Podcast
Questions and Answers
Which of the following best describes the role of the dermis in the context of skin anatomy?
Which of the following best describes the role of the dermis in the context of skin anatomy?
- It is the outermost layer of the skin, directly exposed to the environment.
- It is composed of subcutaneous tissue, fascia, muscle, and tendons.
- It provides skin flexibility and strength. (correct)
- It primarily provides protection against trauma and harmful organisms.
In the normal wound healing process, which of the following occurs during the inflammatory/hemostatic phase?
In the normal wound healing process, which of the following occurs during the inflammatory/hemostatic phase?
- Vasoconstriction and haemostasis. (correct)
- Angiogenesis and granulation tissue formation.
- Extracellular matrix formation.
- Re-epithelialization.
A patient presents with a wound that is described as having skin loss involving the epidermis and dermis with a shallow crater. Which depth of injury does this best describe?
A patient presents with a wound that is described as having skin loss involving the epidermis and dermis with a shallow crater. Which depth of injury does this best describe?
- Full-thickness
- Superficial-thickness
- Partial-thickness (correct)
- Deep-thickness
Which of the following factors would most likely impair wound healing?
Which of the following factors would most likely impair wound healing?
Which of the following clinical signs is indicative of a local wound infection?
Which of the following clinical signs is indicative of a local wound infection?
A patient has a laceration on their arm that is 3 cm long. When should this patient be referred for further medical treatment?
A patient has a laceration on their arm that is 3 cm long. When should this patient be referred for further medical treatment?
What is the immediate next step in treating a minor acute wound?
What is the immediate next step in treating a minor acute wound?
Why is it important to choose a dressing that provides a moist, but not wet, environment for a wound?
Why is it important to choose a dressing that provides a moist, but not wet, environment for a wound?
Which dressing material is most appropriate/indicated for wounds with high exudate?
Which dressing material is most appropriate/indicated for wounds with high exudate?
A patient is prescribed silver sulfadiazine cream to help prevent burn wound infections. What is the most appropriate counseling point to provide?
A patient is prescribed silver sulfadiazine cream to help prevent burn wound infections. What is the most appropriate counseling point to provide?
What is the MOST common cause of burns?
What is the MOST common cause of burns?
Which of the following is the MOST accurate in describing the pathophysiology of a burn in the 'zone of stasis'?
Which of the following is the MOST accurate in describing the pathophysiology of a burn in the 'zone of stasis'?
What burn depth best describes a burn that is dry, waxy, variable in color, with blisters that may develop and does NOT blanche?
What burn depth best describes a burn that is dry, waxy, variable in color, with blisters that may develop and does NOT blanche?
A patient is burned and has circumferential eschar on their arm. Why is this concerning?
A patient is burned and has circumferential eschar on their arm. Why is this concerning?
Which of the following patients presenting with a burn requires referral?
Which of the following patients presenting with a burn requires referral?
What should you counsel a patient with superficial burn to immediately do?
What should you counsel a patient with superficial burn to immediately do?
What is the first line pharmacologic option recommended in burn patients?
What is the first line pharmacologic option recommended in burn patients?
Which is the best description of pressure injuries?
Which is the best description of pressure injuries?
Which of the following risk factors is MOST associated with the development of a pressure injury?
Which of the following risk factors is MOST associated with the development of a pressure injury?
Why is muscle more susceptible to ischemia than skin when external compression occurs?
Why is muscle more susceptible to ischemia than skin when external compression occurs?
What is the best description of a Stage 1 Pressure Injury?
What is the best description of a Stage 1 Pressure Injury?
Which pressure injury stage exhibits a deep lesion with a crater-like shape, where slough or necrotic tissue may be visible?
Which pressure injury stage exhibits a deep lesion with a crater-like shape, where slough or necrotic tissue may be visible?
Which of the following is the MOST important strategy in preventing pressure injuries?
Which of the following is the MOST important strategy in preventing pressure injuries?
Aside from proper preventative measures, what is a treatment step to consider when seeing a patient showing possible signs and symptoms of pressure injuries?
Aside from proper preventative measures, what is a treatment step to consider when seeing a patient showing possible signs and symptoms of pressure injuries?
Which description best describes why you should generally clean a wound using typical tap water or a normal saline solution?
