Podcast
Questions and Answers
Which of the following is NOT a primary function of the skin?
Which of the following is NOT a primary function of the skin?
- Preventing water loss
- Temperature control
- Defense against environmental factors
- Synthesizing vitamin D (correct)
A patient presents with a skin lesion that is a flat, circumscribed area of color change less than 1 cm in diameter. Which term best describes this lesion?
A patient presents with a skin lesion that is a flat, circumscribed area of color change less than 1 cm in diameter. Which term best describes this lesion?
- Plaque
- Nodule
- Macule (correct)
- Vesicle
Which of the following best describes a vesicle?
Which of the following best describes a vesicle?
- A circumscribed, fluid-filled lesion less than 0.5 cm (correct)
- A large, solid, elevated lesion greater than 1 cm
- A solid, elevated lesion less than 0.5 cm
- A deep, pus-filled lesion
A patient has a cluster of small, itchy bumps that have coalesced into a large, raised area on their arm. The area is greater than 1 cm. Which term accurately describes this skin finding?
A patient has a cluster of small, itchy bumps that have coalesced into a large, raised area on their arm. The area is greater than 1 cm. Which term accurately describes this skin finding?
Which characteristic is most indicative of a wheal?
Which characteristic is most indicative of a wheal?
A patient has a skin lesion with focal loss of the epidermis which doesn't penetrate into the dermis. How should this be classified?
A patient has a skin lesion with focal loss of the epidermis which doesn't penetrate into the dermis. How should this be classified?
A deep, linear split in the skin caused by drying is best described as which type of lesion:
A deep, linear split in the skin caused by drying is best described as which type of lesion:
Which of the following skin lesions is characterized by a collection of dried exudate of serum, pus, or blood on the skin's surface?
Which of the following skin lesions is characterized by a collection of dried exudate of serum, pus, or blood on the skin's surface?
Which of these skin assessment findings is considered a primary lesion?
Which of these skin assessment findings is considered a primary lesion?
What is a key characteristic that differentiates a nodule from a papule?
What is a key characteristic that differentiates a nodule from a papule?
Which of the following bacterial species is NOT typically associated with impetigo?
Which of the following bacterial species is NOT typically associated with impetigo?
A child presents with honey-colored crusted lesions around the nose and mouth. Which treatment is most appropriate for this initial presentation?
A child presents with honey-colored crusted lesions around the nose and mouth. Which treatment is most appropriate for this initial presentation?
What is the recommended approach for treating widespread impetigo with confirmed Methicillin-resistant Staphylococcus aureus(MRSA)?
What is the recommended approach for treating widespread impetigo with confirmed Methicillin-resistant Staphylococcus aureus(MRSA)?
A patient is diagnosed with non-bullous impetigo. Which of the following characteristics is most closely associated with this type of impetigo?
A patient is diagnosed with non-bullous impetigo. Which of the following characteristics is most closely associated with this type of impetigo?
A patient is prescribed mupirocin for a skin infection. Which of the following infections is mupirocin most likely to effectively treat?
A patient is prescribed mupirocin for a skin infection. Which of the following infections is mupirocin most likely to effectively treat?
What is the primary characteristic of folliculitis?
What is the primary characteristic of folliculitis?
A barber presents with folliculitis in their beard area. Which of the following is the likely diagnosis?
A barber presents with folliculitis in their beard area. Which of the following is the likely diagnosis?
A patient presents with a tender, hot, red nodule with central necrosis. Which skin infection is most likely?
A patient presents with a tender, hot, red nodule with central necrosis. Which skin infection is most likely?
Compared to a furuncle, what is a unique characteristic of a carbuncle?
Compared to a furuncle, what is a unique characteristic of a carbuncle?
What is an important factor to consider in the management of recurrent furunculosis?
What is an important factor to consider in the management of recurrent furunculosis?
What is the primary difference in presentation between cellulitis and erysipelas?
What is the primary difference in presentation between cellulitis and erysipelas?
A patient presents with erysipelas and a known penicillin allergy. Which antibiotic would be most appropriate?
A patient presents with erysipelas and a known penicillin allergy. Which antibiotic would be most appropriate?
Which of the following findings would warrant a more aggressive treatment approach for cellulitis, such as intravenous antibiotics?
Which of the following findings would warrant a more aggressive treatment approach for cellulitis, such as intravenous antibiotics?
