Podcast
Questions and Answers
What are the three components of the small intestine?
What are the three components of the small intestine?
- Cecum, Rectum, and Anal canal
- Duodenum, Jejunum, and Ileum (correct)
- Ileum, Jejunum, and Cecum
- Duodenum, Jejunum, and Rectum
What is the dietary source of coeliac disease?
What is the dietary source of coeliac disease?
- Sorbitol malabsorption
- Lactose intolerance
- Gluten sensitivity - wheat, barley, rye, and oats (correct)
- Fructose malabsorption
What is the genetic source of coeliac disease?
What is the genetic source of coeliac disease?
- The HLA C7 tissue type
- The HLA A1 tissue type
- The HLA B8 tissue type (correct)
- The HLA D4 tissue type
What is a common gastrointestinal symptom of coeliac disease?
What is a common gastrointestinal symptom of coeliac disease?
What is one of the extra-intestinal symptoms of coeliac disease?
What is one of the extra-intestinal symptoms of coeliac disease?
How is coeliac disease diagnosed?
How is coeliac disease diagnosed?
What is the primary treatment for coeliac disease?
What is the primary treatment for coeliac disease?
What is the increased risk of cancer in patients with coeliac disease?
What is the increased risk of cancer in patients with coeliac disease?
What is the consequence of vitamin K deficiency in coeliac disease?
What is the consequence of vitamin K deficiency in coeliac disease?
Which inflammatory bowel disease is more common?
Which inflammatory bowel disease is more common?
What is the immune aetiology of inflammatory bowel diseases?
What is the immune aetiology of inflammatory bowel diseases?
What is the protective effect of appendicectomy in inflammatory bowel diseases?
What is the protective effect of appendicectomy in inflammatory bowel diseases?
What is the characteristic of Crohn's disease in terms of affected areas?
What is the characteristic of Crohn's disease in terms of affected areas?
What is the characteristic of the wall of the bowel in Crohn's disease?
What is the characteristic of the wall of the bowel in Crohn's disease?
What is the microscopic feature of Crohn's disease?
What is the microscopic feature of Crohn's disease?
What are the two ways to improve the quality of life of a Crohn's patient?
What are the two ways to improve the quality of life of a Crohn's patient?
What is the potential effect of long-term systemic corticosteroid therapy on dental treatment?
What is the potential effect of long-term systemic corticosteroid therapy on dental treatment?
Which of the following is a specific dental complication that can occur as a result of Crohn's?
Which of the following is a specific dental complication that can occur as a result of Crohn's?
What is the diet used to combat orofacial granulomatosis?
What is the diet used to combat orofacial granulomatosis?
What is the definition of ulcerative colitis?
What is the definition of ulcerative colitis?
What is the most common family history that predisposes ulcerative colitis?
What is the most common family history that predisposes ulcerative colitis?
What is the potential complication of ulcerative colitis?
What is the potential complication of ulcerative colitis?
What is the manifestation of ulcerative colitis that is more prevalent in Crohn's?
What is the manifestation of ulcerative colitis that is more prevalent in Crohn's?
What is the joint manifestation of inflammatory bowel disease that is more prevalent in Crohn's?
What is the joint manifestation of inflammatory bowel disease that is more prevalent in Crohn's?
In which inflammatory bowel disease do kidney stones occur?
In which inflammatory bowel disease do kidney stones occur?
What is the bacteria that grows as a result of ulcerative colitis, and what does it cause?
What is the bacteria that grows as a result of ulcerative colitis, and what does it cause?
What is the most common presentation of colon cancer on the right colon?
What is the most common presentation of colon cancer on the right colon?
What is the dental relevance of carcinoma in the colon?
What is the dental relevance of carcinoma in the colon?
What is the characteristic feature of Osetomas?
What is the characteristic feature of Osetomas?
What can IBS mask?
What can IBS mask?
What is the treatment for Diverticular disease?
What is the treatment for Diverticular disease?
What is a common symptom of IBS-C?
What is a common symptom of IBS-C?
What is a common oral manifestation of ulcerative colitis?
What is a common oral manifestation of ulcerative colitis?
What is the purpose of pANCA serological tests in diagnosing IBDs?
What is the purpose of pANCA serological tests in diagnosing IBDs?
What is the recommended frequency for colonoscopy screening in patients with ulcerative colitis?