Which description best describes why you should generally clean a wound using typical tap water or a normal saline solution?
If you have a patient who is a chronic wound and has a high necrotic burden, what treatment should be administered?
If you have a patient who is a chronic wound and has a high necrotic burden, what treatment should be administered?
A patient is experiencing increased warmth, foul odor, fever and elevated WBC count. What is most likely happening in the patient?
A patient is experiencing increased warmth, foul odor, fever and elevated WBC count. What is most likely happening in the patient?
Which of the the following is NOT a sign of local wound infection?
Which of the the following is NOT a sign of local wound infection?
A patient has a partial thickness burn with some small blisters, blanches upon pressure and reports pain. What is the recommended treatment?
A patient has a partial thickness burn with some small blisters, blanches upon pressure and reports pain. What is the recommended treatment?
If you have a burn that covers more than 10% of a patient with no thin skin involved, are they required to be referred?
If you have a burn that covers more than 10% of a patient with no thin skin involved, are they required to be referred?
Upon assessing a patient who has non-blanchable erythema, what management should be aimed at?
Upon assessing a patient who has non-blanchable erythema, what management should be aimed at?
In what direction does damage occur on a pressure injury?
In what direction does damage occur on a pressure injury?
What cells would you most likely not see in wound healing?
What cells would you most likely not see in wound healing?
A researcher is trying to recreate the maturation phase of wound healing in vitro. What component is essential to incorporate?
A researcher is trying to recreate the maturation phase of wound healing in vitro. What component is essential to incorporate?
A researcher is investigating new wound healing approaches by removing foreign material from a wound. What process is the researcher most likely targeting?
A researcher is investigating new wound healing approaches by removing foreign material from a wound. What process is the researcher most likely targeting?
What classification is Osteomyelitis?
What classification is Osteomyelitis?
A researcher has found that matrix metalloproteinases (MMPs) in their treatment group have increased. What phase of wound healing would this be found in?
A researcher has found that matrix metalloproteinases (MMPs) in their treatment group have increased. What phase of wound healing would this be found in?
A patient with a minor laceration reports that the bleeding has not stopped after 15 minutes despite continuous direct pressure, you also observe that the wound edges do not stay together. What is the MOST appropriate course of action?
A patient with a minor laceration reports that the bleeding has not stopped after 15 minutes despite continuous direct pressure, you also observe that the wound edges do not stay together. What is the MOST appropriate course of action?
A patient is prescribed silver sulfadiazine cream for a partial thickness burn, but the pharmacist notices the patient also has a sulfa allergy. What is the MOST appropriate course of action?
A patient is prescribed silver sulfadiazine cream for a partial thickness burn, but the pharmacist notices the patient also has a sulfa allergy. What is the MOST appropriate course of action?
In assessing a patient at risk for pressure injuries, the healthcare provider notes an area of intact skin with persistent redness that does not blanch when pressed. The patient denies any pain or discomfort in the area. What stage of pressure injury corresponds with these findings?
In assessing a patient at risk for pressure injuries, the healthcare provider notes an area of intact skin with persistent redness that does not blanch when pressed. The patient denies any pain or discomfort in the area. What stage of pressure injury corresponds with these findings?
Which dressing would provide the MOST appropriate initial management for a wound characterized by a high level of exudate, while still promoting a moist wound environment?
Which dressing would provide the MOST appropriate initial management for a wound characterized by a high level of exudate, while still promoting a moist wound environment?
A patient with a burn injury is being assessed shortly after the incident. Which of the following findings would require referral to a higher level of care?
A patient with a burn injury is being assessed shortly after the incident. Which of the following findings would require referral to a higher level of care?
Flashcards
What is a wound?
What is a wound?
A disruption in normal skin structure/function due to mechanical trauma or injury.
What is an acute wound?
What is an acute wound?
Caused by burns, bites, abrasions, scrapes, minor lacerations and punctures, minor surgical procedures; Heals within ~3 weeks.
What is a chronic wound?
What is a chronic wound?
Healing delayed or impaired; Healing has not proceeded through the healing process correctly.
What is a superficial-thickness wound?
What is a superficial-thickness wound?
Signup and view all the flashcards
What is a partial-thickness wound?
What is a partial-thickness wound?
Signup and view all the flashcards
What is a full-thickness wound?
