Podcast
Questions and Answers
What is the underlying pathophysiology of Equine Degenerative Myeloencephalopathy (EDM)?
What is the underlying pathophysiology of Equine Degenerative Myeloencephalopathy (EDM)?
- Oxidative damage to the CNS due to difficulty in assimilating vitamin E. (correct)
- Inflammation of the spinal cord caused by protozoal migration from peripheral tissues.
- Autoimmune destruction of myelin sheaths in the spinal cord.
- Direct viral invasion of the central nervous system by herpesviruses.
Which of the following is the MOST accurate description of the neuroanatomic localization typically associated with Equine Degenerative Myeloencephalopathy (EDM) on neurologic examination?
Which of the following is the MOST accurate description of the neuroanatomic localization typically associated with Equine Degenerative Myeloencephalopathy (EDM) on neurologic examination?
- Diffuse spinal cord involvement, often with decreased cutaneous trunci reflex. (correct)
- Cerebellar dysfunction leading to ataxia and dysmetria.
- Focal lesion in the brainstem causing cranial nerve deficits.
- Unilateral spinal cord lesion resulting in asymmetrical weakness.
What diagnostic approach is MOST crucial in confirming Equine Degenerative Myeloencephalopathy (EDM) in a horse?
What diagnostic approach is MOST crucial in confirming Equine Degenerative Myeloencephalopathy (EDM) in a horse?
- Performing a muscle biopsy to identify protozoal cysts.
- Using advanced imaging techniques like MRI to visualize spinal cord lesions.
- Ruling out other potential causes through a process of elimination. (correct)
- Analyzing CSF for elevated antibody titers against specific viral pathogens.
In managing Equine Degenerative Myeloencephalopathy (EDM), what is the primary goal of vitamin E supplementation?
In managing Equine Degenerative Myeloencephalopathy (EDM), what is the primary goal of vitamin E supplementation?
What role does the opossum play in the transmission cycle of Sarcocystis neurona, the causative agent of Equine Protozoal Myelitis (EPM)?
What role does the opossum play in the transmission cycle of Sarcocystis neurona, the causative agent of Equine Protozoal Myelitis (EPM)?
Which of the following clinical signs is LEAST likely to be associated with Equine Protozoal Myelitis (EPM)?
Which of the following clinical signs is LEAST likely to be associated with Equine Protozoal Myelitis (EPM)?
Why might a CSF analysis yield normal results in a horse with confirmed Equine Protozoal Myelitis (EPM)?
Why might a CSF analysis yield normal results in a horse with confirmed Equine Protozoal Myelitis (EPM)?
What is the significance of a seronegative result on a Western blot in the diagnosis of Equine Protozoal Myelitis (EPM), and how does it influence diagnostic decisions?
What is the significance of a seronegative result on a Western blot in the diagnosis of Equine Protozoal Myelitis (EPM), and how does it influence diagnostic decisions?
What is the primary mechanism of action of ponazuril (Marquis®) in treating Equine Protozoal Myelitis (EPM)?
What is the primary mechanism of action of ponazuril (Marquis®) in treating Equine Protozoal Myelitis (EPM)?
Why are corticosteroids generally contraindicated in horses with Equine Protozoal Myelitis (EPM)?
Why are corticosteroids generally contraindicated in horses with Equine Protozoal Myelitis (EPM)?
What is the MOST critical factor influencing the prognosis for horses diagnosed with Equine Protozoal Myelitis (EPM)?
What is the MOST critical factor influencing the prognosis for horses diagnosed with Equine Protozoal Myelitis (EPM)?
Which of the following biosecurity measures is MOST effective in preventing the spread of Equine Protozoal Myelitis (EPM) among horses in a stable?
Which of the following biosecurity measures is MOST effective in preventing the spread of Equine Protozoal Myelitis (EPM) among horses in a stable?
What is the significance of the AA substitution at position 752 in the viral DNA polymerase of the neuropathic strain of Equine Herpesvirus-1 (EHV-1)?
What is the significance of the AA substitution at position 752 in the viral DNA polymerase of the neuropathic strain of Equine Herpesvirus-1 (EHV-1)?
During an outbreak of neuropathic Equine Herpesvirus-1 (EHV-1), what clinical signs would be MOST indicative of neurologic involvement?
During an outbreak of neuropathic Equine Herpesvirus-1 (EHV-1), what clinical signs would be MOST indicative of neurologic involvement?
What would CSF analysis reveal in a horse affected by the neuropathic form of Equine Herpesvirus-1 (EHV-1)?
