Podcast
Questions and Answers
What is the primary consequence of chronic excessive dilation of the myocardium?
What is the primary consequence of chronic excessive dilation of the myocardium?
- Reduced contractility and stroke volume (correct)
- Increased stroke volume and cardiac output
- Hypertrophy of myocytes
- Increased thickness of the myocardial wall
What is the primary goal of treatment for LV systolic heart failure?
What is the primary goal of treatment for LV systolic heart failure?
- Reduce aldosterone levels
- Prolong diastole and increase venous return
- Reduce symptoms and hospitalization (correct)
- Improve cardiac output and stroke volume
Which of the following is a characteristic of LV diastolic heart failure?
Which of the following is a characteristic of LV diastolic heart failure?
- Impaired contractility
- Increased cardiac output
- Preserved ejection fraction (correct)
- Reduced ejection fraction
What is the effect of beta blockers on the heart?
What is the effect of beta blockers on the heart?
Which of the following is a treatment for LV diastolic heart failure?
Which of the following is a treatment for LV diastolic heart failure?
What type of ischemia is seen in unstable angina?
What type of ischemia is seen in unstable angina?
What is the main difference between stable and unstable angina?
What is the main difference between stable and unstable angina?
What is the diagnostic test for stable ischemic heart disease?
What is the diagnostic test for stable ischemic heart disease?
What is the treatment for acute coronary syndrome?
What is the treatment for acute coronary syndrome?
What is the pathological change in acute myocardial infarction?
What is the pathological change in acute myocardial infarction?
What is the most common early complication of acute myocardial infarction?
What is the most common early complication of acute myocardial infarction?
What is the formula for cardiac output?
What is the formula for cardiac output?
What is the determinant of stroke volume that depends on venous return to the heart?
What is the determinant of stroke volume that depends on venous return to the heart?
What is the result of increased preload on stroke volume?
What is the result of increased preload on stroke volume?
What is the type of infarction seen in main artery occlusion?
What is the type of infarction seen in main artery occlusion?
According to the Frank-Starling law, what is the effect of increased venous return on the heart?
According to the Frank-Starling law, what is the effect of increased venous return on the heart?
What is the primary factor that determines afterload?
What is the primary factor that determines afterload?
What is the characteristic feature of left ventricular systolic heart failure?
What is the characteristic feature of left ventricular systolic heart failure?
What is the effect of myocardial ischemia and infarction on the heart?
What is the effect of myocardial ischemia and infarction on the heart?
What is the primary cause of left ventricular diastolic heart failure?
What is the primary cause of left ventricular diastolic heart failure?
What is the clinical significance of reduced blood ejected forward in systolic heart failure?
What is the clinical significance of reduced blood ejected forward in systolic heart failure?
What is the primary mechanism of the sympathetic nervous system in response to heart failure?
What is the primary mechanism of the sympathetic nervous system in response to heart failure?
What is the effect of chronic activation of the renin-angiotensin-aldosterone system (RAAS) in heart failure?
What is the effect of chronic activation of the renin-angiotensin-aldosterone system (RAAS) in heart failure?
What is the primary mechanism of cardiac remodeling in heart failure?
What is the primary mechanism of cardiac remodeling in heart failure?
What is the characteristic feature of left ventricular diastolic heart failure?
What is the characteristic feature of left ventricular diastolic heart failure?
What is the primary mechanism by which smoking contributes to the development of atherosclerosis?
What is the primary mechanism by which smoking contributes to the development of atherosclerosis?
What is the result of glucose binding to blood lipids and proteins in diabetes?
What is the result of glucose binding to blood lipids and proteins in diabetes?
What is the mechanism by which hypertension contributes to the development of atherosclerosis?
What is the mechanism by which hypertension contributes to the development of atherosclerosis?
What is the primary consequence of excessive LDL deposition in the endothelium?
What is the primary consequence of excessive LDL deposition in the endothelium?
What characterizes a complicated atherosclerotic plaque?
What characterizes a complicated atherosclerotic plaque?
What is the consequence of oxidative LDL attracting macrophages in atherosclerosis?
What is the consequence of oxidative LDL attracting macrophages in atherosclerosis?
What is the result of the rupture of an atherosclerotic plaque?
What is the result of the rupture of an atherosclerotic plaque?
What type of atherosclerotic plaque is characterized by a thin capsule and inflammatory core?
What type of atherosclerotic plaque is characterized by a thin capsule and inflammatory core?
