Veins are more numerous than arteries in the body to facilitate the return of blood from tissues to the heart.
- Veins cannot withstand high pressure due to their larger lumen and thinner walls.
Differences between Veins and Arteries
- Veins lack internal and external elastic laminae, which are present in arteries.
- Veins have thinner walls and a larger lumen than arteries.
- Veins have a less developed tunica media (middle layer) compared to arteries.
- Veins have a thinner tunica interna (inner layer) compared to arteries.
Veins as Capacitance Vessels
- Veins are known as capacitance vessels because they can accommodate large volumes of blood, acting as blood reservoirs.
- Approximately 65% of the body's blood volume is held in veins at any given time.
- Veins operate under low pressure, which reduces the risk of bursting.
Structural Features of Veins
- Veins have a large lumen which creates little resistance to blood flow, aiding in the return of blood to the heart.
- Venous valves are primarily found in veins in the limbs.
- These valves are formed from the tunica intima layer of the vein wall.
Function of Venous Valves
- Venous valves function to prevent backflow of blood and ensure one-way flow toward the heart.
Varicose Veins Causes
- Varicose veins result from faulty valves within veins, causing blood to pool in the affected area.
Varicose Veins Location
-
Lower limbs are the most common sites for varicose veins.
-
Prolonged standing or sitting significantly increases venous pressure in the lower limbs, promoting varicose vein formation.
Varicose Veins Risk Factors
-
Varicose veins can be hereditary.
-
Prolonged standing, obesity, and pregnancy are major risk factors.
-
Increased abdominal pressure from obesity and pregnancy contributes to varicose vein development.
-
Low venous pressure is not a risk factor for varicose veins.
Varicose Veins Type
- Varicose veins primarily affect superficial veins.
Varicose Veins Prevalence
- More than 15% of adults experience varicose veins.
Varicose Veins Complications
- Increased pressure caused by straining during bowel movements or childbirth can lead to hemorrhoids, a condition similar to varicose veins in the anal area.
Blood Flow in Veins
-
When both the proximal and distal valves in a vein are open, blood flows upward through the vein.
-
Contraction of skeletal muscles surrounding a vein compresses the vein, forcing blood upward and closing the distal valve.
-
The distal valve closes during muscle contraction to prevent backflow of blood.
-
When the muscle relaxes, the proximal valve closes to prevent blood from flowing backward.
-
During muscle relaxation, the distal valve opens, allowing blood to fill the vein from below.
The Skeletal Muscle Pump
-
The skeletal muscle pump is a mechanism that ensures blood flows only toward the heart and prevents backflow.
-
This pump is particularly important for promoting blood flow in the lower limbs.
Respiratory Pump
- The respiratory pump is a mechanism that aids blood flow by relying on pressure changes in the thoracic and abdominal cavities.
- Inhalation:
- The diaphragm moves downward, decreasing pressure in the thoracic cavity.
- This decreased thoracic pressure draws air into the lungs.
- The increased abdominal pressure during inhalation pushes blood from the abdominal veins to the thoracic veins, aiding blood flow towards the heart.
- Exhalation:
- The diaphragm relaxes, and pressure in the thoracic and abdominal cavities equalizes.
- The venous valves prevent blood from flowing backward during exhalation.
- The primary role of the respiratory pump is to help move blood toward the heart by using pressure changes during breathing.
Blood Flow Definition
- Blood flow is the volume of blood moving through any tissue per minute.
Cardiac Output (CO)
- Cardiac output is the amount of blood pumped by the heart per minute.
- CO is calculated using the formula: CO = Heart Rate (HR) × Stroke Volume (SV)
- If a person's HR is 70 beats per minute and SV is 70 mL per beat, their CO is 4900 mL/min (70 x 70 = 4900).
Cardiac Output Distribution
- The distribution of CO depends primarily on blood pressure and vascular resistance
Blood Pressure
- Blood pressure drives blood through vessels
Vascular Resistance
- Vascular resistance opposes blood flow
- Blood viscosity influences vascular resistance
- Vascular resistance is influenced by vessel diameter, blood viscosity, and vessel length
Blood Pressure and Circulation
- Blood flows from areas of high pressure to low pressure.
