Podcast
Questions and Answers
During the second stage of labor, what contraction pattern would be considered typical?
During the second stage of labor, what contraction pattern would be considered typical?
- Frequency of 10-15 minutes, duration of 20-30 seconds.
- Frequency of 5-7 minutes, duration of 30-40 seconds.
- Frequency of 1-2 minutes, duration of 50-90 seconds. (correct)
- Frequency of 3-5 minutes, duration of 40-60 seconds.
What biological response is most indicative of the second stage of labor?
What biological response is most indicative of the second stage of labor?
- Reduced urge to push.
- Increased desire to ambulate.
- Decreased intra-abdominal pressure.
- Perineal burning and stretching. (correct)
A multiparous woman is in the second stage of labor. How long is this stage expected to last typically?
A multiparous woman is in the second stage of labor. How long is this stage expected to last typically?
- 4 to 6 hours
- 2 to 4 hours
- Less than 1 hour (correct)
- 1 to 2 hours
During the third stage of labor, which observation suggests placental separation?
During the third stage of labor, which observation suggests placental separation?
Which of the following interventions is most appropriate during the second stage of labor?
Which of the following interventions is most appropriate during the second stage of labor?
A woman in labor is experiencing contractions every 4 minutes, lasting 35 seconds each, and reports increasing bloody show. Her cervix is 6 cm dilated. Which stage of labor is she most likely in?
A woman in labor is experiencing contractions every 4 minutes, lasting 35 seconds each, and reports increasing bloody show. Her cervix is 6 cm dilated. Which stage of labor is she most likely in?
During which phase of the first stage of labor is a woman most likely to exhibit behaviors such as panic, irritability, and a feeling of loss of control?
During which phase of the first stage of labor is a woman most likely to exhibit behaviors such as panic, irritability, and a feeling of loss of control?
Which of the following scenarios necessitates an emergent Cesarean section?
Which of the following scenarios necessitates an emergent Cesarean section?
A postpartum patient who underwent a C-section is being discharged. Which instruction regarding lifting is MOST appropriate?
A postpartum patient who underwent a C-section is being discharged. Which instruction regarding lifting is MOST appropriate?
A nulliparous woman arrives at the labor and delivery unit stating that she thinks she is in labor. Which finding would help the nurse determine that the woman is in the latent phase of labor?
A nulliparous woman arrives at the labor and delivery unit stating that she thinks she is in labor. Which finding would help the nurse determine that the woman is in the latent phase of labor?
A patient who had a C-section is experiencing significant gas pain. Besides medication, which of the following non-pharmacological interventions is MOST appropriate?
A patient who had a C-section is experiencing significant gas pain. Besides medication, which of the following non-pharmacological interventions is MOST appropriate?
A laboring woman reports feeling nauseous and experiencing leg cramps. Assessment reveals she is 9 cm dilated. What stage of labor is she in?
A laboring woman reports feeling nauseous and experiencing leg cramps. Assessment reveals she is 9 cm dilated. What stage of labor is she in?
A patient in labor is experiencing strong contractions lasting 50 seconds each, occurring every 2 minutes. She is increasingly irritable and feels a stretching sensation deep in her pelvis. These signs indicate which stage?
A patient in labor is experiencing strong contractions lasting 50 seconds each, occurring every 2 minutes. She is increasingly irritable and feels a stretching sensation deep in her pelvis. These signs indicate which stage?
Prior to administering an epidural, what is the priority nursing intervention?
Prior to administering an epidural, what is the priority nursing intervention?
A woman in labor is breathing rapidly and states that she feels like she is losing control. Upon assessment, her cervix is found to be 7 cm dilated. Which of the following nursing interventions is most appropriate?
A woman in labor is breathing rapidly and states that she feels like she is losing control. Upon assessment, her cervix is found to be 7 cm dilated. Which of the following nursing interventions is most appropriate?
During epidural administration, how should the patient be positioned?
During epidural administration, how should the patient be positioned?
Which of the following is a characteristic of the latent phase of the first stage of labor?