What is a full-thickness wound?
Signup and view all the flashcards
How does diabetes affect wound healing?
How does diabetes affect wound healing?
Signup and view all the flashcards
How does infection affect wound healing?
How does infection affect wound healing?
Signup and view all the flashcards
How do nutritional problems affect wound healing?
How do nutritional problems affect wound healing?
Signup and view all the flashcards
How does excessive tension affect wound healing?
How does excessive tension affect wound healing?
Signup and view all the flashcards
How does 'another wound' affect wound healing?
How does 'another wound' affect wound healing?
Signup and view all the flashcards
How does low temperature affect wound healing?
How does low temperature affect wound healing?
Signup and view all the flashcards
How does Epidermis Depth of Injury affect wound healing?
How does Epidermis Depth of Injury affect wound healing?
Signup and view all the flashcards
How does Dermis Depth of Injury affect wound healing?
How does Dermis Depth of Injury affect wound healing?
Signup and view all the flashcards
How does Arterial Blood Depth of Injury affect wound healing?
How does Arterial Blood Depth of Injury affect wound healing?
Signup and view all the flashcards
How does Venous Blood Depth of Injury affect wound healing?
How does Venous Blood Depth of Injury affect wound healing?
Signup and view all the flashcards
How does Subcutaneous Tissue Depth of Injury affect wound healing?
How does Subcutaneous Tissue Depth of Injury affect wound healing?
Signup and view all the flashcards
Basic wound treatment principles?
Basic wound treatment principles?
Signup and view all the flashcards
Signs of local wound infection?
Signs of local wound infection?
Signup and view all the flashcards
Signs of systemic wound infection?
Signs of systemic wound infection?
Signup and view all the flashcards
When to refer a wound for vaccination?
When to refer a wound for vaccination?
Signup and view all the flashcards
When to refer burns for medical attention?
When to refer burns for medical attention?
Signup and view all the flashcards
What is a burn?
What is a burn?
Signup and view all the flashcards
Thermal: what causes burns?
Thermal: what causes burns?
Signup and view all the flashcards
Radiation: what causes burns?
Radiation: what causes burns?
Signup and view all the flashcards
Electrical: what causes burns?
Electrical: what causes burns?
Signup and view all the flashcards
Chemical: what causes burns?
Chemical: what causes burns?
Signup and view all the flashcards
Factors affecting burn severity?
Factors affecting burn severity?
Signup and view all the flashcards
Patient factors affecting burn severity?
Patient factors affecting burn severity?
Signup and view all the flashcards
What is Coagulation zone?
What is Coagulation zone?
Signup and view all the flashcards
What is Stasis Zone?
What is Stasis Zone?
Signup and view all the flashcards
What is Hyperemia zone?
What is Hyperemia zone?
Signup and view all the flashcards
Superficial, 1st Degree Burn?
Superficial, 1st Degree Burn?
Signup and view all the flashcards
Superficial Partial Thickness, 2nd Degree?
Superficial Partial Thickness, 2nd Degree?
Signup and view all the flashcards
Deep Partial Thickness 2nd Degree Burn?
Deep Partial Thickness 2nd Degree Burn?
Signup and view all the flashcards
Full Thickness, 3rd Degree Burn?
Full Thickness, 3rd Degree Burn?
Signup and view all the flashcards
Complications of local infection?
Complications of local infection?
Signup and view all the flashcards
What is a contracture?
What is a contracture?
Signup and view all the flashcards
What is Eschar?
What is Eschar?
Signup and view all the flashcards
What is TBSA in relation to RED FLAGS of when to refer?
What is TBSA in relation to RED FLAGS of when to refer?
Signup and view all the flashcards
What is Severity of Burns in relation to RED FLAGS of when to refer?
What is Severity of Burns in relation to RED FLAGS of when to refer?
Signup and view all the flashcards
What is Age of Burns in relation to RED FLAGS of when to refer?
What is Age of Burns in relation to RED FLAGS of when to refer?
Signup and view all the flashcards
What is Location of Burns in relation to RED FLAGS of when to refer?
What is Location of Burns in relation to RED FLAGS of when to refer?
Signup and view all the flashcards
What is Concomitant trauma of Burns in relation to RED FLAGS of when to refer?