What would CSF analysis reveal in a horse affected by the neuropathic form of Equine Herpesvirus-1 (EHV-1)?
Why is prompt isolation of affected horses a CRITICAL step in managing an outbreak of neuropathic Equine Herpesvirus-1 (EHV-1)?
Why is prompt isolation of affected horses a CRITICAL step in managing an outbreak of neuropathic Equine Herpesvirus-1 (EHV-1)?
In cases of neuropathic Equine Herpesvirus-1 (EHV-1), what is the rationale behind using antiviral therapy, such as valacyclovir or IV acyclovir, despite the limitations of oral acyclovir?
In cases of neuropathic Equine Herpesvirus-1 (EHV-1), what is the rationale behind using antiviral therapy, such as valacyclovir or IV acyclovir, despite the limitations of oral acyclovir?
What is the MOST significant reason for a poor prognosis in horses affected by the neuropathic form of Equine Herpesvirus-1 (EHV-1)?
What is the MOST significant reason for a poor prognosis in horses affected by the neuropathic form of Equine Herpesvirus-1 (EHV-1)?
What role does vaccination play in reducing the impact of Equine Herpesvirus-1 (EHV-1) outbreaks, considering its limitations?
What role does vaccination play in reducing the impact of Equine Herpesvirus-1 (EHV-1) outbreaks, considering its limitations?
How does corticosteroid administration potentially affect horses with latent Equine Herpesvirus-1 (EHV-1) infection?
How does corticosteroid administration potentially affect horses with latent Equine Herpesvirus-1 (EHV-1) infection?
Flashcards
Equine Degenerative Myeloencephalopathy (EDM)
Equine Degenerative Myeloencephalopathy (EDM)
Oxidative damage to CNS due to difficulty assimilating vitamin E; causes spheroid formation in brainstem nuclei and neuraxonal dystrophy.
Neurologic signs of EDM
Neurologic signs of EDM
Symmetric gait deficits with prominent spasticity; forelimb deficits equal to or worse than hind limbs, diffuse spinal cord involvement, decreased cutaneous trunci reflex.
Equine Protozoal Myelitis (EPM)
Equine Protozoal Myelitis (EPM)
Protozoal infection by Sarcocystis neurona affecting the spinal cord and brainstem.
EPM Transmission
EPM Transmission
Signup and view all the flashcards
EPM Clinical Signs and Progression
EPM Clinical Signs and Progression
Signup and view all the flashcards
CSF Analysis in EPM
CSF Analysis in EPM
Signup and view all the flashcards
SAG-2, 4/3 ELISA for EPM
SAG-2, 4/3 ELISA for EPM
Signup and view all the flashcards
Ponazuril (Marquis®) for EPM
Ponazuril (Marquis®) for EPM
Signup and view all the flashcards
Diclazuril (Protazil®) for EPM
Diclazuril (Protazil®) for EPM
Signup and view all the flashcards
Neurologic examination findings for EHV-1
Neurologic examination findings for EHV-1
Signup and view all the flashcards
Treatment for EHV-1
Treatment for EHV-1
Signup and view all the flashcards
Equine Herpes Myeloencephalitis (EHV-1)
Equine Herpes Myeloencephalitis (EHV-1)
Signup and view all the flashcards
EHV-1 Pathophysiology
EHV-1 Pathophysiology
Signup and view all the flashcards
Study Notes
- Spinal Ataxia II encompasses:
- Equine Degenerative Myeloencephalopathy (EDM)
- Equine Protozoal Myelitis
- Equine Herpesvirus Myeloencephalopathy
Equine Degenerative Myelopathy
- Affected horses struggle to assimilate vitamin E, leading to oxidative damage in the CNS.
- This results in spheroid formation in brainstem nuclei, neuraxonal dystrophy in lumbosacral and cervical intermediate gray columns.
- It also causes neuronal degeneration in ventral and dorsal spinocerebellar tracts, and ventromedial funiculi.
- Signalment includes horses aged 6 months to 2 years, with no gender predilection.
- It's familial in Standardbreds, Morgans, Thoroughbreds, Quarterhorses, and Zebras.
- Neurologic examination reveals symmetric gait deficits (prominent spasticity), with forelimb deficits equal to or worse than hind limbs.
- Neuroanatomic localization is diffuse spinal cord, with decreased cutaneous trunci reflex.
- Diagnosed by exclusion, it involves unremarkable CSF analysis, cervical radiographs, and myelographic examination.
- Serum vitamin E concentrations may be low, and necropsy examination requires submitting the medulla, pons, and thoracic spinal cord.