A patient has superficial bacterial infection in the axilla. The area is itchy with well defined brown patches with superficial scales. What is the likely diagnosis?
A patient has superficial bacterial infection in the axilla. The area is itchy with well defined brown patches with superficial scales. What is the likely diagnosis?
A patient is diagnosed with erythrasma. What is an appropriate first-line topical treatment?
A patient is diagnosed with erythrasma. What is an appropriate first-line topical treatment?
Erythrasma is most commonly associated with which of the following causative agents?
Erythrasma is most commonly associated with which of the following causative agents?
Regarding differentiating cellulitis from deep vein thrombosis (DVT), which of the following is true?
Regarding differentiating cellulitis from deep vein thrombosis (DVT), which of the following is true?
Leprosy is primarily transmitted via:
Leprosy is primarily transmitted via:
Which of the following best describes the primary impact of leprosy on the human body?
Which of the following best describes the primary impact of leprosy on the human body?
A patient with leprosy presents with few skin lesions, strong cell-mediated immunity, and is smear-negative. According to the classification, which type does this patient most likely have?
A patient with leprosy presents with few skin lesions, strong cell-mediated immunity, and is smear-negative. According to the classification, which type does this patient most likely have?
A patient with leprosy has multiple skin lesions, bacterial index +5, and exhibits poor immunity to the bacteria. Which type do they classify as?
A patient with leprosy has multiple skin lesions, bacterial index +5, and exhibits poor immunity to the bacteria. Which type do they classify as?
A patient with tuberculoid leprosy (TT) is most likely to present with:
A patient with tuberculoid leprosy (TT) is most likely to present with:
Which of the following complications is most closely associated with lepromatous leprosy?
Which of the following complications is most closely associated with lepromatous leprosy?
In a patient with leprosy, sensory loss, weakness, facial palsy and a clawed hand all impact the:
In a patient with leprosy, sensory loss, weakness, facial palsy and a clawed hand all impact the:
A patient is diagnosed with Multibacillary (MB) leprosy. What drug combination is indicated for this diagnosis for adults?
A patient is diagnosed with Multibacillary (MB) leprosy. What drug combination is indicated for this diagnosis for adults?
How long does it typically take for leprosy treatment to render a patient non-infectious?
How long does it typically take for leprosy treatment to render a patient non-infectious?
How should a 40 year old with bacterial index +5 be treated? (Rifampicin-600mg Monthly, Dapsone-100mg daily, Clofazimine 300mg monthly/50mg daily)?
How should a 40 year old with bacterial index +5 be treated? (Rifampicin-600mg Monthly, Dapsone-100mg daily, Clofazimine 300mg monthly/50mg daily)?
Dora, is diagnosed with Erythrasa, which choice for treating this disease is inappropriate for preventing re-occurance?
Dora, is diagnosed with Erythrasa, which choice for treating this disease is inappropriate for preventing re-occurance?
Flashcards
Dermatology
Dermatology
The study of the skin, its structure, functions, and diseases.
Epidermis
Epidermis
The outermost layer of the skin, providing a protective barrier.
Dermis
Dermis
The middle layer of the skin, containing blood vessels, nerves, and hair follicles.