What is Concomitant trauma of Burns in relation to RED FLAGS of when to refer?
Signup and view all the flashcards
How to manage pressure injuries?
How to manage pressure injuries?
Signup and view all the flashcards
Study Notes
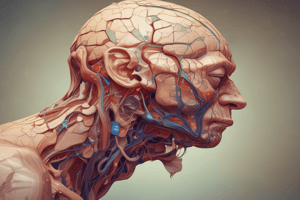
Anatomy of the Skin
- The epidermis is 0.5mm - 6mm thick and provides protection
- The dermis is 0.3 to 4.0 mm thick and provides skin flexibility and strength
- Underlying structures include subcutaneous tissue, fascia, muscle, and tendons
Normal Healing Process
- Wound healing begins at the moment of injury
- Wound healing is described as the physiological process which restores the function of the damaged tissue
- Wound healing occurs in three phases:
- Inflammatory/Hemostatic phase
- Proliferative/Tissue formation/Granulation phase
- Maturation/Tissue remodeling phase
Wound Assessment
- Wound assessment should determine the impact of trauma and the depth or degree of the injury
- Wound assessment may involve describing the thickness of the injury
- A break in the skin, bruising, induration, bogginess, and changes to skin turgor can indicate deep tissue damage
- Assess the presence of any foreign bodies
- Assess the quality of the wound bed including the presence of necrotic tissue, moisture balance and bacterial burden
- Acute wounds are caused by burns, bites, abrasions, scrapes, minor lacerations, and punctures, minor surgical procedures, and heal within ~3 weeks
- Chronic wounds have delayed or impaired healing that has not proceeded through the healing process correctly
Depth of Injury
- Superficial-thickness involves skin loss that only affects the epidermis, and may present as an abrasion or blister
- Partial-thickness involves skin loss that affects the epidermis or dermis (or both) and may present as a shallow crater
- Full-thickness skin loss is the result of extensive destruction, tissue necrosis, or damage to underlying structures such as muscle, tendon, or bone, may present as a deep crater and may tunnel into surrounding subcutaneous tissue.
- Abrasion occurs if epidermis is damaged
- Bleeding occurs and the body's first line of defense is breached, and healing is multifactorial
- Poor arterial flow leads to ischemia and impaired healing
- Venous hypertension leads to edema and interferes with healing
- Lymphedema often accompanies venous edema, it is rarely acknowledged and poorly understood
- Poorly vascularized tissue leads to slow healing
- Entry into the fascial plane leads to infection
- Muscles are very vascular and tear easily
- Exposed tendons and ligaments should be kept moist and are poorly vascularized and therefore slow to heal
- Exposed bone usually leads to osteomyelitis, and bone (periosteum) should not be allowed to dry out
Patient Assessment
- Identify what puts the patient at risk for wounds and/or how their wound developed
- Have the patient describe how it started, how it evolved, and what has made it better or worse
- The health of the patient, patient co-morbidities that increase the risk for skin breakdown, interfere with healing and/or impair immunity should be identified
- Note drug history and known allergies and sensitivities, lifestyle choices, and level of physical function
Factors Leading to Impaired Wound Healing
- Diabetes: the long-term effects of diabetes impair wound healing due to diminished sensation and circulation
- Infection: bacteria compete with fibroblasts for oxygen, delaying collagen synthesis. 12 Infection prolongs the duration of the inflammatory process, which delays wound healing
- Drugs: Corticosteroids generally inhibit cell growth and decrease the inflammatory process.