Which of the following is a characteristic of the latent phase of the first stage of labor?
A fetal heart rate monitor indicates variable decelerations during labor. According to the mnemonic VC-EH-AO-LP, what does this signify, and what is an appropriate initial intervention?
A fetal heart rate monitor indicates variable decelerations during labor. According to the mnemonic VC-EH-AO-LP, what does this signify, and what is an appropriate initial intervention?
A client in the immediate postpartum period reports feeling intense chills. Which of the following is the most appropriate nursing intervention?
A client in the immediate postpartum period reports feeling intense chills. Which of the following is the most appropriate nursing intervention?
A woman experiencing back labor reports intense pain. Her contractions are regular, occurring every 3 minutes and lasting 40 seconds. The monitor shows a cervical dilation of 5 cm. What stage of labor would the nurse document?
A woman experiencing back labor reports intense pain. Her contractions are regular, occurring every 3 minutes and lasting 40 seconds. The monitor shows a cervical dilation of 5 cm. What stage of labor would the nurse document?
Late decelerations are observed on the fetal heart rate monitor. Based on the mnemonic VC-EH-AO-LP, what does LP indicate, and what is the MOST appropriate intervention?
Late decelerations are observed on the fetal heart rate monitor. Based on the mnemonic VC-EH-AO-LP, what does LP indicate, and what is the MOST appropriate intervention?
Which medication is typically administered prior to a C-section to neutralize stomach acid?
Which medication is typically administered prior to a C-section to neutralize stomach acid?
During the fourth stage of labor, a nurse assesses a client and notes excessive bleeding. Which intervention should the nurse implement first?
During the fourth stage of labor, a nurse assesses a client and notes excessive bleeding. Which intervention should the nurse implement first?
A laboring client's contractions are irregular and subside with ambulation. The nurse recognizes these as signs of:
A laboring client's contractions are irregular and subside with ambulation. The nurse recognizes these as signs of:
A nurse is teaching a childbirth education class about non-pharmacological methods to induce labor. Which of the following should be included?
A nurse is teaching a childbirth education class about non-pharmacological methods to induce labor. Which of the following should be included?
A laboring client is using the open glottis pushing technique. Which statement reflects the correct application of this method?
A laboring client is using the open glottis pushing technique. Which statement reflects the correct application of this method?
After spontaneous rupture of membranes, a nurse notes a strong odor to the amniotic fluid using the COAT assessment. This finding should prompt the nurse to prioritize:
After spontaneous rupture of membranes, a nurse notes a strong odor to the amniotic fluid using the COAT assessment. This finding should prompt the nurse to prioritize:
Following an amniotomy, a nurse assesses the amniotic fluid using nitrazine paper. A blue result indicates:
Following an amniotomy, a nurse assesses the amniotic fluid using nitrazine paper. A blue result indicates:
A client's membranes have ruptured, and the nurse encourages ambulation. What is the rationale for this nursing intervention?
A client's membranes have ruptured, and the nurse encourages ambulation. What is the rationale for this nursing intervention?
A patient's amniotic fluid is noted to contain meconium after artificial rupture of membranes (AROM). What is the MOST important initial nursing action?
A patient's amniotic fluid is noted to contain meconium after artificial rupture of membranes (AROM). What is the MOST important initial nursing action?
During active labor, a patient reports intense pain and exhibits signs of being inwardly focused, with contractions occurring every 4 minutes. Which of the following pain scores and coping mechanisms BEST aligns with these observations?
During active labor, a patient reports intense pain and exhibits signs of being inwardly focused, with contractions occurring every 4 minutes. Which of the following pain scores and coping mechanisms BEST aligns with these observations?
A postpartum patient is experiencing continued uterine contractions after delivery. What physiological process explains this phenomenon?
A postpartum patient is experiencing continued uterine contractions after delivery. What physiological process explains this phenomenon?
Which maternal position is MOST conducive to fetal descent and effective pushing during the second stage of labor?
Which maternal position is MOST conducive to fetal descent and effective pushing during the second stage of labor?
