Podcast
Questions and Answers
A patient reports seeing small, dark spots drifting across their vision. This symptom is most likely related to which of the following?
A patient reports seeing small, dark spots drifting across their vision. This symptom is most likely related to which of the following?
- Lattice degeneration
- Increased intraocular pressure
- Cataract formation
- The presence of floaters (correct)
Which type of retinal detachment is characterized by fluid accumulation beneath the retina without any tears or breaks?
Which type of retinal detachment is characterized by fluid accumulation beneath the retina without any tears or breaks?
- Tractional
- Rhegmatogenous
- Combined tractional-rhegmatogenous
- Exudative (correct)
A patient with proliferative diabetic retinopathy is at increased risk for which type of retinal detachment?
A patient with proliferative diabetic retinopathy is at increased risk for which type of retinal detachment?
- Age-related
- Exudative
- Tractional (correct)
- Rhegmatogenous
Why is maintaining a specific post-operative position, such as face-down, crucial after retinal detachment surgery?
Why is maintaining a specific post-operative position, such as face-down, crucial after retinal detachment surgery?
Which of the following statements best describes the mechanism of action of laser photocoagulation in treating retinal tears?
Which of the following statements best describes the mechanism of action of laser photocoagulation in treating retinal tears?
Which diagnostic test is most useful when the view of the retina is obscured by a vitreous hemorrhage?
Which diagnostic test is most useful when the view of the retina is obscured by a vitreous hemorrhage?
A patient who has undergone a vitrectomy is at increased risk for which of the following complications?
A patient who has undergone a vitrectomy is at increased risk for which of the following complications?
Which of the following is a key nursing intervention in the preoperative care of a patient scheduled for retinal detachment surgery?
Which of the following is a key nursing intervention in the preoperative care of a patient scheduled for retinal detachment surgery?
A patient post pneumatic retinopexy should be educated to immediately report which of the following symptoms?
A patient post pneumatic retinopexy should be educated to immediately report which of the following symptoms?
Which of the following is a significant risk factor for developing rhegmatogenous retinal detachment?
Which of the following is a significant risk factor for developing rhegmatogenous retinal detachment?
Flashcards
Retinal Detachment
Retinal Detachment
Separation of the retina from the underlying epithelium, disrupting vision and potentially causing blindness.
Rhegmatogenous Retinal Detachment
Rhegmatogenous Retinal Detachment
A tear or break in the retina allows fluid to seep between the retinal layers.
Tractional Retinal Detachment
Tractional Retinal Detachment
Pulling forces, usually from scar tissue, cause the retina to detach.
Exudative (Serous) Retinal Detachment
Exudative (Serous) Retinal Detachment
Signup and view all the flashcards
Photopsia
Photopsia
Signup and view all the flashcards
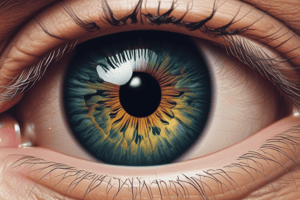
Floaters
Floaters
Signup and view all the flashcards
Pneumatic Retinopexy
Pneumatic Retinopexy
Signup and view all the flashcards
Scleral Buckling
Scleral Buckling
Signup and view all the flashcards
Vitrectomy
Vitrectomy
Signup and view all the flashcards
Proliferative Vitreoretinopathy (PVR)
Proliferative Vitreoretinopathy (PVR)
Signup and view all the flashcards
Study Notes
- Retinal detachment is a separation of the retina from the underlying epithelium
- It disrupts vision and can cause blindness
- Prompt intervention is needed
Types of Retinal Detachment
- Rhegmatogenous:
- Most common type
- A tear or break in the retina allows fluid from the vitreous cavity to seep between the retinal layers
- Fluid accumulation separates the retina from the retinal pigment epithelium (RPE)
- Tractional:
- Occurs when pulling forces, usually from scar tissue or membranes on the retina, cause it to detach
- Often seen in patients with proliferative diabetic retinopathy or other conditions causing retinal neovascularization and subsequent fibrosis
