Podcast
Questions and Answers
What effect does hydrostatic pressure during mastication have on bacteria in dentinal tubules?
What effect does hydrostatic pressure during mastication have on bacteria in dentinal tubules?
- It prevents bacteria from entering the tubules.
- It allows bacteria to enter the tubules without obstruction.
- It pushes bacteria into the tubules. (correct)
- It causes bacteria to die due to pressure.
What condition can lead to a rapid bacterial invasion of dentinal tubules?
What condition can lead to a rapid bacterial invasion of dentinal tubules?
- Healthy periodontal tissue.
- A soft dentinal smear layer.
- Non-vital pulp. (correct)
- Thick enamel layer.
What factors can breach the integrity of the enamel and cementum, thereby exposing the pulpodentin complex to infection?
What factors can breach the integrity of the enamel and cementum, thereby exposing the pulpodentin complex to infection?
- Fluoride treatments
- Scaling and root planning procedures (correct)
- Natural wear and tear from chewing (correct)
- Orthodontic adjustments
Which statement about the dentinal tubules and bacterial invasion is accurate?
Which statement about the dentinal tubules and bacterial invasion is accurate?
What is a consequence of exposing the dentin during restorative procedures?
What is a consequence of exposing the dentin during restorative procedures?
⭐️What is the average diameter of dentinal tubules near the pulp?
⭐️What is the average diameter of dentinal tubules near the pulp?
What is the MEAN diameter of dentinal tubules at their SMALLEST point?
What is the MEAN diameter of dentinal tubules at their SMALLEST point?
⭐️How do the dimensions of bacterial species interact with dentinal tubules?
⭐️How do the dimensions of bacterial species interact with dentinal tubules?
What tubular shape do dentinal tubules present?
What tubular shape do dentinal tubules present?
Flashcards are hidden until you start studying
Study Notes
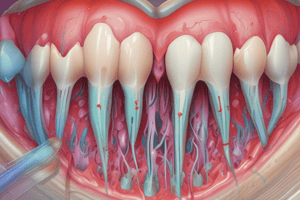
Routes of Infection
- The pulpodentin complex is normally sterile and isolated from oral microbiota by enamel and cementum.
- Breach, absence, or damage to these layers exposes the pulp to oral environment.
- Bacteria from caries, saliva, plaque, subgingival biofilms, or periodontal disease can enter the pulp through dentinal tubules.
- Dentinal tubules provide a pathway for bacteria to reach the pulp.
- The tubule diameter is compatible with most bacteria.
- Bacteria invading dentinal tubules is faster in nonvital pulps than vital pulps.
- A vital pulp can defend against bacteria through dentinal fluid and tubular contents, such as odontoblast processes, collagen fibrils, and lamina limitans.
- Other factors that limit bacterial invasion of dentinal tubules include dentinal sclerosis, tertiary dentin, smear layer, and intratubular fibrinogen deposition.
- Host defense molecules, like antibodies and components of the complement system, also protect against deep bacterial invasion of dentin.
- Direct exposure of the pulp to oral bacteria is the most obvious route for infection.
- Caries is the most common cause, but trauma and restorative procedures can also expose the pulp.
- Exposed pulps are susceptible to inflammation, necrosis, and infection.
- The time from exposure to infection varies, but it is usually a slow process.
- Bacteria and their products can exit the infected root canals through apical, lateral, or furcation foramina, dentinal tubules, and iatrogenic root perforations.
- Periodontal disease bacteria can reach the pulp through the same pathways as intracanal bacteria and affect the pulp.
- Periodontal biofilm reaching the apical foramen can cause pulpal necrosis.
- Once necrotic, the pulp can be invaded by periodontal bacteria through apical foramina, lateral canals, and dentinal tubules.
- Anachoresis, the transport of bacteria via bloodstream to damaged tissue, is not a confirmed route for root canal infection.
- Bacteria may be present in traumatized teeth with necrotic pulps, but the infection is more likely to arise from dentinal exposure due to enamel cracks.
- Cracks in enamel can provide portals of entry for bacteria into the pulp.
- The pulp is vulnerable to infection once it is necrotic.
- The root canal system is also vulnerable to infection after pulp removal during treatment.
- Microbial introduction during treatment can occur due to:
- Residual plaque biofilm, calculus, or caries on the tooth crown.
- Leaking rubber dam.
- Contaminated endodontic instruments.
- Contaminated irrigant solutions.
- Microbial introduction between appointments can occur due to:
- Leakage through temporary restorations.
- Breakdown, fracture, or loss of temporary restorations.
- Fracture of the tooth structure.
- Teeth left open for drainage.
- Microbial introduction after obturation can occur due to:
- Leakage through permanent restorations.
- Breakdown, fracture, or loss of permanent restorations.
- Fracture of the tooth structure.
- Recurrent decay.
- Delay in permanent restoration placement.
Dentinal Tubules
- Dentinal tubules are cylindrical canals that extend through the dentin, connecting the pulp chamber to the outer enamel or cementum.
- The diameter of these tubules gradually decreases from the pulp side (mean 2.5 mm) towards the enamel or cementum (mean 0.9 mm).
- The smallest diameter of the tubules is compatible with the size of most oral bacterial species, whose diameter typically ranges from 0.2 to 0.7 mm.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.