Podcast
Questions and Answers
A) Coeliac disease can result from a variety of genetic factors, one of which is HLA-DQ2 and HLA-DQ8 genes. Explain the role of these genes in the pathogenesis of coeliac disease, focusing on their association with gluten intolerance. (5 marks)
A) Coeliac disease can result from a variety of genetic factors, one of which is HLA-DQ2 and HLA-DQ8 genes. Explain the role of these genes in the pathogenesis of coeliac disease, focusing on their association with gluten intolerance. (5 marks)
These genes encode proteins known as human leukocyte antigens (HLAs), which are responsible for presenting antigens to immune cells. In the context of coeliac disease, individuals who possess specific variants of the HLA-DQ2 (encoded by the HLA-DQA1 and HLA-DQB1 genes) and HLA-DQ8 (encoded by the HLA-DQA1 and HLA-DQB1 genes) genes are at an increased risk of developing the condition. These HLA molecules play a crucial role in initiating the immune response to gluten, the protein complex found in wheat, barley, and rye. Specifically, HLA-DQ2 and HLA-DQ8 molecules bind to gluten peptides that have been modified by tissue transglutaminase (tTG) within the gut lumen. This binding facilitates the presentation of gluten peptides to T lymphocytes, triggering an immune response characterized by inflammation and tissue damage within the small intestine.
Discuss the histological changes observed in the small intestine of individuals with coeliac disease and their significance in diagnosis. (5 marks)
Discuss the histological changes observed in the small intestine of individuals with coeliac disease and their significance in diagnosis. (5 marks)
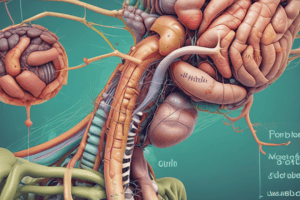
These histological changes range from mild intraepithelial lymphocytosis ( an increase in the number of lymphocytes within the epithelial layer of the small intestine) to severe villous atrophy, reflecting the extent of damage to the intestinal mucosa caused by the autoimmune response to gluten. In coeliac disease, prolonged exposure to gluten triggers an immune-mediated attack on the intestinal mucosa, leading to damage and flattening of the villi. This results in a loss of surface area for nutrient absorption and can manifest as malabsorption-related symptoms such as diarrhea, weight loss, and nutrient deficiencies.
ompare the treatment options for coeliac disease, focusing on the effectiveness of a gluten-free diet and the management of associated nutrient deficiencies. (15 marks; 5 points for each stage)
Guide: Your answer should discuss the primary treatment approach for coeliac disease, including the role of a gluten-free diet in achieving histological recovery and normalizing nutrient levels. Additionally, address the potential persistence of nutrient deficiencies despite dietary changes and the recommended strategies for managing these deficiencies at different stages of life.
ompare the treatment options for coeliac disease, focusing on the effectiveness of a gluten-free diet and the management of associated nutrient deficiencies. (15 marks; 5 points for each stage)
Guide: Your answer should discuss the primary treatment approach for coeliac disease, including the role of a gluten-free diet in achieving histological recovery and normalizing nutrient levels. Additionally, address the potential persistence of nutrient deficiencies despite dietary changes and the recommended strategies for managing these deficiencies at different stages of life.
Treatment options for coeliac disease primarily revolve around the adoption of a strict gluten-free diet. However, effectively managing associated nutrient deficiencies is also crucial for optimizing the health and well-being of individuals with coeliac disease. adherence to a gluten-free diet is essential for promoting healing of the intestinal mucosa, can lead to histological recovery and resolution of symptoms and prevent further damage. nutrient supplementation in nutrients such as iron, calcium, vitamin D and B12 may be needed to resolve nutrient deficiencies. Regular monitoring of nutritional status and growth parameters is important for identifying and addressing any ongoing nutrient deficiencies or growth delays and for preventing long-term health complications such as osteoporosis and anemia. dults with coeliac disease are at increased risk of osteoporosis due to malabsorption of calcium and vitamin D. Therefore, emphasis should be placed on optimizing bone health through adequate calcium and vitamin D intake, regular weight-bearing exercise, and bone density monitoring.
What are the potential causes of diet-refractory coeliac disease, and how are they managed? (10 marks)
Your answer should discuss the common causes of diet-refractory coeliac disease, such as non-malignant inflammation of the small intestine, enteropathy-associated T-cell lymphoma, collagenous sprue, and alternative diagnoses. For each cause, provide insights into the clinical presentation, diagnostic considerations, and management strategies.
What are the potential causes of diet-refractory coeliac disease, and how are they managed? (10 marks) Your answer should discuss the common causes of diet-refractory coeliac disease, such as non-malignant inflammation of the small intestine, enteropathy-associated T-cell lymphoma, collagenous sprue, and alternative diagnoses. For each cause, provide insights into the clinical presentation, diagnostic considerations, and management strategies.
Study Notes
Coeliac Disease and Genetics
- Coeliac disease is associated with genetic factors, including HLA-DQ2 and HLA-DQ8 genes.
- These genes play a role in the pathogenesis of coeliac disease, specifically in the development of gluten intolerance.
Histological Changes in Coeliac Disease
- Histological changes observed in the small intestine of individuals with coeliac disease include:
- Villous atrophy (flattening of villi)
- Crypt hyperplasia (increased crypt cell growth)
- Increased intraepithelial lymphocyte count
- These changes are significant in diagnosing coeliac disease.
Treatment Options for Coeliac Disease
- Primary treatment approach: gluten-free diet
- Goals of a gluten-free diet:
- Achieve histological recovery
- Normalize nutrient levels
- Potential persistence of nutrient deficiencies despite dietary changes
- Recommended strategies for managing nutrient deficiencies:
- Supplemental vitamins and minerals
- Regular monitoring of nutrient levels
Diet-Refractory Coeliac Disease
- Causes of diet-refractory coeliac disease:
- Non-malignant inflammation of the small intestine
- Enteropathy-associated T-cell lymphoma
- Collagenous sprue
- Alternative diagnoses
- For each cause:
- Clinical presentation
- Diagnostic considerations
- Management strategies
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Learn about the genetic factors contributing to coeliac disease, specifically the role of HLA-DQ2 and HLA-DQ8 genes in gluten intolerance. Understand how these genes affect the body's response to gluten. Test your knowledge of coeliac disease pathogenesis.