Podcast
Questions and Answers
What is the primary reason for the reduction in stiffness and strength of connective tissue in old age?
What is the primary reason for the reduction in stiffness and strength of connective tissue in old age?
- Enhanced fibroblast metabolism and remodeling ability
- Increased collagen content in connective tissues
- Decreased activity and inactivity rather than aging itself (correct)
- Natural aging process without influence from activity levels
Which type of cartilage is characterized as the weakest among the three types mentioned?
Which type of cartilage is characterized as the weakest among the three types mentioned?
- Dense connective tissue
- Articular (hyaline) cartilage (correct)
- Elastic cartilage
- Fibrocartilage
In which type of connective tissue are chondrocytes sparse and may be found in groups called lacunae?
In which type of connective tissue are chondrocytes sparse and may be found in groups called lacunae?
- Fibrocartilage
- Elastic cartilage
- Articular cartilage (correct)
- Dense connective tissue
What is a unique characteristic of articular cartilage compared to other types of cartilage?
What is a unique characteristic of articular cartilage compared to other types of cartilage?
Which statement about the adaptive shortening of connective tissue structures is true?
Which statement about the adaptive shortening of connective tissue structures is true?
What characterizes an open fracture?
What characterizes an open fracture?
During which phase of fracture healing does angiogenesis primarily occur?
During which phase of fracture healing does angiogenesis primarily occur?
Which cells migrate to the hematoma during the initial healing phase?
Which cells migrate to the hematoma during the initial healing phase?
In which phase does the formation of fibrocartilaginous tissue occur?
In which phase does the formation of fibrocartilaginous tissue occur?
What is the result of a stress injury if not adequately addressed?
What is the result of a stress injury if not adequately addressed?
What is the consequence of reduced compression on bone health?
What is the consequence of reduced compression on bone health?
Which of the following statements accurately describes osteopenia?
Which of the following statements accurately describes osteopenia?
What happens to bone during the unloading phase following a fracture?
What happens to bone during the unloading phase following a fracture?
What is the primary role of articular cartilage?
What is the primary role of articular cartilage?
Which zone of articular cartilage contains the highest concentration of proteoglycans?
Which zone of articular cartilage contains the highest concentration of proteoglycans?
How does bone remodeling respond to weight-bearing activity?
How does bone remodeling respond to weight-bearing activity?
What consequence results from reduced loading of the articular cartilage?
What consequence results from reduced loading of the articular cartilage?
What primarily influences the remodeling of bone architecture?
What primarily influences the remodeling of bone architecture?
How does aging affect articular cartilage?
How does aging affect articular cartilage?
In the event of excessive loading, what is a common outcome for articular cartilage?
In the event of excessive loading, what is a common outcome for articular cartilage?
What mechanism provides nutrition to the articular cartilage?
What mechanism provides nutrition to the articular cartilage?
What effect does impact loading have on articular cartilage?
What effect does impact loading have on articular cartilage?
Which type of tissue is included in the types of periarticular connective tissue?
Which type of tissue is included in the types of periarticular connective tissue?
What biological response is triggered by the loading of tendons?
What biological response is triggered by the loading of tendons?
What effect does underloading have on tendons?
What effect does underloading have on tendons?
Which type of tissue primarily composes the outer layer of the joint capsule?
Which type of tissue primarily composes the outer layer of the joint capsule?
What is the primary function of ligaments?
What is the primary function of ligaments?
What type of collagen is predominantly found in tendons?
What type of collagen is predominantly found in tendons?
What is a common cause of dense connective tissue injury?
What is a common cause of dense connective tissue injury?
What occurs during the Remodeling Phase of soft tissue healing?
What occurs during the Remodeling Phase of soft tissue healing?
What is the possible outcome of prolonged immobilization on connective tissues?
What is the possible outcome of prolonged immobilization on connective tissues?
What is the main role of fibroblasts during the Proliferative Phase of healing?
What is the main role of fibroblasts during the Proliferative Phase of healing?
What happens to collagen synthesis and degradation over time during the healing process?
What happens to collagen synthesis and degradation over time during the healing process?
What is the primary effect of applying heat to soft tissues?
What is the primary effect of applying heat to soft tissues?
Which type of ligaments are oriented to resist multidirectional forces?
Which type of ligaments are oriented to resist multidirectional forces?
What happens to mechanically induced tissue stress during early healing phases?
What happens to mechanically induced tissue stress during early healing phases?
What typically occurs when the rate of loading on a ligament is high?
What typically occurs when the rate of loading on a ligament is high?
Flashcards are hidden until you start studying
Study Notes
Tendon Mechanobiology
- Tendons are living tissues that respond to loading changes by undergoing remodeling.
