Podcast
Questions and Answers
What is the primary role of the superior head of the lateral pterygoid muscle?
What is the primary role of the superior head of the lateral pterygoid muscle?
- Facilitates contralateral excursion
- Active during lateral movements of the mandible
- Responsible for closing the jaw (correct)
- Aids in jaw depression
Which nerve provides motor innervation to the anterior belly of the digastric muscle?
Which nerve provides motor innervation to the anterior belly of the digastric muscle?
- Masseteric nerve
- Auriculotemporal nerve
- Deep temporal nerve
- Mandibular division of the trigeminal nerve (correct)
What is the main function of the buccinator muscle during chewing?
What is the main function of the buccinator muscle during chewing?
- Positions the cheek (correct)
- Facilitates jaw opening
- Aids in tongue movement
- Raises the mandible
What is the average rotation range of the condyle during mandibular motion?
What is the average rotation range of the condyle during mandibular motion?
Which artery bifurcates at the level of the condyle to supply the muscles of mastication?
Which artery bifurcates at the level of the condyle to supply the muscles of mastication?
What is the purpose of the jaw jerk reflex?
What is the purpose of the jaw jerk reflex?
What condition is considered a possible cause of disc displacements in the temporomandibular joint?
What condition is considered a possible cause of disc displacements in the temporomandibular joint?
During maximum opening of the jaw, what is the average distance achieved?
During maximum opening of the jaw, what is the average distance achieved?
What is a commonly considered factor in the development of intra-articular disorders?
What is a commonly considered factor in the development of intra-articular disorders?
Which clinical test is most widely used for assessing temporomandibular disorders (TMD)?
Which clinical test is most widely used for assessing temporomandibular disorders (TMD)?
What symptom is most commonly associated with TMD?
What symptom is most commonly associated with TMD?
What could cause acute closed lock of the jaw?
What could cause acute closed lock of the jaw?
Which factor is NOT listed as a contributing etiology of TMD?
Which factor is NOT listed as a contributing etiology of TMD?
What demographic is most affected by TMD?
What demographic is most affected by TMD?
What is one of the indicators for expert psychological evaluation in TMD patients?
What is one of the indicators for expert psychological evaluation in TMD patients?
Which of the following is NOT a procedure for assessing mandibular range of motion?
Which of the following is NOT a procedure for assessing mandibular range of motion?
What structure connects the posterior band of the disc to the posterior slope of the condyle?
What structure connects the posterior band of the disc to the posterior slope of the condyle?
Which muscles are involved in producing the powerful forces required for chewing?
Which muscles are involved in producing the powerful forces required for chewing?
What is the primary function of the lateral pterygoid muscle?
What is the primary function of the lateral pterygoid muscle?
Which part of the temporalis muscle is responsible for elevating the mandible?
Which part of the temporalis muscle is responsible for elevating the mandible?
Where does the deep head of the masseter muscle originate?
Where does the deep head of the masseter muscle originate?
Which muscle is primarily involved in retracting the mandible?
Which muscle is primarily involved in retracting the mandible?
What is the role of the capsular ligament in relation to the temporomandibular joint?
What is the role of the capsular ligament in relation to the temporomandibular joint?
Which muscle does NOT elevate the mandible?
Which muscle does NOT elevate the mandible?
What type of joint is the temporomandibular joint (TMJ)?
What type of joint is the temporomandibular joint (TMJ)?
Which component primarily contributes to the normal mouth opening in the TMJ?
Which component primarily contributes to the normal mouth opening in the TMJ?
What type of tissue occupies the space behind the disc and the condyle in the TMJ?
What type of tissue occupies the space behind the disc and the condyle in the TMJ?
How is the articular disc of the TMJ characterized in terms of vascularization?
How is the articular disc of the TMJ characterized in terms of vascularization?
At what age does the S-shaped form of the fossa and eminence begin to develop?
At what age does the S-shaped form of the fossa and eminence begin to develop?
What is the anatomical term for the mass of soft tissue located behind the articular disc in the TMJ?
What is the anatomical term for the mass of soft tissue located behind the articular disc in the TMJ?
Which structures are involved in the management of temporomandibular disorders?
Which structures are involved in the management of temporomandibular disorders?
What is one of the possible etiological factors associated with TMJ pain dysfunction syndrome?
What is one of the possible etiological factors associated with TMJ pain dysfunction syndrome?
Which of the following is NOT a characteristic symptom of rheumatoid arthritis?
Which of the following is NOT a characteristic symptom of rheumatoid arthritis?
What is a common result of a blow to the chin?
What is a common result of a blow to the chin?
Which factor is a known risk for septic arthritis?
Which factor is a known risk for septic arthritis?