- Contraction of the left ventricle generates blood pressure in the circulatory system.
- Blood pressure is highest in the aorta and large arteries.
- Systolic blood pressure occurs during ventricular contraction (systole).
- Diastolic blood pressure represents the lowest arterial pressure during heart relaxation.
- Blood pressure drops significantly in arterioles due to increased resistance.
- Blood pressure is near zero by the time blood reaches the vena cavae.
- Blood pressure decreases as it moves further from the heart because of resistance in smaller blood vessels and the distance from the pumping source.
Mean Arterial Pressure (MAP)
- MAP is the average pressure in the arteries throughout one cardiac cycle (systole and diastole).
- It's a better indicator of organ perfusion than systolic or diastolic pressure because it reflects the sustained pressure pushing blood through organs and tissues.
MAP Calculation
- Formula: MAP = SBP + (2 × DBP) ÷ 3
- Example: With a blood pressure of 120/80 mmHg, the MAP is approximately 90 mmHg.
MAP and Organ Perfusion
- A minimum MAP of 60 mmHg is generally required for adequate perfusion of vital organs.
Factors Affecting MAP
- Higher cardiac output: Increases MAP by increasing blood pressure.
- Vascular resistance: Influenced by vessel diameter and elasticity.
Normal MAP Range
- Normal values typically range between 65 and 110 mmHg.
Vascular Resistance
- Luminal Size & Resistance: Smaller luminal diameter increases vascular resistance, while larger diameter decreases it. This occurs due to increased friction between blood and vessel walls in narrower vessels.
- Vasoconstriction: Narrows blood vessels, increasing resistance.
- Vasodilation: Widens blood vessels, decreasing resistance.
- Blood Viscosity & Resistance: Higher blood viscosity (thickness) increases resistance. This is primarily influenced by the proportion of red blood cells (hematocrit).
- Dehydration & Resistance: Dehydration increases blood viscosity, leading to increased resistance.
- Blood Vessel Length & Resistance: Longer vessels increase resistance due to increased surface area for friction between blood and vessel walls.
- Obesity & Resistance: Obesity increases total blood vessel length, leading to increased vascular resistance.
Blood Flow Velocity and Circulation Time
- Inverse Relationship: Blood flow velocity is inversely proportional to the cross-sectional area of blood vessels. This means as the cross-sectional area increases, blood flow velocity decreases, and vice versa.
- Slowest in Capillaries: Blood flow velocity is slowest in capillaries, which are the smallest blood vessels. This slow flow allows sufficient time for nutrient and gas exchange between blood and tissues.
- Fastest in Aorta: Blood flow velocity is fastest in large arteries like the aorta, which have a large cross-sectional area.
- Increased Velocity in Veins: Blood flow velocity increases as blood moves back towards the heart through larger veins because the cross-sectional area decreases.
- Circulation Time: Defined as the time taken for a drop of blood to travel from the right atrium through the pulmonary and systemic circuits and return to the right atrium.
- Circulation Time in Healthy Adults: Approximately 1 minute.
Blood Vessel Cross-Sectional Area and Blood Flow Velocity
- Cross-sectional area is smallest in the aorta and large arteries.
- Cross-sectional area is largest in capillaries. This is because of the vast network of capillaries, creating a large total cross-sectional area.
- Blood flow velocity is highest in the aorta and large arteries due to the smallest cross-sectional area.
- Blood flow velocity reaches its lowest point in the capillaries because of the large cross-sectional area.
- As blood passes through the capillaries and moves through venules and veins, the velocity increases due to the decreasing cross-sectional area.
Heart Rate and Blood Pressure
- An increase in heart rate leads to an increase in blood pressure.
Stroke Volume
- Stroke volume refers to the volume of blood pumped by the heart per beat.