- Tenocytes are affected by shear and compression forces during loading.
- Underloading (rest/immobilization) decreases tendon stiffness and collagen production.
- Excessive overload with inadequate recovery leads to tendon injury.
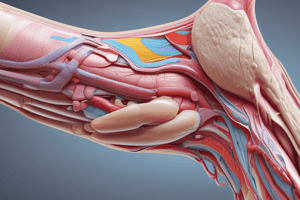
Joint Capsule
- Surrounds and encloses a joint.
- Has a fibrous (outer) and synovial (inner) layer.
- Mechanosensitive and adapts to different loading demands.
- Primarily consists of Type I collagen, but composition varies depending on joint.
Function of Joint Capsule
- Maintains the intra-articular environment of the joint.
- Provides joint stability, sometimes thickened in specific areas to form capsular ligaments.
- Provides proprioceptive feedback.
- Produces synovial fluid for lubrication and joint nutrient supply.
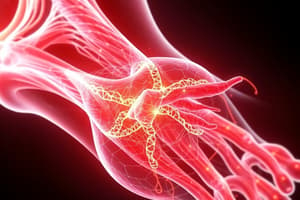
Ligaments
- Connect bone to bone.
- Similar hierarchical structure to tendons, but collagen fibers are not always parallel.
- Contain less collagen, but more elastin and proteoglycans compared to tendons.
- More metabolically active than tendons.
Types of Ligaments
- Capsular Ligaments: Thickenings of the joint capsule that resist multi-directional forces.
- Intra- or Extra-capsular Ligaments: More rope-like, typically resist one or two forces.
Function of Ligaments
- Resist excessive joint motion.
- Guide joint motion.
- Provide proprioceptive feedback.
Dense Connective Tissue Injury
- Overuse: Repetitive microtrauma leading to gradual damage (degeneration).
- Acute: Stress exceeding the structure's failure point, potentially preceded by degeneration.
- Can be complete or partial ruptures.
Overuse Dense Connective Tissue Injury
- Load tolerance is a balance between collagen degradation and synthesis.
- Repeated overload with inadequate recovery reduces load tolerance, increasing injury risk.
Rate of Force Application
- Force application speed influences injury type.
- High rate of loading can cause rupture.
- Lower rate of loading can result in avulsion.
Soft Tissue Healing Phases
- Hemostasis (Bleeding) (Seconds to Hours)
- Vasoconstriction to slow bleeding.
- Platelet aggregation forms an immature clot.
- Fibrin reinforces the clot.
- Inflammatory Phase (Hours to Days)
- Pro-inflammatory chemicals trigger the inflammatory response.
- Neutrophils and macrophages remove bacteria, foreign materials, and damaged cells.
- Proliferative (Repair) Phase (Days to Weeks)
- Fibroblasts produce extracellular matrix and disorganized collagen fibers (Type III) forming granulation tissue.
- Angiogenesis (formation of new blood vessels) occurs.
- Remodeling Phase (Weeks to >1 Year)
- Weak, disorganized Type III collagen (scar tissue) is replaced by stronger Type I collagen.
- Collagen fibers align to stresses placed on the tissue.
- Scar tissue contraction can limit joint motion if not mobilized.
Importance of Mechanical Stress During Healing
- Moderate stress encourages organized collagen alignment in the direction of forces.
- Minimizes scar tissue contraction.
- Early joint movement provides sufficient stress for healing.
Effects of Temperature
- Increased temperature increases stress relaxation and creep.
- Heated tissues require less time to reach a given strain when stretched.
Response to Prolonged Immobilization
- Reduced tensile strength: Can take 12 to 18 months to fully recover.
- Adaptive shortening of structures: Especially the joint capsule.
- Arthrofibrosis: Excessive collagen production and adhesion formation causing joint stiffness and pain.
Effects of Age and Aging
- Adolescents: Dense connective tissue is often stronger than bon, making avulsion fractures more likely than ruptures.
- Old Age: Degenerative changes, altered fibroblast metabolism, reduced stiffness, strength and collagen content.
- Decreased activity appears to contribute to these changes, rather than age itself.
Types of Periarticular Connective Tissues
- Dense Connective Tissue: Joint capsule, ligaments, and tendons.
- Articular Cartilage: Specialized hyaline cartilage covering joint surfaces.
- Fibrocartilage: Found in intervertebral discs, pubic symphysis, and menisci.
Cartilage
- Strong and elastic connective tissue.
- Contains chondrocytes, collagen, and matrix.
- 70-85% water by weight.
- Avascular and aneural.
- Usually surrounded by perichondrium containing blood vessels and nerves for tissue maintenance.