What is a feature distinguishing synovial chondromatosis?
What is a feature distinguishing synovial chondromatosis?
Which of the following conditions may present with trismus and deviation of the mandible?
Which of the following conditions may present with trismus and deviation of the mandible?
Which imaging technique is commonly used in the diagnosis of conditions affecting the TMJ?
Which imaging technique is commonly used in the diagnosis of conditions affecting the TMJ?
What is the primary treatment for chronic recurring dislocations of the temporomandibular joint?
What is the primary treatment for chronic recurring dislocations of the temporomandibular joint?
Which developmental disturbance involves the absence of the condyle?
Which developmental disturbance involves the absence of the condyle?
What is the primary goal of treatment for anterior disc displacement without reduction?
What is the primary goal of treatment for anterior disc displacement without reduction?
Which type of treatment modality does NOT belong to the category of physiotherapy?
Which type of treatment modality does NOT belong to the category of physiotherapy?
Which condition is characterized by the condyle slipping over the anterior rim of the disc?
Which condition is characterized by the condyle slipping over the anterior rim of the disc?
What is a common symptom of anterior disc displacement with reduction?
What is a common symptom of anterior disc displacement with reduction?
Which of the following is NOT typically a pharmacotherapy used in managing temporomandibular disorders?
Which of the following is NOT typically a pharmacotherapy used in managing temporomandibular disorders?
During which stage of articular disc disorders might there be intermittent locking of the jaw?
During which stage of articular disc disorders might there be intermittent locking of the jaw?
What treatment option could be used for posterior disc displacement?
What treatment option could be used for posterior disc displacement?
Which of the following is a characteristic of temporomandibular joint arthritis?
Which of the following is a characteristic of temporomandibular joint arthritis?
Flashcards
Describe the TMJ
Describe the TMJ
A bilateral synovial joint responsible for opening and closing the jaw. It's formed by the articulation of the temporal bone and mandibular condyle.
What are temporomandibular disorders?
What are temporomandibular disorders?
A collective term for issues affecting the masticatory muscles, TMJ, and associated structures
What is the articular disc in the TMJ?
What is the articular disc in the TMJ?
A fibrocartilage disc separating the condyle and fossa, allowing smooth joint movement.
What is the retrodiscal tissue?
What is the retrodiscal tissue?
Signup and view all the flashcards
What is a disc displacement in the TMJ?
What is a disc displacement in the TMJ?
Signup and view all the flashcards
What is the role of synovial fluid in the TMJ?
What is the role of synovial fluid in the TMJ?
Signup and view all the flashcards
What is TMJ pain dysfunction syndrome?
What is TMJ pain dysfunction syndrome?
Signup and view all the flashcards
How is a TMJ assessed?
How is a TMJ assessed?
Signup and view all the flashcards
Capsular Ligament
Capsular Ligament
Signup and view all the flashcards
Lateral Temporomandibular Ligament
Lateral Temporomandibular Ligament
Signup and view all the flashcards
Masseter Muscle
Masseter Muscle
Signup and view all the flashcards
Temporalis Muscle
Temporalis Muscle
Signup and view all the flashcards
Medial Pterygoid Muscle
Medial Pterygoid Muscle
Signup and view all the flashcards
Lateral Pterygoid Muscle
Lateral Pterygoid Muscle
Signup and view all the flashcards
Inferior Lamina
Inferior Lamina
Signup and view all the flashcards
Muscle of Mastication
Muscle of Mastication
Signup and view all the flashcards
Lateral Pterygoid Muscle Function
Lateral Pterygoid Muscle Function
Signup and view all the flashcards
Medial Pterygoid Muscle Function
Medial Pterygoid Muscle Function
Signup and view all the flashcards
Masseter Muscle Function
Masseter Muscle Function
Signup and view all the flashcards
Temporalis Muscle Function
Temporalis Muscle Function
Signup and view all the flashcards
Jaw Jerk Reflex
Jaw Jerk Reflex
Signup and view all the flashcards
Jaw Opening Reflex
Jaw Opening Reflex
Signup and view all the flashcards
Centric Relation
Centric Relation
Signup and view all the flashcards
Mandibular Range of Motion
Mandibular Range of Motion
Signup and view all the flashcards
Articular Disc Disorders of the TMJ
Articular Disc Disorders of the TMJ
Signup and view all the flashcards
Anterior Disc Displacement with Reduction (ADD with reduction)
Anterior Disc Displacement with Reduction (ADD with reduction)
Signup and view all the flashcards
Anterior Disc Displacement without Reduction (ADD without reduction)
Anterior Disc Displacement without Reduction (ADD without reduction)
Signup and view all the flashcards
Posterior Disc Displacement
Posterior Disc Displacement
Signup and view all the flashcards
Temporomandibular Joint Arthritis (TMJ Arthritis)
Temporomandibular Joint Arthritis (TMJ Arthritis)
Signup and view all the flashcards
Mandibular Fossa Angle
Mandibular Fossa Angle
Signup and view all the flashcards
Disc Adhesion in Fossa
Disc Adhesion in Fossa
Signup and view all the flashcards
Muscle Palpation for TMD
Muscle Palpation for TMD
Signup and view all the flashcards
Jaw Jerk Reflex and Silent Period
Jaw Jerk Reflex and Silent Period
Signup and view all the flashcards
TMJ Clicking
TMJ Clicking
Signup and view all the flashcards
Nerve Entrapment in TMD
Nerve Entrapment in TMD
Signup and view all the flashcards
Ear Symptoms and TMD
Ear Symptoms and TMD
Signup and view all the flashcards
TMD Etiology (Causes)
TMD Etiology (Causes)
Signup and view all the flashcards
What are the clinical signs of TMJ osteoarthritis?