What is the recommended frequency for colonoscopy screening in patients with ulcerative colitis?
What is the name of the valve located in the colon?
What is the name of the valve located in the colon?
What is the prognosis for ulcerative colitis?
What is the prognosis for ulcerative colitis?
What is the purpose of cyclosporin in treating Crohn's disease?
What is the purpose of cyclosporin in treating Crohn's disease?
What is the name of the acronym used to remove infection in IBDs?
What is the name of the acronym used to remove infection in IBDs?
What is the increased risk of colon cancer associated with?
What is the increased risk of colon cancer associated with?
What is the purpose of aminosalicylates in treating ulcerative colitis?
What is the purpose of aminosalicylates in treating ulcerative colitis?
What is the common dental complication associated with cyclosporin use in Crohn's disease?
What is the common dental complication associated with cyclosporin use in Crohn's disease?
What is the common gastrointestinal symptom of coeliac disease associated with malabsorption?
What is the common gastrointestinal symptom of coeliac disease associated with malabsorption?
What is the type of anaemia commonly associated with coeliac disease?
What is the type of anaemia commonly associated with coeliac disease?
Which antibody is used first in the diagnosis of coeliac disease?
Which antibody is used first in the diagnosis of coeliac disease?
What is the name of the canal that is one of the three components of the large intestine?
What is the name of the canal that is one of the three components of the large intestine?
What is the name of the part of the small intestine that is affected in coeliac disease?
What is the name of the part of the small intestine that is affected in coeliac disease?
What is the name of the procedure used to diagnose coeliac disease?
What is the name of the procedure used to diagnose coeliac disease?
What is the percentage of people with coeliac disease that can be cured with gluten restriction?
What is the percentage of people with coeliac disease that can be cured with gluten restriction?
What is the increased risk of cancer associated with coeliac disease?
What is the increased risk of cancer associated with coeliac disease?
What is the dental complication associated with coeliac disease in childhood?
What is the dental complication associated with coeliac disease in childhood?
What is the age at which Crohn's disease is more common?
What is the age at which Crohn's disease is more common?
What is the protective effect of appendicectomy in inflammatory bowel diseases?
What is the protective effect of appendicectomy in inflammatory bowel diseases?
What is the characteristic feature of the wall of the bowel in Crohn's disease?
What is the characteristic feature of the wall of the bowel in Crohn's disease?
What is the microscopic feature of Crohn's disease?
What is the microscopic feature of Crohn's disease?
What is the method of diagnosis for Crohn's disease?
What is the method of diagnosis for Crohn's disease?
What is the treatment used to improve the quality of life of a Crohn's patient?
What is the treatment used to improve the quality of life of a Crohn's patient?
What is the consequence of vitamin B12 deficiency in coeliac disease?
What is the consequence of vitamin B12 deficiency in coeliac disease?
What effect may long-term systemic corticosteroid therapy have on dental treatment?
What effect may long-term systemic corticosteroid therapy have on dental treatment?
Which of the following is a specific dental complication that can occur as a result of Crohn's?
Which of the following is a specific dental complication that can occur as a result of Crohn's?
What is the oral manifestation of ulcerative colitis that appears as benign, multiple small white and yellow pustules?
What is the oral manifestation of ulcerative colitis that appears as benign, multiple small white and yellow pustules?
What is the diet used to combat orofacial granulomatosis?
What is the diet used to combat orofacial granulomatosis?
What is the purpose of sigmoidoscopy in diagnosing IBDs?
What is the purpose of sigmoidoscopy in diagnosing IBDs?
What is the definition of ulcerative colitis?
What is the definition of ulcerative colitis?
What is the blood investigation used to diagnose the type of anaemia in IBD patients?
What is the blood investigation used to diagnose the type of anaemia in IBD patients?
What is the potential aetiology of ulcerative colitis?
What is the potential aetiology of ulcerative colitis?
What is the purpose of azathioprine in treating IBDs?
What is the purpose of azathioprine in treating IBDs?
What is the complication/risk associated with ulcerative colitis?
What is the complication/risk associated with ulcerative colitis?
What is the cutaneous manifestation of ulcerative colitis that appears as a haemorrhagic lesion?
What is the cutaneous manifestation of ulcerative colitis that appears as a haemorrhagic lesion?
What is the eye manifestation that is more prevalent in Crohn's?
What is the eye manifestation that is more prevalent in Crohn's?