A patient in labor presents with a maternal fever, foul-smelling amniotic fluid, and fetal tachycardia. Which of the following interventions is LEAST appropriate?
A patient in labor presents with a maternal fever, foul-smelling amniotic fluid, and fetal tachycardia. Which of the following interventions is LEAST appropriate?
During a prenatal visit, a patient at 30 weeks gestation is found to have painless, bright red vaginal bleeding. What condition is MOST likely indicated by these signs and symptoms?
During a prenatal visit, a patient at 30 weeks gestation is found to have painless, bright red vaginal bleeding. What condition is MOST likely indicated by these signs and symptoms?
Which of the following patients is at the HIGHEST risk for uterine rupture during labor?
Which of the following patients is at the HIGHEST risk for uterine rupture during labor?
During Leopold's maneuvers, the nurse palpates a soft, irregular mass in the fundus of the uterus. Which fetal part is MOST likely occupying this location?
During Leopold's maneuvers, the nurse palpates a soft, irregular mass in the fundus of the uterus. Which fetal part is MOST likely occupying this location?
What is the primary purpose of an external cephalic version (ECV)?
What is the primary purpose of an external cephalic version (ECV)?
Which of the following is a contraindication for a trial of labor after cesarean (TOLAC)?
Which of the following is a contraindication for a trial of labor after cesarean (TOLAC)?
A patient's Bishop score is assessed to be 9. Based on this finding, what is the most appropriate intervention?
A patient's Bishop score is assessed to be 9. Based on this finding, what is the most appropriate intervention?
During vacuum-assisted delivery, what complication is the '3 pull rule' designed to minimize?
During vacuum-assisted delivery, what complication is the '3 pull rule' designed to minimize?
A laboring patient with ruptured membranes (ROM) is in the latent phase of labor with a category 1 fetal heart rate (FHR) tracing. What is the most appropriate nursing action?
A laboring patient with ruptured membranes (ROM) is in the latent phase of labor with a category 1 fetal heart rate (FHR) tracing. What is the most appropriate nursing action?
What is the primary nursing intervention when a prolapsed umbilical cord is discovered?
What is the primary nursing intervention when a prolapsed umbilical cord is discovered?
Which of the following correctly sequences the first four cardinal movements of labor?
Which of the following correctly sequences the first four cardinal movements of labor?
During vacuum extraction, what action should the nurse expect the patient to perform in conjunction with the application of traction?
During vacuum extraction, what action should the nurse expect the patient to perform in conjunction with the application of traction?
Flashcards
Stage 1 of Labor
Stage 1 of Labor
Latent, Active, and Transitional phases.
Latent Phase
Latent Phase
Longest phase; cervix effaces, dilates to 4 cm; mild contractions every 5-15 min lasting 10-30 sec.
Active Phase
Active Phase
Cervix dilates from 6-7 cm; contractions every 3-5 min lasting 30-45 sec (mod/strong).
Transitional Phase
Transitional Phase
Signup and view all the flashcards
Length of Latent Phase
Length of Latent Phase
Signup and view all the flashcards
Length of Active Phase
Length of Active Phase
Signup and view all the flashcards
Length of Transitional Phase
Length of Transitional Phase
Signup and view all the flashcards
Personal Response during Latent Phase
Personal Response during Latent Phase
Signup and view all the flashcards
Interventions during labor
Interventions during labor
Signup and view all the flashcards
2nd stage of labor
2nd stage of labor
Signup and view all the flashcards
Contractions in 2nd stage
Contractions in 2nd stage
Signup and view all the flashcards
2nd stage Interventions
2nd stage Interventions
Signup and view all the flashcards
Signs of placental separation
Signs of placental separation
Signup and view all the flashcards
Why administer Oxytocin postpartum?
Why administer Oxytocin postpartum?
