Podcast
Questions and Answers
What is the primary role of pulsatile GnRH secretion?
What is the primary role of pulsatile GnRH secretion?
- To regulate testosterone levels
- To control the secretion of FSH and LH (correct)
- To initiate oocyte maturation
- To directly stimulate sperm production
Which hormone inhibits FSH secretion?
Which hormone inhibits FSH secretion?
- Gonadotropin
- Testosterone
- Activin
- Inhibin (correct)
What is the role of Leydig cells in the male reproductive system?
What is the role of Leydig cells in the male reproductive system?
- They produce testosterone (correct)
- They store sperm
- They produce inhibin
- They conduct sperm
What triggers spermatogenesis?
What triggers spermatogenesis?
Which of the following is NOT a function of Sertoli cells?
Which of the following is NOT a function of Sertoli cells?
What is an effect of androgens on male development?
What is an effect of androgens on male development?
Which male accessory gland is responsible for secreting a fluid that nourishes sperm?
Which male accessory gland is responsible for secreting a fluid that nourishes sperm?
Which environmental factor does NOT influence reproductive physiology in women?
Which environmental factor does NOT influence reproductive physiology in women?
What substance must spermatids develop into to participate in fertilization?
What substance must spermatids develop into to participate in fertilization?
After puberty, how frequently does tonic GnRH release occur?
After puberty, how frequently does tonic GnRH release occur?
What is the primary reason male gametogenesis has a continuous production of sperm from puberty until death?
What is the primary reason male gametogenesis has a continuous production of sperm from puberty until death?
What occurs to primary oocytes before puberty in female gametogenesis?
What occurs to primary oocytes before puberty in female gametogenesis?
Which of the following describes the fate of the secondary oocyte after ovulation?
Which of the following describes the fate of the secondary oocyte after ovulation?
What is the main function of the hormone aromatase in the reproductive system?
What is the main function of the hormone aromatase in the reproductive system?
At birth, what is unique about female gametogenesis compared to male gametogenesis?
At birth, what is unique about female gametogenesis compared to male gametogenesis?
Which of the following best describes the feedback mechanisms of reproductive hormones in both sexes?
Which of the following best describes the feedback mechanisms of reproductive hormones in both sexes?
What role does inhibin play in the regulation of reproductive hormones?
What role does inhibin play in the regulation of reproductive hormones?
What happens during the first meiotic division in female gametogenesis?
What happens during the first meiotic division in female gametogenesis?
In male gametogenesis, what is the outcome of the first meiotic division?
In male gametogenesis, what is the outcome of the first meiotic division?
What is the primary hormonal trigger for both male and female gametogenesis?
What is the primary hormonal trigger for both male and female gametogenesis?
What is the primary role of anti-Müllerian hormone (AMH) during the early follicular phase?
What is the primary role of anti-Müllerian hormone (AMH) during the early follicular phase?
During which phase of the ovarian cycle does ovulation occur?
During which phase of the ovarian cycle does ovulation occur?
Which hormones are primarily secreted by the luteal cells of the corpus luteum?
Which hormones are primarily secreted by the luteal cells of the corpus luteum?
What occurs in the late luteal phase if pregnancy does not happen?
What occurs in the late luteal phase if pregnancy does not happen?
What is the significance of the surge in LH and FSH during the mid-late follicular phase?
What is the significance of the surge in LH and FSH during the mid-late follicular phase?
What is a primary characteristic of secondary follicles during follicular development?
What is a primary characteristic of secondary follicles during follicular development?
What initiates the proliferative phase of the uterine cycle?
What initiates the proliferative phase of the uterine cycle?
Which structure forms from the ruptured follicle after ovulation?
Which structure forms from the ruptured follicle after ovulation?
What causes the endometrium to thicken during the menstrual cycle?
What causes the endometrium to thicken during the menstrual cycle?
What happens to primary oocytes if they are not selected for maturation during follicular development?
What happens to primary oocytes if they are not selected for maturation during follicular development?
What is the function of the SRY gene in sex determination?
What is the function of the SRY gene in sex determination?
What is the significance of the presence of testosterone during male embryonic development?