- Exudative (Serous):
- Results from fluid accumulation beneath the retina due to inflammation, vascular abnormalities, or other conditions
- No tears or breaks in the retina
- Fluid comes from the choroid
Risk Factors
- Myopia (nearsightedness): Increased axial length can predispose to retinal tears
- Prior cataract surgery: Can increase the risk of retinal breaks
- Family history: Genetic predisposition
- Age: More common in older adults
- Trauma: Injury to the eye
- Lattice degeneration: Thinning of the peripheral retina
- Diabetic retinopathy: Tractional detachments
Signs and Symptoms
- Flashes of light (photopsia): Often occur with vitreous traction on the retina
- Floaters: Small dark spots or streaks that drift across the field of vision, indicating blood or pigment released into the vitreous
- Blurred vision: Can occur as detachment progresses
- Shadow or curtain in the peripheral vision: Classic symptom as the retina detaches
- Decreased central vision: Occurs if the macula detaches, indicating a more severe detachment
Diagnostic Tests
- Dilated fundus examination: Essential for visualizing the retina
- Slit-lamp biomicroscopy: Provides a magnified view of the retina and vitreous
- Optical coherence tomography (OCT): Scans the retina to evaluate its structure
- Ultrasound: Performed if the view of the retina is obscured by hemorrhage
Treatment Options
- Laser photocoagulation or cryopexy:
- Used to create chorioretinal adhesion around retinal tears or breaks
- Prevent fluid from entering and causing detachment
- Pneumatic retinopexy:
- Involves injecting a gas bubble into the vitreous cavity
- The bubble flattens the retina against the RPE
- Laser or cryopexy is then used to seal the tear
- Scleral buckling:
- A silicone band is sewn onto the sclera to indent the eye wall and relieve traction on the retina
- May be combined with cryopexy or laser
- Vitrectomy:
- Surgical removal of the vitreous gel, which then replaces it with a gas or oil
- Used for complex detachments, tractional detachments, and cases with significant vitreous hemorrhage
- Often combined with membrane peeling or endolaser
Preoperative Nursing Interventions
- Educate the patient about the surgical procedure
- Explain the expected outcomes, and potential complications
- Obtain informed consent
- Administer prescribed eye drops (e.g., mydriatics, cycloplegics, antibiotics)
- Maintain the patient on NPO status as directed
- Emphasize the importance of following post-operative positioning instructions
Postoperative Nursing Interventions
- Monitor vital signs and assess pain levels
- Administer pain medication as prescribed
- Position the patient as prescribed:
- Crucial for promoting retinal reattachment, especially with gas or oil tamponade, often face-down
- Educate the patient about activity restrictions
- Avoid strenuous activities, heavy lifting, and sudden head movements
- Administer prescribed eye drops:
- Antibiotics, anti-inflammatories, and cycloplegics to prevent infection, reduce inflammation, and relieve pain
- Monitor for complications:
- Increased intraocular pressure (IOP), infection, bleeding, and recurrence of retinal detachment
- Educate the patient on signs and symptoms to report
- Increased pain, decreased vision, flashes of light, or new floaters
- Provide emotional support:
- Vision changes can be distressing
Patient Education
- Importance of adherence to prescribed eye drops and medications
- Proper eye hygiene to prevent infection
- Use of eye shields, especially at night, to protect the eye
- Recognizing and reporting potential complications
- Importance of follow-up appointments to monitor progress
- Visual rehabilitation strategies and devices as needed
Potential Complications
- Increased intraocular pressure (IOP): Can lead to glaucoma
- Infection (endophthalmitis): A severe sight-threatening complication
- Bleeding (vitreous hemorrhage): Can obscure vision
- Cataract formation: Can occur after vitrectomy
- Recurrent retinal detachment: Requires further treatment
- Proliferative vitreoretinopathy (PVR): Scar tissue formation on the retina leading to re-detachment
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.