Flashcards are hidden until you start studying
Study Notes
Risk Factors of Atherosclerosis and Mechanism
- Smoking: produces reactive oxygen species, leading to oxidative stress, damage to endothelial cells, and increased permeability, resulting in accumulation of lipoprotein in the subendothelial space
- Diabetes: glucose binds to blood lipids and proteins, forming Advanced Glycation End products (AGEs), which interact with and damage endothelial cells, leading to accumulation of lipoproteins in the subendothelial space
- Hypertension (HTN): shear mechanical stress on endothelial cells, decreasing nitric oxide production, leading to vasoconstriction and increased endothelial permeability
- Dyslipidemia (elevated LDL): increased LDL in the blood, leading to accumulation of lipoprotein in the subendothelial space
Formation of Atherosclerotic Plaque
- Excessive LDL deposition in the endothelium, leading to oxidation and formation of a soft, lipid-loaded core
- Platelet activation, growth factor release, and formation of a hard, fibrotic cap
- Types of atherosclerotic plaques: uncomplicated (slowly growing, asymptomatic), complicated (rupture, symptomatic), and unstable (rupture before occlusion)
Ischemic Heart Disease Syndromes
- Stable Ischemic Heart Disease (uncomplicated, stable plaque): chest pain, pressure, or tightness with activity, relieved with rest
- Acute Coronary Syndrome (complicated, unstable plaque): acute onset of chest pain or pressure at rest, due to rupture of atherosclerotic plaque with thrombosis
- Unstable Angina (reversible ischemia): acute onset of chest pain or pressure at rest, due to rupture of atherosclerotic plaque with thrombosis
- Acute Myocardial Infarction (irreversible infarction): acute onset of chest pain or pressure at rest, due to rupture of atherosclerotic plaque with 100% thrombosis
Diagnosis and Treatment
- Diagnosis of Stable Ischemic Heart Disease: normal ECG during rest, ST depression during stress test, and negative cardiac enzymes
- Diagnosis of Acute Coronary Syndrome: resting ECG (ST depression), negative cardiac enzymes, and anticoagulant and revascularization treatment
- Diagnosis of Acute Myocardial Infarction: resting ECG (ST depression or elevation), elevated cardiac enzymes, and treatment with anticoagulant and revascularization
- Treatment for Coronary Artery Syndrome: anticoagulant, revascularization, and aspirin to reduce platelet aggregation
Pathological Changes in Acute Myocardial Infarction
- Myocardial oxygen deprivation, leading to anaerobic metabolism, accumulation of lactate, and calcium influx into cells, causing cellular death (necrosis)
- Necrosis starts within 30 minutes, completes within 6-12 hours, and is recognized by macrophages within 3-7 days, leading to fibrosis and diminished heart function
Complications of Acute Myocardial Infarction
- Early complications: arrhythmias, cardiogenic shock, and acute rupture of cardiac structures
- Late complications: pericarditis, heart failure, and ventricular remodeling
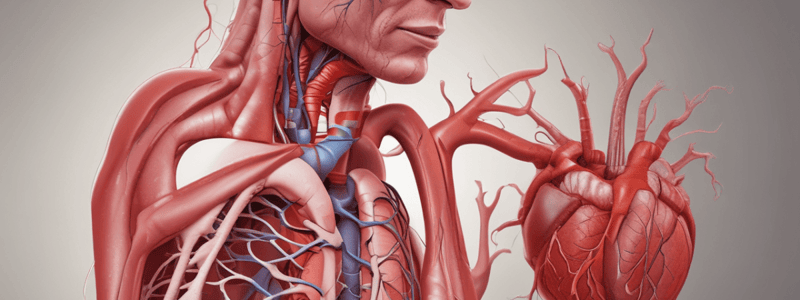
Cardiac Output and Failure
- Cardiac Output: stroke volume x heart rate
- Stroke volume: end diastolic volume - end systolic volume
- Ejection fraction: stroke volume divided by end diastolic volume
- Stroke volume determinants: contractility, preload, and afterload
- Left Ventricular Systolic Heart Failure (HF with reduced EF): weak ventricular contraction, decreased stroke volume, and decreased cardiac output
- Left Ventricular Diastolic Heart Failure (HF with preserved EF): impaired ability to relax and accommodate volume, reduced end diastolic volume, and reduced stroke volume
- Causes of LV systolic HF: MI/ischemia, HTN, valvular disease, and rare diseases (myocarditis)
- Causes of LV diastolic HF: long-standing HTN, myocardial ischemia and infarction, and valvular disease
Compensatory Mechanisms
- Sympathetic nervous system activation: increases myocardial contractility, heart rate, and cardiac output
- Renin-angiotensin-aldosterone system (RAAS) activation: increases sodium and water retention, leading to increased preload and cardiac output
- Cardiac remodeling: mechanical stress on myocardium, leading to increased LV size, accommodation of increased end diastolic volume, and increased cardiac output
Diagnosis and Treatment of Heart Failure
- Diagnosis of LV systolic HF: echo (reduced LV contractility, reduced EF), chest x-ray (cardiomegaly, pulmonary congestion/edema), and treatment with beta blockers and ACE/ARBs
- Diagnosis of LV diastolic HF: echo (preserved EF, hypertrophy of wall), chest x-ray (pulmonary congestion/edema), and treatment with diuretics and SGLT2 inhibitors
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.