Systemic Vascular Resistance
- The primary factor influencing systemic vascular resistance (SVR) is the diameter of blood vessels.
Vasoconstriction and Blood Pressure
- Vasoconstriction (narrowing of blood vessels) causes an increase in blood pressure.
Blood Volume and Blood Pressure
- An increase in blood volume results in an increase in blood pressure.
Regulation of Blood Pressure
- Rapid changes in blood pressure are primarily regulated by adjustments in heart rate and blood vessel diameter.
- Long-term regulation of blood pressure through blood volume control is managed by the kidneys.
Factors that Lower Blood Pressure
- Decreasing blood volume is likely to lower blood pressure.
Heart Rate and Blood Pressure
- An increase in heart rate leads to an increase in blood pressure.
Stroke Volume
- Stroke volume represents the amount of blood pumped by the heart with each beat.
Systemic Vascular Resistance
- The diameter of blood vessels is the primary influencer of systemic vascular resistance.
Vasoconstriction
- Vasoconstriction, the narrowing of blood vessels, leads to an increase in blood pressure.
Blood Volume and Blood Pressure
- Increased blood volume results in elevated blood pressure.
Blood Pressure Regulation
- The body utilizes feedback mechanisms to quickly adjust blood pressure through changes in heart rate and blood vessel diameter.
- Long-term blood pressure regulation is primarily managed by the kidneys through the control of blood volume.
Factors that Lower Blood Pressure
- Decreased blood volume can lower blood pressure.
Cardiovascular Center (CVC)
- CVC regulates heart rate and stroke volume, which directly impact cardiac output and blood pressure.
- CVC coordinates neural, hormonal, and local feedback systems to regulate blood flow and blood pressure.
- Specific groups of neurons within the CVC control heart rate, contractility, and blood vessel diameter.
- The vasomotor center in the CVC adjusts blood vessel diameter.
- Cardiostimulatory responses from the CVC increase heart rate and contractility.
- The cardioinhibitory response of the CVC lowers heart rate and contractility.
- The CVC can adjust cardiovascular responses to changing conditions to maintain homeostasis.
Brain Regions and Cardiovascular Control
- Cerebral cortex provides input to the Cardiovascular Control Center (CVC) based on conscious thoughts, impacting cardiovascular responses during stress or relaxation.
- Limbic system plays a critical role in the CVC by governing emotions that influence heart rate and blood pressure.
- Hypothalamus acts as a key regulator of homeostasis, impacting the CVC based on physiological needs like body temperature and hydration.
Sensory Receptors and the CVC
- Baroreceptors detect changes in blood pressure, providing feedback to the CVC.
- Chemoreceptors send signals to the CVC based on changes in oxygen, carbon dioxide, and pH levels in the blood.
- Proprioceptors sense body position and movement, providing input to the CVC during physical activity.
- All of the above sensory receptors (proprioceptors, chemoreceptors, and baroreceptors) help the CVC respond to immediate physiological changes in the body.
Parasympathetic Nervous System
- The parasympathetic nervous system influences the heart through the vagus nerve.
- This pathway has an inhibitory effect, slowing down heart rate.
- As a result, the parasympathetic nervous system also reduces both cardiac output and blood pressure.
Sympathetic Nervous System
- The sympathetic nervous system sends signals to the heart through the cardiac accelerator nerves.
- The cardiac accelerator nerves increase both heart rate and force of contraction.
- Vasomotor nerves are a part of the sympathetic nervous system.
- Vasomotor nerves increase blood pressure by causing vasoconstriction.
- The sympathetic nervous system overall increases blood pressure by boosting both cardiac output and vascular resistance.
Baroreceptors
- Detect changes in blood pressure.
- Located in the carotid arteries and aorta.
- When blood pressure rises, baroreceptors signal the cardiovascular center (CVC) to lower heart rate and dilate blood vessels.
Chemoreceptors
- Monitor oxygen, carbon dioxide, and pH levels in the blood.
- Located primarily in the carotid and aortic bodies.