Chondrocytes
- Mature cartilage cells that maintain the cartilaginous matrix.
- Sparsely distributed.
- Can occur in groups called Lacunae.
Types of Cartilage
- Articular (hyaline) Cartilage: Found on joint surfaces, reduces friction and absorbs shock.
- Fibrocartilage: Strongest type, found in intervertebral discs, pubic symphysis, and menisci.
- Elastic Cartilage: Found in external ear, arteries, and lung tissue.
Articular Cartilage
- Specialized hyaline cartilage on joint surfaces.
- Lacks a perichondrium.
- Chondrocytes are surrounded by Type II collagen.
Roles of Articular Cartilage
- Distributing and dispersing compressive forces.
- Reducing friction between joint surfaces, significantly more slippery than ice on ice.
Articular Cartilage Zones
- Superficial Tangential Zone (STZ): Collagen fibers parallel to the articular surface. Highest collagen, lowest proteoglycan content.
- Middle Zone: Oblique collagen fibers. Thickest layer, contains round chondrocytes.
- Deep Zone: Perpendicular collagen fibers. Highest concentration of proteoglycans.
- Calcified Zone: Anchors cartilage to bone.
- Tidemark: Separates the calcified zone from subchondral bone, acts as a diffusion barrier between cartilage and bone.
Articular Cartilage Nutrition
- Nutrition is supplied by diffusion.
- Intermittent joint loading deforms the articular surface, "washing" synovial fluid in and out of cartilage.
- Synovial fluid also lubricates cartilage.
Response to Reduced Loading
- Reduced nutrition and lubrication can lead to degenerative changes.
Response to Immobilization/Unloading
- Reduced cartilage thickness, chondrocyte density, and collagen content.
- Cartilage becomes softer and weaker.
Response to Excessive Loading (Injury)
- Damage to collagen fiber network (fibrillation) causes roughness.
- Loss of proteoglycans decreases fluid content.
- Reduced stiffness.
- Impaired ability to respond to compressive and shear forces.
Response to Impact Loading
- Occurs when loads are applied rapidly.
- Cartilage stiffens, unable to deform and redistribute loads quickly.
Effect of Aging on Cartilage
- Imbalance between breakdown and repair processes.
- Reduced thickness, increased calcification, and cross-linking.
- Increased stiffness and susceptibility to fatigue failure.
- Reduced chondrocyte density.
Types of Periarticular Connective Tissues
- Dense Connective Tissue: Covers joint capsule, ligaments, and tendons.
- Articular Cartilage: Specialized tissue covering load-bearing joint surfaces.
- Weight-bearing long bones vs. flat bones: Different structural characteristics and functions.
Fractures
- Classified based on location, severity, and shape.
- Open Fracture: Bone penetrates the skin.
- Closed Fracture: Skin remains intact.
- Displaced Fracture: Bone fragments shift out of alignment.
- Stress Injury: Repetitive overload with inadequate recovery. Can progress into a stress fracture.
Fracture Healing Phases
- 1. Formation of Hematoma (Days 1-5): Blood vessels tear, forming a clot which acts as a framework for repair. Neutrophils, macrophages, and osteoclasts remove damaged tissue.
- 2. Fibrocartilaginous Callus Formation (Days 5-11): Angiogenesis occurs, and a fibrin-rich granulation tissue bridges the fracture gap. Mesenchymal stem cells differentiate into fibroblasts, chondroblasts, and osteoblasts.
- 3. Bony Callus Formation (Days 11-28): Ossification of callus occurs, along with continued bone deposition under the periosteal surface.
- 4. Bone Remodeling (Day 18+): Bone is remodeled by osteoclast absorption and osteoblast deposition. This process can last months to years.
Response to Loading (Fracture Repair)
- Compression loads promote stronger bone growth in the direction of the force.
- Weight-bearing during the remodeling stage is essential for healing.
- Reduced compression due to lack of weight bearing results in weaker bone.
Response to Unloading
- Reduced compression and tensile strain from lack of weight bearing and muscle force.
- Less bone deposition, weaker bone.
- Greater impact on weight-bearing bones.
Effects of Aging on Bone
- Resorption exceeds deposition.
- Reduced bone mass and density.
- Bone stiffens (becomes brittle).
- Mechanically weaker.
- Changes can be mitigated with activity levels that promote muscle force and weight bearing load.
Osteopenia and Osteoporosis
- Resorption significantly outweighs deposition.
- Calcium depletion occurs.
- Estrogen and testosterone levels are reduced.
- Osteopenia: Reduced bone mineral density.
- Osteoporosis: Bone mineral density is 2.5 standard deviations below normal.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.