What are the clinical signs of TMJ osteoarthritis?
Signup and view all the flashcards
What is TMJ osteoarthritis?
What is TMJ osteoarthritis?
Signup and view all the flashcards
What is synovial chondromatosis?
What is synovial chondromatosis?
Signup and view all the flashcards
What are the clinical signs of synovial chondromatosis?
What are the clinical signs of synovial chondromatosis?
Signup and view all the flashcards
What is septic arthritis of the TMJ?
What is septic arthritis of the TMJ?
Signup and view all the flashcards
What are the clinical signs of septic arthritis of the TMJ?
What are the clinical signs of septic arthritis of the TMJ?
Signup and view all the flashcards
What is condylar hyperplasia?
What is condylar hyperplasia?
Signup and view all the flashcards
Study Notes
Temporomandibular Joint (TMJ) Disorders
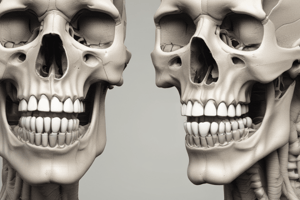
- The TMJ is a bilateral synovial joint formed by the articulation of the temporal bone and the mandibular condyle.
- Temporomandibular disorders (TMDs) encompass a range of problems involving the masticatory muscles, the temporomandibular joints, and associated structures.
Learning Outcomes
- Define the TMJ
- Classify TMJ diseases
- Assess TMJ
- Manage TMJ disorders
Functional Anatomy of the TMJ
- The TMJ exhibits hinge and gliding movements.
- The fossa and eminence develop fully by the second decade.
- Condylar rotation is more significant for mouth opening than translation.
- Synovial fluid facilitates lubrication (weeping lubrication).
- Fibrocartilage covers the articulating surfaces.
Articular Disc
- The articular disc is composed of dense collagen fibers.
- It fills the space between the fibrocartilage coverings of the condyle and mandibular fossa.
- The disc is primarily avascular and has limited sensory nerve innervation.
- The disc attaches to the medial and lateral aspects of the condyle
- The disc consists of anterior and posterior bands, thickest in the intermediate zone.
- Fibers from the temporalis, masseter, and lateral pterygoid muscles insert into the anterolateral and anteromedial two-thirds of the disc.
Retrodiscal Tissue
- Retrodiscal tissue is soft tissue positioned behind the disc and condyle, often referred to as the posterior attachment.
- A superior lamina connects the posterior band of the disc to the squamotympanic fissure and tympanic part of the temporal bone.
- An inferior lamina connects to the inferior margin of the posterior slope of the condyle.
TMJ Ligaments
- Capsular ligament
- Lateral temporomandibular ligament
- Sphenomandibular ligament
- Stylomandibular ligament
Muscles of Mastication
- Mandibular movements toward tooth contact are driven by masseter, temporalis, and medial pterygoid muscles.
- Masseter forms a sling that generates significant forces for chewing.
- The masseter muscle, with superficial and deep heads, elevates the mandible.
- Temporalis muscle has anterior, middle, and posterior segments, inserting into the coronoid process and anterior aspect of the mandibular ramus.
- Medial pterygoid muscle, with superficial and deep heads, participates in jaw movement and excursion.
- Lateral pterygoid muscle helps in jaw protrusion and lateral movement.
Other Muscles Related to TMJ Function
- Contraction of the anterior belly of diagastric muscle results in mandible depression.
- Mylohyoid and geniohyoid muscles contribute to mandibular depression.
- Buccinator assists in cheek positioning during chewing.
Vascular Supply of Masticatory System
- The external carotid artery bifurcates into superficial temporal and internal maxillary arteries at the level of the condyle.