- When blood oxygen levels are low, chemoreceptors increase heart rate and respiration rate.
Proprioceptors
- Provide information on body position and movement.
- During physical activity, proprioceptors signal the CVC to increase blood flow to the muscles to meet their demand for oxygen and nutrients.
The Carotid Sinus
- Located within the left and right carotid arteries.
- The carotid sinus reflex is a mechanism that helps maintain a stable blood flow to the brain by responding to blood pressure changes.
- The sensory impulses from the carotid sinus baroreceptors are transmitted to the Cardiovascular Center (CVC) via the glossopharyngeal nerve (cranial nerve IX).
- When blood pressure increases in the carotid sinus, the baroreceptors send signals to the CVC, triggering a decrease in heart rate and adjusting blood vessel diameter.
The Aortic Reflex
- The aortic reflex involves baroreceptors situated in the aortic arch and ascending aorta.
- These baroreceptors send signals to the CVC via the vagus nerve (cranial nerve X).
- The primary role of the aortic reflex is to regulate systemic blood pressure, ensuring stable blood flow throughout the body.
Shared Functions of the Carotid Sinus and Aortic Reflexes
- Both reflexes are crucial in maintaining stable blood pressure and blood flow throughout the body.
Blood Pressure Regulation
-
Baroreceptors are pressure-sensitive receptors located in the walls of the carotid arteries and the aorta. They detect changes in blood pressure and send signals to the cardiovascular center (CVC) in the brainstem.
-
When blood pressure falls, baroreceptors generate fewer impulses to the CVC. This triggers a series of physiological responses to increase blood pressure.
-
CVC increases sympathetic stimulation in response to low blood pressure. This leads to increased heart rate, vasoconstriction (narrowing of blood vessels), and increased cardiac output.
-
Vasoconstriction increases vascular resistance, further contributing to higher blood pressure.
-
When blood pressure rises, baroreceptors generate more frequent impulses to the CVC. This activates the parasympathetic nervous system.
-
The CVC increases parasympathetic activity in response to high blood pressure, resulting in decreased heart rate and cardiac output.
-
Vasodilation (widening of blood vessels) occurs, reducing vascular resistance and lowering blood pressure.
Chemoreceptors
- Detect changes in oxygen (O₂), hydrogen ions (H⁺), and carbon dioxide (CO₂) levels in the blood
- Located near baroreceptors in carotid bodies and aortic bodies
- Respond to low oxygen levels (hypoxia), high hydrogen ion concentrations (acidosis), and elevated carbon dioxide levels (hypercapnia)
- Send impulses to the Cardiovascular Center (CVC) in response to these changes
- Trigger increased sympathetic stimulation, which causes vasoconstriction and increases blood pressure
Cardiovascular Center (CVC)
- Responsible for regulating heart rate and blood pressure
- Receives signals from chemoreceptors
- Increases sympathetic stimulation to respond to chemoreceptor activity
- Sympathetic stimulation leads to vasoconstriction and increased blood pressure
Blood Chemistry and Homeostasis
- Hypoxia, Acidosis, and Hypercapnia: These conditions signal a disruption in blood gas levels and pH.
- Hypoxia: Low oxygen levels in the blood.
- Acidosis: Increased acidity (lower pH) in the blood.
- Hypercapnia: Elevated carbon dioxide levels in the blood.
- Chemoreceptors: Specialized cells located in the carotid and aortic bodies that detect changes in blood chemistry.
- Carotid Bodies: Located near the carotid arteries in the neck.
- Aortic Bodies: Located in the aortic arch.
- Vasomotor Center: A region in the brainstem that controls blood vessel diameter.
- Chemoreceptor Signals: Chemoreceptors send signals to the vasomotor center when they detect hypoxia, acidosis, or hypercapnia.
- Vasomotor Center Response: Activates vasoconstriction, increasing heart rate and cardiac output.
- Vasoconstriction: Narrowing of blood vessels.
- Effect on Blood Flow: Increases vascular resistance, redirecting blood flow to vital organs.