Signup and view all the flashcards
Length & main risk of the 4th stage of labor
Length & main risk of the 4th stage of labor
Signup and view all the flashcards
Intervention during the 4th stage of labor
Intervention during the 4th stage of labor
Signup and view all the flashcards
Non-pharmacological ways to induce labor
Non-pharmacological ways to induce labor
Signup and view all the flashcards
Open Glottis Pushing
Open Glottis Pushing
Signup and view all the flashcards
True signs of labor
True signs of labor
Signup and view all the flashcards
COAT Acronym
COAT Acronym
Signup and view all the flashcards
Tests to confirm amniotic fluid
Tests to confirm amniotic fluid
Signup and view all the flashcards
Emergent Delivery
Emergent Delivery
Signup and view all the flashcards
Post C-Section Care
Post C-Section Care
Signup and view all the flashcards
Activity Restrictions Post C-Section
Activity Restrictions Post C-Section
Signup and view all the flashcards
Pre-C-Section Medication
Pre-C-Section Medication
Signup and view all the flashcards
Priority Before Epidural
Priority Before Epidural
Signup and view all the flashcards
Nursing Actions After Epidural
Nursing Actions After Epidural
Signup and view all the flashcards
VEAL CHOP
VEAL CHOP
Signup and view all the flashcards
Interventions for Late Decelerations
Interventions for Late Decelerations
Signup and view all the flashcards
External Cephalic Version (ECV)
External Cephalic Version (ECV)
Signup and view all the flashcards
TOLAC
TOLAC
Signup and view all the flashcards
VBAC
VBAC
Signup and view all the flashcards
Bishop Score
Bishop Score
Signup and view all the flashcards
Operative Vaginal Delivery
Operative Vaginal Delivery
Signup and view all the flashcards
Ferguson Reflex
Ferguson Reflex
Signup and view all the flashcards
7 Cardinal Movements of Labor
7 Cardinal Movements of Labor
Signup and view all the flashcards
Priority action after Rupture of Membranes
Priority action after Rupture of Membranes
Signup and view all the flashcards
AROM: Nursing priority?
AROM: Nursing priority?
Signup and view all the flashcards
Active Labor Characteristics
Active Labor Characteristics
Signup and view all the flashcards
Chorioamnionitis Signs
Chorioamnionitis Signs
Signup and view all the flashcards
Chorioamnionitis Interventions
Chorioamnionitis Interventions
Signup and view all the flashcards
Fetal Tachycardia
Fetal Tachycardia
Signup and view all the flashcards
Placenta Previa S/S
Placenta Previa S/S
Signup and view all the flashcards
Placenta Abruption S/S
Placenta Abruption S/S
Signup and view all the flashcards
Signs of Impending Labor
Signs of Impending Labor
Signup and view all the flashcards
Study Notes
- Study notes for the Nur 335 exam 2 on Maternal Health Theory & Application
Stage 1 of Labor
- Consists of latent, active, and transitional phases; a mnemonic to remember labor actively transitioning exists
Stages of Labor
Latent Phase
- The longest stage
- Lasts 6-12 hours
- Causes cervical effacement and dilation to 4 cm
- Contractions occur every 5-15 minutes, lasting 10-30 seconds at a mild intensity
- May or may not have show/membrane/station intact, usually at -2-0
- Biological response includes cramps, backache, excitement, anxiety, happiness, relief, curiosity, quietness, or talkativeness, and the need for information and reassurance
- Personal response includes thoughts centered on self, labor, and baby
Active phase
- Lasts 1-6 hours
- Causes cervical effacement and dilation to 6-7 cm
- Contractions occur every 3-5 minutes, lasting 30-45 seconds at a moderate/strong intensity
- Show/membrane/station increases, intact or ruptured at 0 - +2
- Biological response includes restlessness, labored respiration, hyperventilation, increasing fears and anxieties, and feeling threatened and inwardly focused
- Requires human presence
Transitional phase
- Lasts 1-2 hours, or 4 hours can be normal
- Causes cervical effacement to 10 cm
- Contractions occur every 1-2 minutes, lasting 40-60 seconds with strong intensity
- Show/membrane/station is heavy, usually ruptured at 0 - +2
- Causes leg cramps, nausea, vomiting, hiccups, belches, perspiration, and a pulling or stretching sensation deep in the pelvis, as well as panic, emotional, and irritable responses to external environment stimuli
- Personal response becomes limited, losing control; thoughts are on self, uncooperative, amnesic between contractions, and dependent
Interventions
- Involves lab tests, IV, fetal monitoring, assessing VS, GBS status, SVE, support, and comfort measures
Second Stage of Labor: Expulsive Phase
- Length for primiparas is 2-4 hours; for multiparas, less than 1 hour
- Cervix is fully dilated to 10 cm
- Contractions occur every 1-2 minutes, lasting 50-90 seconds, and are less painful and expulsive
- Show/membranes/station is heavy, ruptured at +4
- Intra-abdominal pressure is exerted (bearing down), urge to push, perineum bulges and flattens, perineal burning and stretching.