Subcutaneous fat
Subcutaneous fat
Signup and view all the flashcards
Macule
Macule
Signup and view all the flashcards
Patch
Patch
Signup and view all the flashcards
Papule
Papule
Signup and view all the flashcards
Nodule
Nodule
Signup and view all the flashcards
Plaque
Plaque
Signup and view all the flashcards
Vesicle
Vesicle
Signup and view all the flashcards
Bulla
Bulla
Signup and view all the flashcards
Wheal
Wheal
Signup and view all the flashcards
Pustule
Pustule
Signup and view all the flashcards
Crusts
Crusts
Signup and view all the flashcards
Erosion
Erosion
Signup and view all the flashcards
Ulcer
Ulcer
Signup and view all the flashcards
Fissure
Fissure
Signup and view all the flashcards
Scar
Scar
Signup and view all the flashcards
Impetigo
Impetigo
Signup and view all the flashcards
Non Bullous Impetigo
Non Bullous Impetigo
Signup and view all the flashcards
Bullous Impetigo
Bullous Impetigo
Signup and view all the flashcards
Ecthyma
Ecthyma
Signup and view all the flashcards
Mild cases
Mild cases
Signup and view all the flashcards
widespread impetigo or severe cases
widespread impetigo or severe cases
Signup and view all the flashcards
Folliculitis
Folliculitis
Signup and view all the flashcards
Sycosis barbae
Sycosis barbae
Signup and view all the flashcards
Furuncle
Furuncle
Signup and view all the flashcards
Carbuncle
Carbuncle
Signup and view all the flashcards
Erysipelas & cellulites
Erysipelas & cellulites
Signup and view all the flashcards
Erysipelas
Erysipelas
Signup and view all the flashcards
cellulitis
cellulitis
Signup and view all the flashcards
Erythrasma
Erythrasma
Signup and view all the flashcards
Leprosy
Leprosy
Signup and view all the flashcards
Bacteriological classification
Bacteriological classification
Signup and view all the flashcards
Paucibacillary leprosy
Paucibacillary leprosy
Signup and view all the flashcards
Multibacillary leprosy
Multibacillary leprosy
Signup and view all the flashcards
Lepromatous leprosy
Lepromatous leprosy
Signup and view all the flashcards
Characteristic lesion of tuberculoid leprosy (TT)
Characteristic lesion of tuberculoid leprosy (TT)
Signup and view all the flashcards
Study Notes
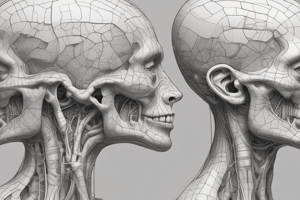
Skin Histology
- Skin is composed of 3 layers: Epidermis, Dermis, and Subcutaneous fat
- Other parts include hair shaft, sweat gland, sebaceous gland, arrector pili muscle, hair bulb and dermal papilla
Skin Function
- Aspect to the world
- Holds the structures together
- Prevents water loss
- Defends against environment
- Temperature control
- Barrier against micro-organisms
- Skin sensations
- Disease occurs when there is impairment of the normal function or structure
Skin Patient - Important Considerations
- When examining skin patients, take history and ensure standard approach
- Examination involves: inspection (lesional and whole skin), nails and har, palpation, regional LN (lymph node)
- Four aspects of looking at lesions are: morphology, shape, distribution and color
Primary Lesions
- Macule or patch; flat lesions- macule is <1cm whereas patch is >1cm
- Papule or nodule; skin lesion
- Vesicle or Bulla; skin lesion
- Wheal is the primary lesion of urticaria
- Burrow is the primary lesion of scabies and a linear elevation of the epidermis
- Plaque describes changes in texture and can be elevated or depressed
- Originates de novo or results from confluence of multiple papules, has a large surface area compared to its height
Secondary Lesions
- Include crust, furrow, pustule, excoriation, abrasion, erosion, fissure, ulcer
Morphology: Macule
- Described as circumscribed color change with no elevation or depression in any shape, and <1 cm in size
Morphology: Patch
- Patch has circumscribed color change with no elevation or depression in any shape, and >1 cm in size
Morphology: Papule
- This is a solid elevated lesion, flat pointed or rounded and less than 0.5cm
- Can coalesce into plaque
Morphology: Nodule
- Described as circumscribed solid elevation that is epidermal, dermal or SC
- Variable shaped measuring greater than 0.5cm in size
Morphology: Plaque
- Characterised as having a circumscribed solid elevation that is usually flat-topped, with surface area greater than height
- Measures greater than 1cm
Morphology: Vesicle
- A circumscribed, fluid-filled elevated lesion that measures less than 0.5cm
Morphology: Bulla
- A circumscribed, fluid-filled elevated lesion that measures greater than 0.5cm
Morphology: Wheal
- Characterized by edematous elevation that is itchy, variable in size and evanescent
- Diagnostic of urticaria
Morphology: Pustule
- Described as having either a vesicle or bulla containing pus
- Cream, yellow or green in color; and may or may not be sterile
- Varies in size and shape
Morphology: Scales
- Laminated masses of keratin, dry or greasy.