- These arteries supply the masticatory muscles and the TMJ.
Nerve Supply of Masticatory System
- The mandibular division of the trigeminal nerve provides motor innervation to mastication muscles.
- The auriculotemporal nerve innervates the TMJ.
- Deep temporal and masseteric nerves supply the anterior part of the joint.
Anatomy of Clinical Interest
- Jaw jerk reflex is a monosynaptic reflex of jaw closing muscles.
- Jaw opening reflex inhibits jaw closing muscles.
- Rest position / centric relation is the maxillomandibular relationship where each condyle articulates with the thinnest portion of the disc against the posterior slope of the articular eminence.
- The mandibular range of motion includes rotation and translation of the condyle and varies in individuals.
- Articular covering is thickest at areas with greatest functional load.
Disc Displacement
- Injury to the inferior lamina of posterior attachment is considered a cause of disc displacement.
- The angle of mandibular fossa might contribute to intra-articular disorders and chronic subluxation or dislocation of the condyle.
- Disc adhesions in the fossa could cause acute closed lock syndrome.
Clinical Tests for TMJ Assessment
- Muscle palpation
- Jaw jerk reflex
- Electromyography (EMG) activity
- Identifying the silent period
Joint Noises and Nerve Entrapment
- TMJ clicking might be due to condylar hypermobility, lateral pole enlargement, intra-articular bodies, and dysfunctional movement patterns.
- Nerve entrapment can occur.
Ear Symptoms Associated with TMDs
- Possible symptoms include earache, tinnitus, and fullness, or feeling of stiffness.
Etiology, Epidemiology, Classification of TMJ Disorders
-
Etiology includes premature occlusal contacts, masticatory muscle hyperactivity (bruxism and parafunction), psychological distress, trauma, and rheumatic disorders.
-
Prevalence of TMJ disorders is higher in women between the ages of 20 and 40 years.
-
Classification is based on the taxonomy of joint disorders, disc disorders, masticatory muscle disorders, and associated structures.
Diagnostic Imaging
- Plain film radiography
- Plain film tomography
- Arthrography
- CT scan
- MRI
- Single photon emission CT
- Radioisotope scanning
Diagnostic Local Anesthetic Nerve Blocks
- Injections in the TMJ, masticatory muscles, or trigger areas.
Prediction of TMD Chronicity
- Pain that extends beyond a certain period.
- Pain persisting beyond usual healing time.
- Pain not responding to usual treatment.
General Principles of Treating TMDs
- Patient categorisation (remission, recurring, persistent symptoms).
- Implement surgical intervention.
- Use relaxation and cognitive behavioral therapy (CBT).
- Consulting a specialist when necessary.
Specific Disorders and their Management
- Myalgia and Myofascial Pain - Education, self-management, physiotherapy (active/passive modalities).
- Instructions to patients for self-care.
- Intra oral appliances (splints, orthotics).
- Pharmacotherapy (NSAIDs, muscle relaxants).
- Behavioral therapy (relaxation techniques, biofeedback, hypnosis).
- Trigger point therapy, injections of local anesthetic.
- Restorative dental procedures.
Intra Oral Appliances
- Splints, orthotics, night guards, bite guards.
Articular Disc Disorders
- Abnormal relationships between the disc, condyle, and articular eminence.
- Common disc displacement is anterior and medial.
- Classified based on signs, symptoms, (e.g., ADD with/without reduction, intermittent locking) and diagnostic imaging.
Types of Disc Displacement
- Anterior disc displacement with reduction
- Anterior disc displacement without reduction
- Posterior disc displacement
Temporomandibular Joint Arthritis
- Degenerative joint diseases involve cartilage and subchondral bone, with secondary synovial membrane inflammation.
- Risk factors include gender, diet, genetics, and psychological stress.
- Presentation can include joint space narrowing, irregular joint space, flattening of articular surfaces, osteophyte formation, and anterior condylar lipping.
Other Types of TMJ Disorders
- Rheumatoid arthritis (primarily affecting periarticular tissue then bone, bilateral involvement, morning stiffness)
- Synovial chondromatosis (rare, cartilage nodules, progressive swelling)
- Septic arthritis (infection)
- Developmental disturbances (hyperplasia, hypoplasia, agenesis)
- Fractures (trauma)
- Dislocation
- Ankylosis (fusion) (bone fusion)
Sleep Bruxism
- Oral appliance therapy,
- Selective serotonin uptake inhibitors,
- Botulinum toxin
Oral Dyskinesia and Dystonia
- Abnormal, involuntary movements of tongue, lips, and jaw.
- Often related to poor fitting dentures associated with lack of replacement of teeth (important to manage).
- Emphasize management, including Botulinum toxin and neurosurgery.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.