- Desires to sleep between contractions, amnesic between contractions
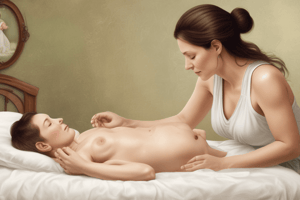
Interventions
- Instruct the woman to bear down with the urge to push, check Fetal Heart Rate (FHR), and provide comfort measures
Third Stage of Labor: Placenta
- Length is 1-20 minutes, with cervix closing
- Contractions are less painful
- Uterus rises and becomes globular shape, gush or flood as placenta separates, umbilical cord lengthens, cramping.
- May want to sleep, proud, happy, relief, may or may not display emotions
- Personal system is relieved
Interventions
- Oxytocin administration prevents hemorrhage
Fourth Stage of Labor: Immediate Postpartum
- Highest risk for hemorrhage
- Length is 2-4 hours, with the cervix closing
- Contractions cause cramping
- Biological response includes post-partum chills, hunger, thirst, drowsiness, moderate to heavy lochia, and usually painless uterine contractions
Interventions
- Fundal massage
Non-Pharmacological Ways to Induce Labor
- Ambulation and position changes
Two Different Pushing Techniques
Open Glottis
- Mom pushes only when she has the urge by continuing to breathe, which keeps the glottis open
- 3-4 times per contraction for 6-8 seconds
Closed Glottis
- Mom takes a deep breath and pushes for 10 seconds
- 2-3 times per contraction
Signs of Labor
- True labor presents with cervical changes (effacement, dilation, station), patterned contractions, and contractions while laying down
- False labor presents with irregular contractions, and contractions go away with ambulation, position changes, and laying down
COAT Acronym
- Describes and assesses amniotic fluid (Color, Odor, Amount, Time)
Tests to Confirm Amniotic Fluid
- Fern test (looking for ferns under a microscope)
- Amnisure (non-invasive test looking for amniotic protein)
- Nitrazine paper (will turn blue if amniotic fluid is present)
Management After Water Breaks
- No ambulation to progress labor
Reasons to Monitor Rupture Time
- Risk of infection and a small window of time for the baby to remain in the mom after rupture exists
Reasons to do Amnioinfusion
- Thick meconium
- Low amniotic fluid
- Variables and cord compression
Fetal Heart Rate Monitoring (FHR 1)
- Desirable findings include a baseline of 110-160, moderate variability, absent late or variable decelerations, absent or present early decelerations, and absent or present accelerations
FHR 2
-
Undesirable findings include a baseline rate of Bradycardia not accompanied by absent baseline variability, or a baseline rate of Tachycardia
-
Minimal variability
-
Absent variability without recurrent decelerations
-
Marked variability
-
Absence of induced accelerations after fetal stimulation
-
Recurrent variable decelerations with minimal or moderate variability
-
Prolonged deceleration
-
Recurrent late decelerations with moderate variability
-
Variable decelerations with “slow return to baseline," “overshoots," or "shoulders"
Intervention
- Reposition the mom
FHR 3
- Contains absent variability with, recurrent late decelerations, recurrent variable decelerations, bradycardia, and sinusoidal pattern
Clinical Situations and Interventions
-
Minimal or absent variability/Recurrent late decelerations: Promote fetal oxygenation by lateral positioning, IV fluid bolus of lactated Ringer's solution, and oxygen administration at 10 L/min via nonrebreather face mask.