What is the significance of the presence of testosterone during male embryonic development?
Which structure develops in the absence of both testosterone and Anti-Mullerian hormone (AMH)?
Which structure develops in the absence of both testosterone and Anti-Mullerian hormone (AMH)?
What happens to the Müllerian duct in male embryonic development?
What happens to the Müllerian duct in male embryonic development?
How many pairs of sex chromosomes are present in a typical diploid human cell?
How many pairs of sex chromosomes are present in a typical diploid human cell?
Which hormone is responsible for the regression of the gonadal medulla in female embryonic development?
Which hormone is responsible for the regression of the gonadal medulla in female embryonic development?
What type of cells produce testosterone in the developing male fetus?
What type of cells produce testosterone in the developing male fetus?
The diploid number of chromosomes in humans is represented as which of the following?
The diploid number of chromosomes in humans is represented as which of the following?
What role do gametes play in the context of human reproduction?
What role do gametes play in the context of human reproduction?
What is the outcome if the SRY gene is absent in an embryo?
What is the outcome if the SRY gene is absent in an embryo?
Flashcards
Spermatogenesis
Spermatogenesis
The process of sperm production in males, beginning at puberty and continuing throughout life.
Oogenesis
Oogenesis
The process of egg production in females, completed before birth and resuming at puberty.
Spermatogonia
Spermatogonia
Immature germ cells in males that divide mitotically to produce sperm.
Oogonia
Oogonia
Signup and view all the flashcards
Primary Oocyte
Primary Oocyte
Signup and view all the flashcards
Secondary Oocyte
Secondary Oocyte
Signup and view all the flashcards
Polar Body
Polar Body
Signup and view all the flashcards
Androgens
Androgens
Signup and view all the flashcards
Estrogens
Estrogens
Signup and view all the flashcards
Aromatase
Aromatase
Signup and view all the flashcards
GnRH
GnRH
Signup and view all the flashcards
FSH
FSH
Signup and view all the flashcards
LH
LH
Signup and view all the flashcards
Inhibin
Inhibin
Signup and view all the flashcards
Activin
Activin
Signup and view all the flashcards
Pulsatile GnRH Release
Pulsatile GnRH Release
Signup and view all the flashcards
Pulse Generator
Pulse Generator
Signup and view all the flashcards
Seminal Vesicles
Seminal Vesicles
Signup and view all the flashcards
Prostate Gland
Prostate Gland
Signup and view all the flashcards
Bulbourethral Gland (Cowper's Gland)
Bulbourethral Gland (Cowper's Gland)
Signup and view all the flashcards
Sex Chromosomes
Sex Chromosomes
Signup and view all the flashcards
Sperm's Role
Sperm's Role
Signup and view all the flashcards
Y Chromosome's Power
Y Chromosome's Power
Signup and view all the flashcards
Bipotential Gonads
Bipotential Gonads
Signup and view all the flashcards
What does SRY do?
What does SRY do?
Signup and view all the flashcards
Testosterone's Role
Testosterone's Role
Signup and view all the flashcards
AMH's Role
AMH's Role
Signup and view all the flashcards
Female Development
Female Development
Signup and view all the flashcards
Wolffian Duct
Wolffian Duct
Signup and view all the flashcards
Mullerian Duct
Mullerian Duct
Signup and view all the flashcards
Ovarian Cycle
Ovarian Cycle
Signup and view all the flashcards
Follicular Phase
Follicular Phase
Signup and view all the flashcards
Early Follicular Phase
Early Follicular Phase
Signup and view all the flashcards
Mid-to-Late Follicular Phase
Mid-to-Late Follicular Phase
Signup and view all the flashcards
Ovulation
Ovulation
Signup and view all the flashcards
Luteal Phase
Luteal Phase
Signup and view all the flashcards
Early-to-Mid Luteal Phase
Early-to-Mid Luteal Phase
Signup and view all the flashcards
Late Luteal Phase & Menstruation
Late Luteal Phase & Menstruation
Signup and view all the flashcards
Uterine Cycle
Uterine Cycle
Signup and view all the flashcards
Menstruation
Menstruation
Signup and view all the flashcards
Study Notes
Sex Determination
- Sperm determines sex by carrying either an X or Y chromosome
- One pair of sex chromosomes (XX or XY) determines gender
- The Y chromosome is essential for male development
Sex Chromosome Development
- Autosomal cells are somatic cells, having 22 pairs of non-sex chromosomes
- Gametes (egg and sperm cells) are haploid, meaning they contain 23 chromosomes.
