Podcast
Questions and Answers
Which stage of labor begins with the onset of regular contractions and ends with full cervical dilation?
Which stage of labor begins with the onset of regular contractions and ends with full cervical dilation?
- First stage (correct)
- Second stage
- Fourth stage
- Third stage
The latent phase of the first stage of labor is characterized by strong, regular contractions and rapid cervical dilation.
The latent phase of the first stage of labor is characterized by strong, regular contractions and rapid cervical dilation.
False (B)
What marks the beginning and end of the third stage of labor?
What marks the beginning and end of the third stage of labor?
Begins after the birth of the baby and ends with the delivery of the placenta and membranes.
The hour immediately following delivery is known as the ______ stage of labor.
The hour immediately following delivery is known as the ______ stage of labor.
Match the phases of the first stage of labor with their descriptions:
Match the phases of the first stage of labor with their descriptions:
What is the normal range for baseline fetal heart rate (FHR)?
What is the normal range for baseline fetal heart rate (FHR)?
Absent FHR variability indicates a healthy interplay between the fetal sympathetic and parasympathetic nervous systems.
Absent FHR variability indicates a healthy interplay between the fetal sympathetic and parasympathetic nervous systems.
What does FHR variability reflect?
What does FHR variability reflect?
An amplitude range of 6-25 bpm in FHR variability is classified as ______ variability.
An amplitude range of 6-25 bpm in FHR variability is classified as ______ variability.
Match the FHR variability ranges with their classifications:
Match the FHR variability ranges with their classifications:
During which phase of the second stage of labor does the woman experience an urge to push as the fetus descends further into the pelvis?
During which phase of the second stage of labor does the woman experience an urge to push as the fetus descends further into the pelvis?
External fetal monitoring involves placing an electrode on the fetal scalp to directly measure FHR.
External fetal monitoring involves placing an electrode on the fetal scalp to directly measure FHR.
What is the purpose of an intrauterine pressure catheter (IUPC)?
What is the purpose of an intrauterine pressure catheter (IUPC)?
The active phase of the second stage of labor involves maternal expulsive efforts combined with ______ to deliver the baby.
The active phase of the second stage of labor involves maternal expulsive efforts combined with ______ to deliver the baby.
Match the type of fetal monitoring with its method:
Match the type of fetal monitoring with its method:
What is the primary focus of obstetrics?
What is the primary focus of obstetrics?
Gynaecology exclusively deals with pregnancy and childbirth.
Gynaecology exclusively deals with pregnancy and childbirth.
Define labour and delivery in a single sentence.
Define labour and delivery in a single sentence.
Full cervical dilation is defined as ______ cm.
Full cervical dilation is defined as ______ cm.
Match the medical field with its primary focus:
Match the medical field with its primary focus:
Flashcards
Obstetrics
Obstetrics
Focuses on pregnancy, childbirth, and the postpartum period.
Gynaecology
Gynaecology
Deals with the health of the female reproductive system.
Labour and delivery
Labour and delivery
Physiological process of childbirth, encompassing all stages.
First stage of labour
First stage of labour
Signup and view all the flashcards
Latent phase
Latent phase
Signup and view all the flashcards
Active phase
Active phase
Signup and view all the flashcards
Transition phase
Transition phase
Signup and view all the flashcards
Second stage of labour
Second stage of labour
Signup and view all the flashcards
Passive phase
Passive phase
Signup and view all the flashcards
Active phase of second stage
Active phase of second stage
Signup and view all the flashcards
Third stage of labour
Third stage of labour
Signup and view all the flashcards
Fourth stage of labour
Fourth stage of labour
Signup and view all the flashcards
Electronic fetal monitoring (EFM)
Electronic fetal monitoring (EFM)
Signup and view all the flashcards
External monitoring
External monitoring
Signup and view all the flashcards
Internal monitoring
Internal monitoring
Signup and view all the flashcards
Baseline FHR
Baseline FHR
Signup and view all the flashcards
FHR variability
FHR variability
Signup and view all the flashcards
Absent variability
Absent variability
Signup and view all the flashcards
Minimal variability
Minimal variability
Signup and view all the flashcards
Moderate variability
Moderate variability
Signup and view all the flashcards
Study Notes
- Obstetrics focuses on pregnancy, childbirth, and the postpartum period.
- Gynaecology deals with the health of the female reproductive system.
- Labour and delivery encompass the physiological process of childbirth.
Stages of Labour
- First stage: begins with the onset of regular contractions and ends with full cervical dilation (10 cm).
- Latent phase: early part of the first stage, characterized by mild, irregular contractions and slow cervical dilation.
- Active phase: contractions become stronger, more frequent, and regular, leading to more rapid cervical dilation.
- Transition phase: the final part of the first stage, with intense contractions and increasing pressure in the rectum.
- Second stage: complete cervical dilation to the birth of the baby.
- Passive phase: foetus descends further into the pelvis, woman has an urge to push.
- Active phase: maternal expulsive efforts combined with uterine contractions to deliver the baby.
- Third stage: begins immediately after the birth of the baby and ends with the delivery of the placenta and membranes.
- Fourth stage: the hour immediately following delivery.
Fetal Monitoring
- Electronic fetal monitoring (EFM) is used to assess fetal well-being during labour.
- External monitoring: uses transducers placed on the mother's abdomen to detect fetal heart rate (FHR) and uterine contractions.