- Anti-metabolites impede proliferation of fibroblasts and collagen synthesis
- Anticoagulants impede clot formation and delay wound healing
- Nutritional problems: Protein-calorie malnutrition & deficiencies of zinc/vitamins A or C impair normal healing mechanisms
- Tissue necrosis: This results from local or systemic ischemia or radiation injury
- Hypoxia: Inadequate tissue oxygenation impairs wound healing
- Excessive tension on wound edges: tension due to factors can lead to local tissue ischemia and necrosis
- Another wound: competition between several healing areas for the substrates required for wound healing impairs healing at all sites
- Low temperature: The relatively low tissue temperature in the distal aspects of the upper and lower extremities is responsible for slower healing of wounds at these sites
- Other factors include: ischemia, foreign bodies (including necrotic tissue, age (epidermis and subcutaneous layer become thinner), hypothermia and pain, major trauma and burns, hematologic abnormalities (e.g., HIV), sepsis, organ failure, edema/elevated pressure, smoking, ionizing radiation and chemotherapy, and hypothyroidism
Complications of Impaired Wound Healing
- Infection
- Scarring
- Pain and discomfort
- Decreased mobility
- Decrease in quality of life
- Death
- Cost
- Signs of Local Infection: red, puffy/swollen areas around the wound that are tender to touch, red streaks coming from the wound, throbbing pain in the wound area, pus (creamy yellowish-grey fluid) in the wound
- Signs of Systemic infection: fever, chills, malaise or tender lumps or swelling in the armpit, groin or neck
- Complications of infection: osteomyelitis, bacteremia, gangrene and the possibility of amputation
When to Refer
- If a tetanus shot is needed
- Size: Longer than two centimeters
- Location: Lacerations on the face or hands where the edges of the skin do not fall together are present (stitches may be required)
- The wound is reaching fat tissue, muscle or bone
- Prolonged Bleeding does not cease after 10 minutes of pressure
- Contamination: Dirt or debris cannot be removed without scrubbing
- Cause: bites (animal or human)
- If it is not healed after three weeks or the patient is at risk of delayed healing (comorbidities)
- Infection signs are present
- Second- or third-degree burns that require medical attention (usually accompanied by blisters) are present
- If a burn has occurred in a child
- Other: The patient is unable to move the injured body part or is causing severe pain
Treatment of Acute Minor Wounds
- Stop the bleeding
- Cleanse
- Protect
- If there is pain, recommend an appropriate OTC option
Wound Management
- Stop the bleeding by covering with a clean dressing and apply pressure for 10 minutes and refer the patient if bleeding does not stop in 10 minutes (*15 minutes)
- Cleanse the wound, remove dirt and debris, and wash thoroughly (once*)
- The choice of cleansing/antiseptic agent is soap and water or normal saline
- Topical antiseptics should be reserved for non-healable wounds or when local bacterial burden is a concern or the use of:
- Isopropryl alcohol (70-90%)
- Hydrogen peroxide (3%)
- Iodine
- Protect (and Heal) by covering the wound to prevent infection/promote moist wound healing/prevent contamination
- Antibiotics are typically unnecessary; If kept clean the wound should heal in 4-14 days
- Close uninfected cuts/lacerations smaller than two centimeters (not on the face or hands) using a skin adhesive such as a cyanoacrylate or butterfly strips
- Debridement = removal of foreign material from a wound, such as dead or contaminated tissue which can harbor bacteria or autolytic debridement, which occurs naturally or is performed by a trained HCP
Choosing Dressings
- A dressing should have the traits of providing a moist environment (not wet), which accelerates epidermal migration and dermal repair
- The dressing should be able to provide thermal insulation and be highly absorptive
- A dressing should also be impermeable to bacteria while being free of contaminants, nonadherent, and nontoxic
Types of Dressings
- Physical
- Act as an absorbent and protectant
- Gauze (+ tape), Bandages
- Medicated
- Impregnated with various agents such as antiseptics or antibiotics
- Protective
- Perform other functions than simply provide a physical barrier
- Some act as tissue adhesives, absorbents for exudate and wound debridement agents
Topical Antibacterial Agents
- For prophylaxis, topical antibiotics are used if there is a high risk of infection or on nonhealing chronic wounds
- Systemic agents are used in cases of bites, deep punctures, or wounds on the palms or fingers
- Mupirocin is the treatment of choice for topical colonization
Monitoring
- Monitor bleeding, should stop within 10 min (15 min if on anticoagulants)
Endpoint:
- Bleeding significantly slows or stops within 10-15 min of direct pressure Action:
- Emergency medical if blood is spurting or significant bleeding persists with direct pressure
- Monitor daily at dressing change for at least 48 h if there is an infection
- Endpoint: no signs or symptoms of infection present at 48 h Action:
- Refer if signs/symptoms of infection are present at or before 48 h
- Monitor daily at dressing change for 4-14 days (depending on wound type, depth and location) for wound healing
Endpoint:
- Normally, healing wounds appear pink or red with tiny opalescent islands of epithelium throughout and no drainage Action:
- Refer if wound continues to weep, remains raw and red, or does not appear to be closing within 2–4 wk
Terminology of Burns
- A burn is an injury to the skin of other organic tissue primarily caused by heat or due to radiation, radioactivity, electricity, friction or chemicals
Causes of Burns
- Thermal: flames, scalding liquids, hot objects, hot gases, and smoke inhalation
- Radiation: Sun, Ultraviolet (UV) lamps, and lasers
- Electrical: Lightning and Home appliances
- Chemical: Caustic cleaners, solvents, laboratory reagents, and alkali agents
Severity of Burns
- Factors affecting severity: body location and skin thickness, temperature of the causative agent, type of causative agent, duration of exposure to causative agent, extent of the burn, and depth of the burn
- Patient factors affecting: Age (<5 or >60 yr = thinner skin = greater risk), medical conditions (e.g. diabetes or vascular disease), malnutrition, smoking, and drug therapy (e.g. immunosuppressants)
Pathophysiology of Burns
- Stasis/Ischemic Zone: Platelets aggregate + vessels constrict= marginally perfused tissue (extends around an injury)
- Hyperemia Zone: Tissue is inflamed, and perfusion is increased
Burn Severity
- Superficial burns only affect the epidermis; they are dry, pink or red, blanche markedly; can cause some edema but there are no blisters and the skin is intact
- Superficial Partial Thickness affect the epidermis + upper dermis, they are moist (weeping); and pink or red cause small blisters, they blanche with pressure, painful Heals in 1-3 weeks and typically, no scarring
- Deep Partial Thickness Affect the epidermis + dermis some hair follicle, sweat gland damage, they are dry or waxy variable color (red, patchy white), blisters may develop, no blanching, possible pain with pressure or only perceives pressure Heals in > 3 weeks and has a risk of scarring
- Full Thickness burns affects the epidermis + dermis + subcutaneous Layer, they are dry, waxy white to leathery grey to charred black may have bright red No blanching with pressure; Anesthetic to hypoesthetic or due to destruction of the nerves does NOT heal spontaneously High risk of scarring and other complications
Complications of Burns
- Local:
- Infection by: streptococci and staphylococci days 1-4 and gram(-) bacteria after 5 to 7 days; however, flora are almost always mixed which may lead to sepsis and mortality
- Scarring & Contractures due to: a major cause of long-term functional and cosmetic deformities which happen when: your muscles, tendons, joints, or other tissues tighten or shorten causing a deformity because Keloids may form in some patients, especially those with darker skin
- Eschar due to: Circumferential eschar, which completely encircles a limb (or sometimes the neck or torso), that is potentially constricting A constricting eschar limits tissue expansion in response to edema; instead, tissue pressure increases, eventually causing local ischemia (= could lose limb)
- Systemic: When >30 % of total body surface area affected the greater the risk of systemic complications, due to the release of cytokines and other inflammatory mediators at the site of injury
Referral for Burns
- TBSA: Burns that involve >10% total body surface area (TBSA) for adults, or >5% TBSA for children
- Severity: Any burn more serious than the mildest superficial partial thickness burn
- Thing Skin: Any burns involving thin skin areas (e.g., face, ears, eyelids, inner surface of arm, perineum)
- Age: Burns in individuals presumed to have thin skin (e.g., children less than 5 years of age or adults older than 60)
- Location: Burns involving the hands or feet or circumferential burns
- Concomitant trauma: events associated with a burn may cause other injuries (e.g. jumping out of burning building, MVC)
- Cause: Electrical, chemical or inhalation burns (e.g., electrical injury → cardiac dysrhythmias):, even if they appear to be minor, since the injury may be deeper than the initial appearance of the burn suggests and can progress to deep tissue necrosis within 24 hours
Management
- Superficial Burns/Minor Partial Thickness:
- Stop the process or cause of the burn
- Cool the burn with running water for 20 minutes
- Leave blisters intact
- Protect/Cover the wound to protect from friction & contamination
- Cleanse if secretions or debris are present, or if blisters break preferring soap & water or normal saline