- Overly macule, papule or plaque
Morphology: Crusts
- Collection of debris on the the skins surface that is a dried exudate of serum, pus, or blood, also described as a scab
Morphology: Erosions
- Focal loss of epidermis with partial or total thickness, doesn’t penetrate into the dermis
- Heals without scarring
Morphology: Ulcer
- Focal loss of epidermis and dermis, that has variable shape, size and depth
- Penetrates into dermis, and heals with scarring
Morphology: Fissure
- A deep linear split in the skin often caused by drying, penetrates into dermis
Morphology: Scar
- Replacement fibrosis of the skin that results from destructive processes
Bacterial Infections - Overview
- Divided according causative agents that include Staphylococcus aureus, Corynebacterium minutissimum, and Streptococcus pyogen
Staphylococcus aureus
- Causes Impetigo, Folliculitis, Sycosis barbea, Furuncles, and Carbunculs
Corynebacterium minutissimum
- Causes Erythrasma
Streptococcus pyogen
- Causes Erysipelas, Cellulites, and Impetigo
Sensitivity to Antibiotics
- Topical antibiotics include Fusidic acid and mupirocin work for both Staph. aureus and Strep. pyogenes
- Neomycin works only with Staph. aureus
- Gentamicin not effective against Strep. pyogenes
Systemic Antibiotics
- Flucloxacilline and Erythromycin are effective against Staph. aureus and Strep. pyogenes
MRSA - Considerations
- Vancomycin can be used for MRSA Infections
- Linezolides considered more effective
Corynebacterium minutissimum - Topical Treatment
- Azol antifungal (miconazol & fluconazole), fucidic acid or mupriocin are Topical treatments
Corynebacterium minutissimum - Systemic Treatment
- Erythromycin & Tetracycline are Systemic treatments
Impetigo
- Superficial skin infection commonly seen in children and transmitted easily from person to another
- Caused by bacterial infection by Streptococci (developing countries) or Staphylococci (major pathogen)
- Primary cause: poor hygiene and moisture (common during summer)
- Secondary cause: insect bite, scabies, or scratch
- CBC is common
- Lesions are rarely painful but are pruritic
Types of Impetigo: Non Bullous
- Common in children; it is very contagious with a macule-vesicle-rupture with seropurulent discharge, or a honey-colored crust
Types of Impetigo: Bullous
- Most common in children under age two
- Larger blisters with larger bases/honey-colored crust.
- Fetal in new born infants, caused by S. aureus capable of producing exfoliative toxins
- Site: Trundk
Types of Impetigo: Ecthyma
- Serious form of impetigo affecting the second layer of the skin (painful)
- Ulcers with raised edges with necrotic crustation in the center; thick brown-black crust
- Heal with scar
Impetigo Treatment Considerations
- Antimicrobial treatment is indicated to relieve symptoms, prevent formation of new lesions, and prevent complications like cellulitis
- Topical local therapy requires removing of crust by water and soap
Impetigo Treatment - Mild Cases
- Topical antibiotic as fusidic acid cream 3 times (7-10 days)
- Mupirocin cream is effective if the cause of infection is MRSA
Impetigo Treatment - Widespread/Severe Cases
- Systemic antibiotics (penicillin, dicloxacillin flucloxacillin, cephalexin) are effective
- Azithromycin, Erythromycin and clindamycin effective in case of penicillin allergy.
- Clindamycin is given 300 mg every 6 hours for 7 days in adults, or 10-20 mg/kg every 8 hours for 7 days in children
- Trimethoprim-sulfamethoxazole is given 160 mg twice a day for 7 days in adults, or 8-12 mg/kg twice daily for 7 days in infants > 2 months
- Doxycycline is given 100 mg twice daily for 7 days in patients > 45 kg, and should not be given to children and pregnant women
Topical Treatments: First-Line Treatment For Impetigo
- Topical: Mupirocin 3 times for 7-10 days, bacitracin, fusidic acid.