- Internal monitoring: involves placing an electrode on the fetal scalp to directly measure FHR and an intrauterine pressure catheter (IUPC) to measure contractions.
- Baseline FHR: the average FHR during a 10-minute segment, excluding accelerations, decelerations, and marked variability. Normal baseline FHR is 110-160 bpm.
- FHR variability: fluctuations in the baseline FHR, reflecting the interplay between the sympathetic and parasympathetic nervous systems; indicates fetal reserve.
- Absent variability: amplitude range undetectable.
- Minimal variability: amplitude range ≤ 5 bpm.
- Moderate variability: amplitude range 6-25 bpm.
- Marked variability: amplitude range > 25 bpm.
- Accelerations: abrupt increases in FHR above the baseline.
- Visually apparent abrupt increase (onset to peak <30 seconds).
- At ≥32 weeks of gestation, ≥15 bpm above the baseline and lasting ≥15 seconds but <2 minutes.
- Before 32 weeks of gestation, ≥10 bpm above the baseline and lasting ≥10 seconds but <2 minutes.
- Decelerations: decreases in FHR below the baseline.
- Early decelerations: gradual decrease (onset to nadir ≥30 seconds) in FHR with the onset and end coinciding with uterine contractions; caused by fetal head compression.
- Late decelerations: gradual decrease (onset to nadir ≥30 seconds) in FHR with the onset occurring after the start of a contraction and the nadir occurring after the peak of the contraction; usually caused by uteroplacental insufficiency.
- Variable decelerations: abrupt decrease (onset to nadir <30 seconds) in FHR, occurring at any time in relation to uterine contractions; usually caused by umbilical cord compression.
- Prolonged deceleration: FHR decreases ≥15 bpm below the baseline and lasting ≥2 minutes but <10 minutes.
Management of Labour
- Pain management:
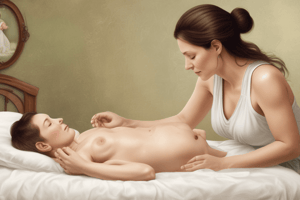
- Non-pharmacological methods: breathing techniques, massage, hydrotherapy.
- Pharmacological methods: epidural analgesia, systemic opioids.
- Augmentation of labour: stimulation of uterine contractions to accelerate labour.
- Amniotomy: artificial rupture of membranes (AROM).
- Oxytocin: synthetic hormone that stimulates uterine contractions.
- Management of the third stage of labour:
- Active management: administration of a uterotonic drug (e.g., oxytocin), umbilical cord clamping and cutting, and controlled cord traction.
- Physiological management: allowing the placenta to deliver spontaneously without intervention.
Delivery
- Vaginal delivery: the baby is born through the birth canal.
- Assisted vaginal delivery: use of instruments (e.g., forceps or vacuum extractor) to aid delivery.
- Cesarean delivery: the baby is delivered through an incision in the mother's abdomen and uterus.
- Indications: fetal distress, breech presentation, placental abnormalities, failure to progress in labour.
Postpartum Care
- Monitoring for postpartum hemorrhage: excessive bleeding after delivery; major cause of maternal mortality.
- Uterine atony: failure of the uterus to contract adequately after delivery.
- Assessment of perineal healing: the perineum is the area between the vagina and anus, which may be lacerated during delivery.
- Lactation support: assisting the mother with breastfeeding.
- Psychological support: addressing postpartum blues or depression.
Common Obstetric Complications
- Preterm labour: labour that begins before 37 weeks of gestation.
- Post-term pregnancy: pregnancy that lasts longer than 42 weeks of gestation.
- Preeclampsia: a pregnancy-specific condition characterized by high blood pressure and proteinuria.
- Gestational diabetes: diabetes that develops during pregnancy.
- Ectopic pregnancy: implantation of the fertilized ovum outside the uterus.
- Miscarriage: spontaneous loss of a pregnancy before 20 weeks of gestation.
- Stillbirth: the death of a fetus at or after 20 weeks of gestation.
Common Gynaecological Conditions
- Menstrual disorders:
- Amenorrhea: absence of menstruation.
- Dysmenorrhea: painful menstruation.
- Menorrhagia: heavy or prolonged menstrual bleeding.
- Pelvic inflammatory disease (PID): infection of the female reproductive organs.
- Endometriosis: the presence of endometrial tissue outside the uterus.
- Uterine fibroids: non-cancerous growths in the uterus.
- Ovarian cysts: fluid-filled sacs on the ovary.
- Polycystic ovary syndrome (PCOS): hormonal disorder causing enlarged ovaries with small cysts on the outer edges.
- Cervical dysplasia: abnormal changes in the cells of the cervix.
- Gynaecological cancers: cancers of the female reproductive organs (e.g., cervical, ovarian, uterine).
Gynaecological Procedures
- Pap smear: screening test for cervical cancer.
- Colposcopy: examination of the cervix using a magnifying instrument.
- Hysterectomy: surgical removal of the uterus.
- Oophorectomy: surgical removal of one or both ovaries.
- Salpingectomy: surgical removal of one or both fallopian tubes.
- Dilation and curettage (D&C): surgical procedure in which the cervix is dilated and the uterine lining is scraped.
- Laparoscopy: minimally invasive surgical procedure using a small incision and a camera to visualize the pelvic organs.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.