- Treatment involves Vitamin E supplementation (10,000 IU PO SID x 6 months, natural).
- Supplementation may prevent disease progression but is unlikely to reverse clinical signs.
- Neurologic dysfunction does not progress to recumbency, and signs plateau at 2 to 3 years of age, remaining stable throughout life.
Equine Protozoal Myelitis (EPM)
- Caused by the protozoal organism Sarcocystis neurona within the spinal cord and cerebrum/brainstem.
- Horses become infected via ingestion of opossum feces.
- Horses are dead-end hosts, and only asexual forms of the organism are seen in horses; horse-to-horse transmission does not occur.
- Sarcocystis neurona has a two-host lifecycle, with cats, skunks, raccoons, and armadillos serving as secondary hosts.
- The organism encysts in the secondary host muscle, completing its lifecycle when an opossum eats it.
- Clinical disease is reported in all breeds and ages, peaking from 15 months to 5 years, and rare in ponies or horses younger than 1 year.
- Its geographic distribution corresponds to opossum populations.
- Neurologic exams show the neuroanatomic localization depends on the organism's location in the central nervous system.
- Multifocal disease, asymmetric signs, and/or focal muscle mass loss should raise suspicion for EPM.
- Clinical signs may be insidious or acute, with progression being rapid, slow, or static.
- Cytologic evaluation during CSF analysis shows mild protein and total cell count elevation (mononuclear pleocytosis).
- Commercial testing is available.
- SAG-2, 4/3 ELISA uses the Serum to CSF ratio, and specificity approaches 100%.
- False negatives do occur. This is currently the most widely-used test.
- Multiplex SAG-1, 5, 6 is a horse-side test with high specificity, however the sensitivity is uncertain.
- Indirect Fluorescent Antibody Test (IFAT) is performed on serum or CSF samples (ideal for CSF samples with iatrogenic blood contamination.)
- Western blot identifies antibody against S. neurona.
- Serum testing indicates a 35-70% immunoblot analysis positive rate.
- A seropositive result does not confirm diagnosis, but a seronegative result rules out EPM.
- Detection of a positive CSF indicates intrathecal production of said anitbodies.
- False positives are common.
- Ponazuril (Marquis®) is the first FDA-approved drug for EPM treatment, and it attacks the chloroplast function of the protozoa.
- Diclazuril (Protazil®) is a top-dress pellet.
- Sulfadiazine, pyrimethamine (Rebalance®) must be administered on an empty stomach, and pyrimethamine is a dihydrofolate reductase inhibitor with high affinity for protozoal organisms.
- Complications include colitis, anemia, neutropenia, and abortion; do not use in pregnant mares.
- Support includes sling support, good footing, and a safe environment.
- Most horses improve in 1 to 3 weeks after therapy initiation.
- Prognosis for complete recovery is less than 20%.
- The prognosis is poor if there's recumbency and more favorable for brainstem dysfunction than spinal cord signs.
- To prevent EPM the hay and pasture should not be contaminated with possum feces.
- Contaminated water sources and grain may also be a source for infection. Secure grain and hay, relocate possums, and remove cat, skunk, etc.
Equine Herpes Myeloencephalitis (EHV-1)
- Signalment includes a history of fever 5 to 7 days before neurologic signs onset, with no gender, breed, geographic, or seasonal predilection.
- Aged horses are predisposed to experimental infections.
- The number of outbreaks and morbidity/mortality is on the rise. The USDA designated neuropathic EHV as a "potentially emerging" disease in 2007. and was the subject of the 2009 ACVIM consensus statement.
- Morbidity for developing during an outbreak is 26%.
- Mortaility in horses with neurologic signs is 29%.
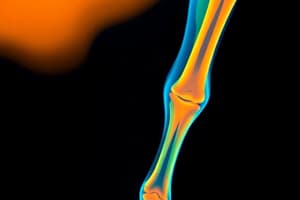
- Symptoms include ascending myelitis, symmetric weakness and ataxia, worse rear limb deficits, poor tail tone, urine dribbling, and prolapsed penis.
- CSF analysis reveals xanthochromia, moderate to marked protein elevation, and normal CSF cell count consisting of small lymphocytes.
- Use Nested PCR (24 hr) and virus isolation to identify the neuropathic strain
- Treatments include isolation from other horses for 21 days of resolution.
- Antiviral therapy of valacyclovir or IV acyclovir are also an option.
- Supportive care of urinary catheterization and sling are also an option.
- Vaccination can reduce the magnitude and duration of viral shedding, which may reduce the spread of infection through premises.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.