-
Recurrent variable decelerations: Modification of pushing efforts; pushing with every other or every third contraction or discontinuation of pushing temporarily (during second stage labor)
-
Tachycardia Bradycardia: Decrease in oxytocin rate
-
Variable, late or prolonged decelerations occurring with maternal pushing efforts: Discontinuation of oxytocin / removal of Cervidil insert/withholding next dose of misoprostol
-
Tachysystole: Reduce uterine activity with IV fluid bolus of lactated Ringer's solution, lateral positioning, decrease/discontinuation of oxytocin
-
Recurrent variable decelerations: Alleviate umbilical cord compression with Amnioinfusion
-
Maternal hypotension: Correct maternal hypotension with lateral positioning and IV fluid bolus of lactated Ringer's solution
Prioritization
- A mom having a category 3 VS is more urgent and would go to surgery first, compared to a mom having labor dystocia and not progressing
Fetal Tachycardia Causes
- Fever and infection
Tachysystole interventions
- Cool mom down with towels and ice
Tachysystole Contractions
- 5 contractions in 10 minutes
- Lasting longer than 120 seconds
- Resting tone is increased
- Less than one minute apart
Fetal Bradycardia Causes
- Perfusion issues; uterine detachment and cord compression
Pressure After SROM and AROM Causes
- Placenta abruptio (detachment) or cord prolapse
Management of a Prolapsed Cord
- Push the head back with fingers to relieve pressure off the cord
Labor Dystocia
- Dilation of more than or equal to 6 cm dilation with membrane rupture and 6 hours or more of inadequate contractions and no cervical change
- New moms and uterine abnormalities are at most risk
Intervention
- Suprapubic pressure (use stool for higher ground) and McRoberts maneuver (mom's thighs towards abdomen)
Actions for Labor Dystocia That Isn't Progressing
- C-section
Turtle Sign
- Indicates shoulder dystocia, where the baby's head starts coming out and then goes back in because the anterior shoulder is stuck on the mom's bone
Warning
- Never do a fundal pressure
Precipitous Delivery
- Fast delivery within 3 hours of the onset of labor
Risk Factors
- Tearing and cervical lacerations
Baby Risks
- A bruised face and broken vessels in the eyes
Action for History of Precipitous Deliveries
- Yes, because deliveries can become quicker each time and nurses need to prepare and know if mom is feeling any sensation of pressure
Thick Meconium Noted When BOW is Ruptured
- Amnioinfusion in labor and bulb syringe suctioning (mouth first and then nose)
Meconium Aspiration Syndrome (MAS)
- Abnormal inhalation of meconium (first stool) produced by a fetus or newborn
Anaphylactic Syndrome
- Emergent and has a high mortality rate
- Amniotic fluid gets into mom's system and causes an embolism
Triage Interventions
- Fetal heart rate monitoring
- Vitals
- Time of
Types of C-Section
Scheduled
- Occurs before the onset of birth due to a previous c-section or conditions that can put the mom/baby at risk during birth (malpresentation)
Non-Urgent
- Relates to complications such as failure to progress and failure to descend with category 1 FHR
Urgent
- Indicates a need for rapid delivery
- Malpresentation diagnosed after onset of labor or placenta previa with mild bleeding diagnosed after labor. and fetal heart rate with Category 1 FHR
Emergent
- Indicates an immediate need to deliver the fetus b/c of prolapse of umbilical cord or rupture of uterus
Care Instructions After C-Section
- Splinting with pillow
- No baths or swimming, only showers
- Watch the incision
- Report signs of infection
- Removed staples
- Lift nothing heavier than the baby
- No driving
- Ambulation
- For gas pain, ambulation, medications, use heating pad and carbonated drink
Medication Before C-Section
- Sodium citrate to neutralize stomach acid
Epidural
- 1st priority: assess BP and give a liter bolus of fluids
Interventions
- Keep the bladder empty with a straight cath
- Position changes every hour (turning side to side)