- Diploid cells have two sets of chromosomes, one from each parent, resulting in a total of 46 chromosomes.
- Autosomal cells exclude sex cells/gametes
Bipotential Reproductive Structures
- Early embryos have bipotential reproductive structures that have the potential to become male or female structures.
- Chemicals/hormones determine the structure's development to either male or female structures
- The gene SRY, found on the Y chromosome, is crucial
- Leads to the production of the testes-determining factor when the SRY gene is present.
- Results in testes formation otherwise, female structures develop
Sexual Differentiation
- Male Development (Testosterone & AMH Present):
- Gonadal cortex regresses (shrinks and disappears)
- Gonadal medulla develops into testes
- Wolffian duct forms epididymis, vas deferens, and seminal vesicle; testosterone converts the Wolffian duct into male accessory structures
- Leydig / interstitial cells secrete testosterone
- Female Development (Testosterone & AMH Absent):
- Gonadal cortex develops into ovaries
- Gonadal medulla regresses
- Wolffian duct regresses
- Mullerian duct develops into fallopian tubes, uterus, cervix, and upper half of the vagina.
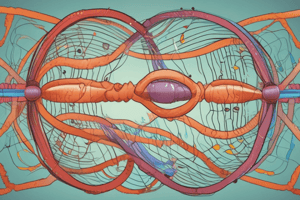
Gametogenesis
-
Male Gametogenesis:
- Begins in the fetus but doesn't proceed past mitosis until puberty.
- Germ cells are spermatogonia and do not divide until puberty.
- Mitosis resumes during puberty
- Continuous sperm production begins during puberty and continues until death.
-
Female Gametogenesis:
- Oogonia complete mitotic stages before birth
- Female meiosis begins before birth, and oocytes remain arrested in the primary oocyte phase until puberty.
- Beginning meiosis 1 steps before birth.
- Oocytes complete meiosis, eventually become eggs in the mature stage only if fertilized, one egg is produced per cycle.
- Oocyte maturation only occurs when selected and triggered every month during puberty and continues until menopause.
Basic Patterns of Reproduction
- Both sexes produce androgens and estrogens.
- Androgens are dominant in males
- Testosterone is produced in the testes.
- Estrogens are dominant in females
- Estrogens, Progestins, and androgens are produced in the ovaries
- Aromatase converts androgens to estrogens.
- Positive and negative feedback pathways control reproductive function. GnRH, FSH and LH (pituitary gonadotropins) are released by different areas in the brain to control gamete production.
Hormonal Control of Spermatogenesis
- Feedback pathways govern spermatogenesis, with testosterone playing a crucial role.
Primary and Secondary Sex Characteristics
- Androgens influence primary and secondary sex characteristics in males.
- Primary characteristics refer to reproductive ducts and organs.
- Secondary characteristics include traits like pubic/axillary hair and muscular development.
Female Reproduction
- Organization of ovary tissues, development of follicles from primordial to mature to release egg to fertilization, and development of the corpus luteum for the next cycle.
- The menstrual cycle has ovarian and uterine cycles that occur simultaneously but in different locations.
- Follicle development begins with the primordial follicle and progresses to the formation of a mature follicle that releases an egg during ovulation.
Menstrual Cycle
- Ovarian and uterine cycles are synchronized, with alternating phases of follicular and luteal development in the ovaries, and accompanying proliferative and secretory phases in the uterus.
Contraceptives
- Various methods exist, including abstinence, sterilization, barrier methods, hormonal treatments, and intrauterine devices (IUDs).
- Abstinence and sterilization are very effective, followed by barrier methods, intrauterine devices and lastly hormonal treatments ineffectiveness varies greatly.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.