- Topical Potassium permanganate 1/8000
Systemic Treatments: First-Line Treatment For Impetigo
- Dicloxacillin Penicillinase resistance penicillin for dosage 250-500 mg PO qid for 5-7 days
- Amoxicillin plus clavulanic acid; cephalexin for 25 mg/kg PO tid, and 250-500 mg PO qid for 10 days
Systemic Treatments: Second-Line Treatment (Penicillin allergy) For Impetigo
- Clindamycin or doxycycline is preferred for MRSA or if penicillin allergy,
- Azithromycin: 500 mg PO × 1, and later 250 my PO daily for 4 days
- Clindamycin: 15 mg/kg/day PO tid for 7 days
- Erythromycin: 250-500 mg PO qid for 5-7 days
Ecthyma Treatments - Key Actions
- Topical treatments: Warm compresses qid
- Systemic treatments: Dicloxacillin at 250-500 mg PO qid for 5-7 days
Ecthyma Treatments -Amoxicillin
- Amoxicillin plus clavulanic acid at 25 mg/kg PO tid
- Cephalexin at 40-50 mg/kg/day PO for 10 days
Ecthyma Treatments (Penicillin Allergy)
- Use azithromycin at 500 mg PO × 1, then 250 mg PO daily for 4 days
- Clindamycin at 15 mg/kg/day PO tid for 10 days
- Erythromycin at 250-500 mg PO qid for 5-7 days
Folliculitis
- Superficial Pruritic Pustule around the upper part of hair follicle (ostium) & discrete (inflammation of hair follicles)
- Caused Staphylococcus aures
- Non-bacterial causes are shaving, waxing, wearing tight clothes or hair styling practices such as wigs and oils
Folliculitis - Other Considerations
- Steroid use, tight clothes, rubber gloves, boots that don't let sweat or heat out
- Poor hygiene , moisture, diabetes and HIV are risk factors
Folliculitis Treatments - Notes
- Identical to treatments for impetigo
Folliculitis Treatments - First Line
- Use fusidic acid, Bacitracin, clindamycin and Mupirocin topically between 5-7 days
- Apply warm compresses to promote drainage, Potassium permanganate 1\8000
- Antiseptic wash (chlorhexidine) bid
Folliculitis Treatments - Next Steps
- Flucloxacillin, penicillin, Dicloxacillin, only if widespread or severe and use Doycycline (2-8 weeks) for MRSA
- If recurrent: eradicate S. aureus carriage (Mupirocin applied to nostrils and chlorhexidine wash, both daily for 5 days)
Sycosis Barbae
- Follicular pustules and papules in beard area
- caused by staphylococcus aures
- risk factors include poor hygiene, moisture and shaving
Furuncle
- Described as a peri-follicular, tender, hot, red nodule or pustule
- Deep infection in lower part hair follicle, with central necrosis
- More common in adults and carrier states.
- Obesity + DM are risk factors
- Important to exclude diabetes is in recurrent furunculosis
Carbuncle - Overview
- Affect multiple hair follicles beside each other.
- Furuncle coalesce into a fistula
- Occur in back, neck and intertriginous area
- DM + Obesity + prolonged use of corticosteroid are risk factors
- Systemic antibiotic + control the cause
Furuncle Treatments - First Line
- Incision and drainage should be avoided along with sqeezing,
- Apply warm compression that is indicated to facilitate drainage of small furuncles
- Large furuncles require incision and drainage, use dicloxacillin or flucloxacillin and Amoxicillin plus calvulanic acid; cephalexin, and duration of treatment is 1-2 weeks
Furuncle Treatments - Considerations
- Immunocompromised patients and severe infections or abscesses in patients who fail incision and drainage, plus oral antibiotics
- Treat empirically with parenteral vancomycin, daptomycin, linezolid, or ceftaroline
Recurrent Furunculosis Management
- Staphylococcus in the anterior nares, nasal swabs be be taken for culture and sensitivity
- Apply Mupirocin cream 2%, three times daily to eliminate nasal carriers of staphylococcus
- Exclude diabetes in recurrent furunculosis, use instructions of hygienic washing of hands, and clean lines
- Start Systemic Rifampicin that is effective in recurrent furunculosis with a dose of 600 mg daily for 1 week each month for 3 months
- Ciprofloxacillin or clindamycin are also used
Erysipelas - Overview
- Swallow erythema inflammation and hotness, with sharp border
- DM, and immunocompromised patients are risk factors
- Cellulites have an ill-defined border
Cellulities and Erysipelas
- Cellulitis results in inflammation of lower dermis and SC tissue with Staph aureus (purulent )and Streptococcus pyogenes whereas Erysipelas is of the upper dermis cause by ẞ hemolytic streptococci
- Patients mention burning pain
- Clinical Picture: face and leg commonly affected/red non-edematous for erysipelas, and for cellulitis commonly affect lower limbs/ pink edematous
Treatments for Cellulitis and Erysipelas Considerations
- Provide symptomatic treatment pain and fever and Underlying predisposing conditions, should be identified like diabetes, for sinus infection to prevents recurrences (in facial erysipelas)
- Prompt systemic Antibiotics if the infection is deep and Oral penicillin is to be given for uncomplicated mild cases, and IV therapy for systemic toxicity
- Consider Amoxicillin and clavulanic acid is if there is evidence of sinus infection
Treatments for Cellulitis and Erysipelas Steps
- Penicillin resistant infection suspected, use clindamycin or substitute with intravenous linezolid
- For severe cellulitis and erysipelas due to MRSA, vancomycin is needed.