- Place mom in C shape position when giving epidural
V-C
- Variable decels and cord compression
- Interventions: This is not okay? Position changes and move on
E-H
- Early decels and Head compression
- Interventions: Okay sign and identify the process of labor
A-O
- Accelerations and oxygen okay
- Interventions: Okay sign and No intervention needed
L-P
- Late decels and perfusion
- Interventions: Not good expedite delivery, intrauterine resuscitation and evaluate why
External Cephalic Version (ECV)
- An attempt to manipulate and turn the fetus externally from a breech presentation to vertex presentation to allow for vaginal birth
Risks of ECV
- The procedure is done at the hospital because is risk for ROM, dangerous, painful
TOLAC & VBAC
- Trial of labor after cesarean & Vaginal birth after cesarean
Contraindications for TOLAC/VBAC
- Pelvic abnormalities that are not conducive for a vaginal birth
- Fetus lies transverse In mom's stomach
- History of 2 previous c/s
- vertical c-section incision
Bishop Score Assessment
- Assesses cervical readiness
High Bishop Score
- 8 or higher
- Favorable for induction! give Pitocin
Low Bishop Score
- Less than 6
- Give cervical ripening medication (cervidil, cytotec) to soften cervix
Operative Vaginal Delivery
- Vacuum assist or use of forceps to help deliver baby faster
Vacuum Assist Rule
- More than 3 or more attempts in 15 minutes can put baby at risk for increased brain bleeds, jaundice and puts mom at risk for lacerations and hemorrhage
Management of Category 1 FHR in Latent Labor w/ ROM
- Ambulation and position changes
Nursing Role During Stage 2 of Labor
- Encourage the patient to push 3-4 times with 6-8 seconds between urges
Ferguson Reflex
- Maternal urge to push
Sign of Labor Progression
- From stage 1 to 2
- The urge to push
Prolapsed Cord Priority Action
- Relieve pressure on cord by elevating presenting part
Seven Cardinal Movements of Labor
- Engagement
- Descent
- Flexion
- Internal Rotation
- Extension
- External Rotation
- Expulsion
Vacuum Extraction Assistance
- Patient will push with vacuum traction
Priority Action After ROM
- Assess the fetal heart rate to rule out cord prolapse
Characteristics of Active Labor
- Include internal focus and breathing, contractions every 3-5 minutes, pain 5-8, and using breathing techniques
Nursing Priority With AROM and Meconium Noted
- Notify NICU
Postpartum Contractions
- Contractions will be felt after the baby is born
Best Position in Stage 2 of Labor
- Elevate HOB and use of the squatting bar
Signs of Chorioamnionitis
- Maternal fever, foul-smelling amniotic fluid, fetal tachycardia
Interventions
- Cool the mom off, start antibiotics for mom and baby, do CBC and blood culture. - Tylenol to get fever down
Fetal Tachycardia Baseline
- A fetus with a baseline of 190 has tachycardia
Action for Controlling Pain
- Use local anesthesia to helps controlling pain with stitches
When To Give Nitrate Oxide
- Give 30 seconds before a contraction
Placenta Previa Signs and Symptoms
- Bright red bleeding that is painless
- Drop in BP
- Baby has late decelerations
Placenta Abruption Signs and Symptoms
- Painful, dark red bleeding, late deceleration
Risk for Uterine Rupture
- Previous c-section due to uterus scarring,
Rupturing Bag of Water
- Rupture the bag of water when the baby's head is engaged
Signs Mom Is Going Into Labor
- Nesting, lightening, loss of mucus plug, weight loss, persistent backache, increased Braxton hicks
Leopold’s Maneuvers: Determining Fetal Position
- 1st maneuver: determine what part of the fetus is located in the fundus of the uterus
- 2nd maneuver: determine location of the fetal back
- 3rd maneuver: determine the presenting part
- 4th maneuver: determine the location of the cephalic prominence.
The 5 P’s of Labor: Factors Affecting Labor Progress
- Passenger (fetus and placenta), passage (birth canal), powers (contractions), position (of the mother), and psychology
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.