What is the joint manifestation that is more prevalent in Crohn's?
What is the joint manifestation that is more prevalent in Crohn's?
What is the dental complication associated with cyclosporin use in Crohn's disease?
What is the dental complication associated with cyclosporin use in Crohn's disease?
What is the name of the valve located in the colon?
What is the name of the valve located in the colon?
What is the liver/billary manifestation that is more prevalent in ulcerative colitis?
What is the liver/billary manifestation that is more prevalent in ulcerative colitis?
What is the bacteria that grows as a result of ulcerative colitis?
What is the bacteria that grows as a result of ulcerative colitis?
What is the purpose of pANCA serological tests in diagnosing IBDs?
What is the purpose of pANCA serological tests in diagnosing IBDs?
What is the increased risk of cancer associated with?
What is the increased risk of cancer associated with?
What is the treatment for inducing remission in Crohn's disease?
What is the treatment for inducing remission in Crohn's disease?
What is the characteristic feature of pain in Osetomas?
What is the characteristic feature of pain in Osetomas?
What is the common feature of colon cancer presentation on both colons?
What is the common feature of colon cancer presentation on both colons?
What is the consequence of anaemia on dental health?
What is the consequence of anaemia on dental health?
What is the primary treatment for Diverticular disease?
What is the primary treatment for Diverticular disease?
What is the characteristic feature of IBS-C?
What is the characteristic feature of IBS-C?
What is the relevance of Virchow's node to colon cancer?
What is the relevance of Virchow's node to colon cancer?
Study Notes
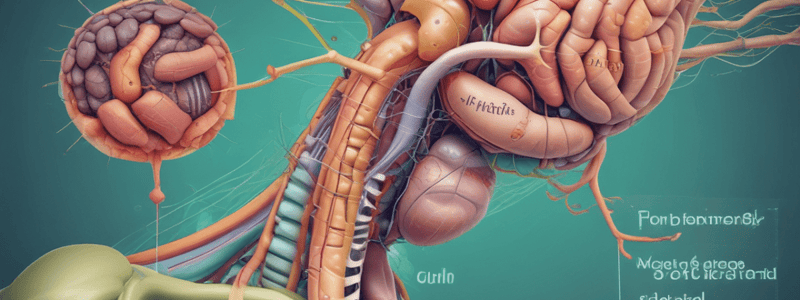
Gastrointestinal System Components
- The small intestine consists of three components: Duodenum, Jejunum, and Ileum
- The large intestine consists of three components: Cecum, Rectum, and Anal canal
Coeliac Disease
- Causes:
- Dietary source: Gluten sensitivity (wheat, barley, rye, and oats)
- Genetic source: HLA B8 tissue type
- Symptoms:
- Change of bowel habit (COBH)
- Gastrointestinal symptoms:
- Diarrhea
- Flatulence
- Borborygmi
- Weight loss
- Weakness, fatigue
- Abdominal pain
- Secondary lactose intolerance
- Steatorrhoea
- Extra-intestinal symptoms:
- Anaemias (10-15%), especially Fe and B12 deficiency
- Neurological symptoms (8-14%)
- Skin disorders (10-20%)
- Endocrine disturbances (infertility, impotence, amenorrhoea, delayed menarche)
- Diagnosis:
- Using antibodies to gliadin, endomysium, and transglutaminase (ttg)
- Endoscopic biopsy
- Pillcam camera for non-invasive inspection
- Treatment:
- Gluten restriction (cures 95%)
- Corticosteroids for the remaining 5%
Complications of Coeliac Disease
- Increased risk of lymphoma and adenocarcinoma of the:
- Pancreas
- Oesophagus
- Small bowel
- Biliary tract
- T and B cell non-Hodgkin lymphoma
- Malabsorption problems:
- B12, folate, ferritin deficiency leading to:
- Glossitis
- Angular cheilitis
- Anaemia
- Burning mouth
- Smooth tongue
- Vitamin K deficiency leading to bleeding tendency
- Vitamin D deficiency leading to osteomalacia and rickets in children
- B12, folate, ferritin deficiency leading to:
- Dental problems:
- Enamel defects in permanent dentition, like hypoplasia, if onset is in childhood
Inflammatory Bowel Diseases
- Two main types: Crohn's disease and Ulcerative colitis
- More common: Ulcerative colitis
- Age of onset: Crohn's (26 years), Ulcerative colitis (34 years)
- Gender ratio: Females: 1.2:1, Males: 1.2:1
- Aetiology: Defective immune system, leading to autoimmunity
- Hygiene: Crohn's occurs in good hygiene and developed countries, while Ulcerative colitis has no relation to hygiene