- Provide pain & itch control using local anesthetics or antihistamines
- Partial & Full Thickness Burns:
- The patient is referred because the injury is assessed and treated by an HCP
- To prevent burn wound infections: Silver sulfadiazine (SSD), apply 1% cream in 1/16-inch layer 1-2x daily until healing or skin grafting
- Acts mainly on the cell membrane and cell wall which causes the bacteria to die and acts as a broad spectrum topical antibiotic
- Painless on application, but once opened should be discarded after 7 days and may actually DECREASE wound healing
- Avoid on face, sulfonamide allergies, infants < 2 months of age, women pregnant or breastfeeding
Pressure Injuries
- Pressure injuries are localized damage to the skin and/or underlying soft tissue as a result of intense and/or prolonged pressure ± shear such as bedsores, pressure ulcers, decubitus ulcers, decubiti, or pressure sores
Risk Factors
- Age: > 65-years-old as people over 65 are more likely to have reduced subcutaneous fat and capillary blood flow
- Mobility: Decreased mobility as they are more likely due to prolonged hospital stay, bed rest, spinal cord injury, sedation, weakness that decreases spontaneous movement, and/or cognitive impairment
- Skin condition: Exposure to moisture or to skin irritants such as due to urinary incontinence and/or fecal incontinence
- Comorbidities: Leading to impaired sensation and/or capacity for wound healing such as due to undernutrition; diabetes; impaired tissue perfusion due to peripheral arterial disease; venous insufficiency
Pathophysiology of Pressure Injury
- Pressure: when soft tissues are compressed for prolonged periods between bony prominences and external surfaces, microvascular occlusion with tissue ischemia and hypoxia occurs
- Friction: Can help trigger skin ulceration by causing local erosion and breaks in the epidermis and superficial dermis such as rubbing against clothing or bedding
- Shearing forces: Stress and damage supporting tissues by causing forces of muscles and subcutaneous tissues that are drawn down by gravity to oppose the more superficial tissues that remain in contact with external surfaces, such as when a patient is placed on an inclined surface
- Moisture: Leads to tissue breakdown and maceration which can initiate or worsen pressure injuries such as through perspiration and incontinence
Diagnosis Based on Location & Appearance
- Stage 1: Non-blanchable Erythema of Intact Skin:
- Erythema of localized area of skin that is intact
- Relieving the pressure does not immediately alleviate the erythema
- Usually over bony prominence or in painful areas Stage 2: Partial Thickness Skin Loss:
- Erosion looks like a shallow ulcer (or intact blister)
- Wound bed is bright pinkish-red
- No slough or necrotic tissue that is typically over specific pressure points such as the scrum, heels, elbows, or occiput
- Stage 3 & 4: Full Thickness Skin Loss:
- Stage 3: No bone, muscle, or tendon visible
- Stage 4: Extends to supporting tissue; bone, muscle or tendon -Diagnosis based on location and appearance: full thickness loss of skin (epidermis + dermis) extending into the subcutaneous tissue that has a crater-like shape or presents as possible slough and necrotic tissue, and eschar that is found in tunneling and undermining of adjacent tissues
Prevention of Pressure Injuries
- Pressure Relief: Determine the source of pressure and then relieve it
- Positioning/ Repositioning and Mobilize where possible by using Pressure-relieving devices, support surfaces and specialized beds
- Other Considerations: general health by ensuring Adequate nutrition & hydration along with proper Skin Care to Keep skin clean, dry & hydrated while protecting skin from moisture, by properly managing incontinence and to not rub or massage the affected area
Treatment for Pressure Injuries
- Preventative Measures of pressure relief, repositioning and mobilization
- Pain Management by monitoring regularly with a pain scale because the injury might be causing pain
- Primary pain management is treating the injury itself with NSAIDs or APAP while avoiding opioids
- Wound Care: Cleansing by generally cleansing with water or normal saline and antiseptic or antimicrobial when their is significant debris, confirmed or suspected infection, or high bacterial colonization
- Wound Care: Debridement by removing devitalized/dead tissue and inflammatory agents, and help convert a chronic wound to the molecular & cellular environment of an acute healing wound using Dressings
- Dressings: Protect the wound and maintain a moist environment to promote healing
- Infection Control by monitoring signs of bacterial infection by noting signs of elevated erythema, foul odor, warmth, drainage, fever, and elevated WBC count and impaired healing Use topical agents or systemic agents after consulting guide lines
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.