- For mild cases it is needed between 5-10 days and Complicated cases, 10-20 days is required
Strategy for Cellulitis and Erysipelas Treatment
- MILD, no evidence of systemic signs or symptoms, and Well-controlled: use Cephalexin, Penicillin VK, and Dicloxacillin oral
- MODERATE for evidence of systemic signs: Cefazolin or Ceftriaxone IV medications
- SEVERE if Presences of SIRS with altered mentation, toxic appearance: Vancomycin+/-,Piperacillin/Tazobactam,Meropenem/Imipenem, and Linezolid IV methods
Cellulitis and Erysipelas Treatments - Additional Factors
- Both these illnesses treated with outpatient therapy
- Hospitalize patients with systemic inflammatory response syndrome (SIRS) for temperature, tachypnea or tachycardia and abscess.
- Use Low-dose antibiotic prophylaxis with penicillin v 250 mg twice daily for 5-7 days every month for 12 months
- Consider I.M benzathine penicillin once a month for 12 months
Erythrasma
- Itchy, Irregular but well defined brown patch with superficial scales and found in intertrigenios area, axilla , groin, sub mammary area.
- Mild, chronic and superficial bacterial infection and the DD is tinea cruris and candida infection
- Superficial infection with corynebacterium minutissimum in intertriginous area (Obesity + DM, Heat, Moisture + poor hygiene)
Erythrasma Treatments
- Topical include fusidic acid, clindamycin, mupirocin antibiotic agents with antifungul Azole derivatives
- Systemic for severe discrete cases uses Erythromycin at 250 mg 4 times daily for 14 days,
- Tetracycline, and Single 1 g clarithromycin dose
Case 1 - Male 40. Erythema left leg, well demarcated, chills and malaise. Diagnoses?
- Erysipelas, difficult to differentiate between cellulitis and Erysipelas
Case 1 - Male 40. How to treat cellulitis with erythema?
- IV antibiotic over 5 - 10 days
Case 1 - What if patient has Penicillin Allergy? what is the treatment?
- Use clindamycin 600 mg 8 hourly IV
Case 1 - What if the patient doesn't get treated? Complications?
- Possibilities include subcutaneous and septicemia.
Case 1 - How do you know the patient has Erysipleas vs DVT?
- Doppler ultrasound examination may be helpful,
- Protein levels higher in cellulitis
Case 2 - Jan is 12 , thin walled vesicle face
- Thin walled vesicle = Imetigo, the treatment would be systemic antibiotic , Topical antiseptic.
- Possible Glomerulonephritis as a compication.
Case 3 - Dora 23 years old women with patch scaly, reddish-brown
- Diagnoses - Enthrasama, and uses azyol agents.
- Long term pordone iodine, drying agents to help prevention.
Leprosy: Overview
- Also known as Hansen's Disease, a chronic, granulomatous infection caused by Mycobacterium leprae, bacterium related the bacteria causing tuberculosis.
- Affects skin and nerves and transmitted mostly through nasal mucosa by droplets or wounds and
- Through nasal mucosa to site of macrophages (intracellular
Leprosy: Key Symptoms
- Sensory Hypothesia, Motor Weakness, facial palsy and Autonomic Decreased Sweating and hyperpigmentation
Classification
- Bacteriological consists of Paucibacillary leprosy or Boroder line, whereas Clinical Consists Of Lepromatous and Border Lin
Leprosy Spectrum
- Paucibacillary has Better Immunity and Multibacillary Leprosy has bad.
Tuburcoid Leprosy
- Characteristic nerve enlargement + Skin of nervial area.
- Good immunity, not highly contagious
Lepromatous Leprosy
- Good immunity, no highly contagiois only if untreated and released into air.
Leprosy - Treatment
- PB including SLBP or rifampcin, and should be 6 months.
- Treat at lease -2 years
Case STudy: MAle with 5+
- Best treatment, MB with 12 motnhs of treatment.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.