- Protective factor: Appendicectomy is protective of Ulcerative colitis
- Maternal act: Breastfeeding reduces the risk of developing IBD
Crohn's Disease
- Definition: Lifelong condition where parts of the digestive system become inflamed
- Areas affected:
- Any part of the digestive tract from mouth to anus
- Phenotypes:
- Stricturing: gradual thickening of intestinal wall, leading to stenosis/obstruction
- Penetrating: intestinal fistulas between GI tract and other organs
- Non-penetrating: anal fissures, abscesses
- Macroscopic changes:
- Thickened bowel
- Narrowed lumen
- Deep ulcers
- Mucosal fissures
- Cobblestone appearance
- Fistulae
- Abscesses
- Apthoid ulceration
- Microscopic changes:
- Chronic inflammatory cells occurring transmurally
- Lymphoid hyperplasia
- Granulomas in Langhans cells
- Diagnosis:
- Barium enema, showing rose thorn, skip lesion, or string sign
- Sigmoidoscopy, biopsy, colonoscopy
- Differential diagnosis includes TB and sarcoidosis
- Treatment:
- Medical: glucocorticoids, immunomodulators, biologics
- Surgical: intestinal resection
- Complications:
- Dental: Many dental patients are receiving long-term systemic corticosteroid therapy, which may have a profound effect on risk of infection, wound healing, and ability to handle stress
- Specific dental lesions:
- Diffuse labial and buccal swelling
- Cobblestones
- Mucosal tags
- Linear ulcers
- Mucogingivitis
- Granulomatous Cheilitis
- Gingival enlargement
- Oral ulceration
- Staghorn calculus in submandibular ducts
- Non-specific dental lesions:
- Aphthous ulcers
- Angular cheilitis
- Glossitis
- Dental caries
- Gingivitis/Periodontitis
Ulcerative Colitis
- Definition: Diffuse mucosal inflammation of the colon with backwash involvement of the terminal ileum
- Areas affected:
- Rectum is always involved
- Conditions:
- Proctitis
- Left-sided colitis
- Pancolitis
- Backwash ileitis
- Microscopic changes:
- Chronic inflammatory cells occurring on the lamina propria
- Goblet cell depletion
- Crypt abscess
- Aetiology:
- Dysregulated interaction mucosal immunology
- Intestinal microflora
- Genetic predisposition (Jewish)
- Symptoms:
- Painless
- Bloody diarrhoea with mucus
- Associated fevers and remissions to near normal
- Surviving mucosa
- Crypt distortion
- Loss of haustra
- Absence of goblet cells
- Diagnosis:
- Colonoscopy and biopsy
- Exudates, ulcerations, loss of vascular pattern, friability, continuous granularity, superficial inflammation with loss of haustration
- Treatment:
- High protein and high fibre diet
- 5-ASA (5-amino salicyclic acid)
- Sulphasalazine and mesalazine
- Thiopurines
- Corticosteroids
- Surgery
- Complications:
- Colorectal cancer
Gastrointestinal System Components
- The small intestine consists of three components: Duodenum, Jejunum, and Ileum
- The large intestine consists of three components: Cecum, Rectum, and Anal canal
Coeliac Disease
- Causes:
- Dietary source: Gluten sensitivity (wheat, barley, rye, and oats)
- Genetic source: HLA B8 tissue type
- Symptoms:
- Change of bowel habit (COBH)
- Gastrointestinal symptoms:
- Diarrhea
- Flatulence
- Borborygmi
- Weight loss
- Weakness, fatigue
- Abdominal pain
- Secondary lactose intolerance
- Steatorrhoea
- Extra-intestinal symptoms:
- Anaemias (10-15%), especially Fe and B12 deficiency
- Neurological symptoms (8-14%)
- Skin disorders (10-20%)
- Endocrine disturbances (infertility, impotence, amenorrhoea, delayed menarche)
- Diagnosis:
- Using antibodies to gliadin, endomysium, and transglutaminase (ttg)
- Endoscopic biopsy
- Pillcam camera for non-invasive inspection
- Treatment:
- Gluten restriction (cures 95%)
- Corticosteroids for the remaining 5%
Complications of Coeliac Disease
- Increased risk of lymphoma and adenocarcinoma of the:
- Pancreas
- Oesophagus