- Combined Effects: Increased heart rate, cardiac output, and vasoconstriction collectively lead to increased blood pressure.
- Increased Blood Pressure: Helps speed the return of blood to the heart and lungs for oxygen uptake and carbon dioxide removal.
- Overall Purpose: The body's response aims to restore normal blood gas levels and pH.
The Renin-Angiotensin-Aldosterone (RAA) System
- The RAA system is triggered when blood flow to the kidneys is reduced
Role of Renin
- Renin converts angiotensinogen to angiotensin I, a key step in the RAA system
Angiotensin I to Angiotensin II
- Angiotensin I is converted to angiotensin II by ACE (Angiotensin-Converting Enzyme)
Primary Effects of Angiotensin II
- Angiotensin II causes vasoconstriction, constricting blood vessels to increase blood pressure
- Angiotensin II stimulates the release of aldosterone
Aldosterone and Blood Pressure
- Aldosterone promotes reabsorption of sodium and water in the kidneys, increasing blood volume and therefore blood pressure
Fight or Flight Response
- Epinephrine and norepinephrine are released during "fight or flight" response triggered by sympathetic stimulation.
- These hormones prepare the body for stressful situations, enhancing blood flow to muscles and vital organs to support increased physical activity
- They increase blood pressure by:
- Increasing cardiac output, how much blood your heart pumps per minute
- Causing vasoconstriction, constricting blood vessels to increase blood pressure
Antidiuretic Hormone
- Antidiuretic Hormone (ADH) is produced in the hypothalamus
- ADH release is triggered by low blood volume or high blood osmolarity
- ADH elevates blood pressure by causing vasoconstriction and increasing water reabsorption
- ADH acts on the kidneys to promote water reabsorption
Atrial Natriuretic Peptide
- Atrial Natriuretic Peptide (ANP) is released in response to high blood volume and stretching of the atrial walls
- ANP has a vasodilation effect on blood vessels
- ANP reduces blood volume by promoting sodium and water excretion in the kidneys
- The primary role of ANP in blood pressure regulation is to lower blood pressure by reducing blood volume and promoting vasodilation.
Autoregulation of Blood Flow
- Autoregulation is the ability of tissues to control their own blood flow to meet metabolic needs.
- The process is primarily regulated by local factors within the tissue, such as changes in oxygen levels, carbon dioxide levels, and metabolic byproducts.
- Vasodilation increases blood flow to tissues that need more nutrients or oxygen, and vasoconstriction reduces blood flow to tissues that are not actively using them.
Mechanisms of Autoregulation:
- Myogenic Response: Smooth muscle in blood vessel walls senses changes in blood pressure.
- Increased blood pressure triggers vasoconstriction to protect capillaries.
- Chemical Factors:
- Nitric Oxide (NO): Released by endothelial cells, a potent vasodilator.
- Endothelins: Released by endothelial cells, act as vasoconstrictors.
Importance of Autoregulation
- Autoregulation ensures blood flow meets the needs of active tissues and organs.
- It is essential for maintaining proper tissue function and oxygenation, particularly during exercise or other situations where blood flow demands change.
Blood Volume and Cardiac Output
- Increased blood volume leads to higher venous return and cardiac output (CO)
- Increased sympathetic impulses from the adrenal medulla result in a higher heart rate (HR) and stroke volume (SV)
Factors Affecting Venous Return
- The skeletal muscle pump, respiratory pump, and venoconstriction all increase venous return
- These mechanisms contribute to elevated mean arterial pressure (MAP)
Systemic Vascular Resistance (SVR)
- Increased blood viscosity, as seen in polycythemia, increases SVR
- Obesity increases SVR by lengthening the vascular network
- Vasoconstriction increases SVR, contributing to a higher MAP
Regulation of Mean Arterial Pressure (MAP)
- A significant rise in MAP results from increased cardiac output (CO) and SVR
- The primary goal of regulating MAP is to maintain adequate blood flow and pressure throughout the body
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.