- Small bowel
- Biliary tract
- T and B cell non-Hodgkin lymphoma
- Malabsorption problems:
- B12, folate, ferritin deficiency leading to:
- Glossitis
- Angular cheilitis
- Anaemia
- Burning mouth
- Smooth tongue
- Vitamin K deficiency leading to bleeding tendency
- Vitamin D deficiency leading to osteomalacia and rickets in children
- B12, folate, ferritin deficiency leading to:
- Dental problems:
- Enamel defects in permanent dentition, like hypoplasia, if onset is in childhood
Inflammatory Bowel Diseases
- Two main types: Crohn's disease and Ulcerative colitis
- More common: Ulcerative colitis
- Age of onset: Crohn's (26 years), Ulcerative colitis (34 years)
- Gender ratio: Females: 1.2:1, Males: 1.2:1
- Aetiology: Defective immune system, leading to autoimmunity
- Hygiene: Crohn's occurs in good hygiene and developed countries, while Ulcerative colitis has no relation to hygiene
- Protective factor: Appendicectomy is protective of Ulcerative colitis
- Maternal act: Breastfeeding reduces the risk of developing IBD
Crohn's Disease
- Definition: Lifelong condition where parts of the digestive system become inflamed
- Areas affected:
- Any part of the digestive tract from mouth to anus
- Phenotypes:
- Stricturing: gradual thickening of intestinal wall, leading to stenosis/obstruction
- Penetrating: intestinal fistulas between GI tract and other organs
- Non-penetrating: anal fissures, abscesses
- Macroscopic changes:
- Thickened bowel
- Narrowed lumen
- Deep ulcers
- Mucosal fissures
- Cobblestone appearance
- Fistulae
- Abscesses
- Apthoid ulceration
- Microscopic changes:
- Chronic inflammatory cells occurring transmurally
- Lymphoid hyperplasia
- Granulomas in Langhans cells
- Diagnosis:
- Barium enema, showing rose thorn, skip lesion, or string sign
- Sigmoidoscopy, biopsy, colonoscopy
- Differential diagnosis includes TB and sarcoidosis
- Treatment:
- Medical: glucocorticoids, immunomodulators, biologics
- Surgical: intestinal resection
- Complications:
- Dental: Many dental patients are receiving long-term systemic corticosteroid therapy, which may have a profound effect on risk of infection, wound healing, and ability to handle stress
- Specific dental lesions:
- Diffuse labial and buccal swelling
- Cobblestones
- Mucosal tags
- Linear ulcers
- Mucogingivitis
- Granulomatous Cheilitis
- Gingival enlargement
- Oral ulceration
- Staghorn calculus in submandibular ducts
- Non-specific dental lesions:
- Aphthous ulcers
- Angular cheilitis
- Glossitis
- Dental caries
- Gingivitis/Periodontitis
Ulcerative Colitis
- Definition: Diffuse mucosal inflammation of the colon with backwash involvement of the terminal ileum
- Areas affected:
- Rectum is always involved
- Conditions:
- Proctitis
- Left-sided colitis
- Pancolitis
- Backwash ileitis
- Microscopic changes:
- Chronic inflammatory cells occurring on the lamina propria
- Goblet cell depletion
- Crypt abscess
- Aetiology:
- Dysregulated interaction mucosal immunology
- Intestinal microflora
- Genetic predisposition (Jewish)
- Symptoms:
- Painless
- Bloody diarrhoea with mucus
- Associated fevers and remissions to near normal
- Surviving mucosa
- Crypt distortion
- Loss of haustra
- Absence of goblet cells
- Diagnosis:
- Colonoscopy and biopsy
- Exudates, ulcerations, loss of vascular pattern, friability, continuous granularity, superficial inflammation with loss of haustration
- Treatment:
- High protein and high fibre diet
- 5-ASA (5-amino salicyclic acid)
- Sulphasalazine and mesalazine
- Thiopurines
- Corticosteroids
- Surgery
- Complications:
- Colorectal cancer
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
This quiz covers the components of the small and large intestine, as well as the causes and symptoms of coeliac disease, including dietary sources and genetic predispositions.