Podcast
Questions and Answers
Which of the following is NOT a primary function of the respiratory system?
Which of the following is NOT a primary function of the respiratory system?
- Transporting oxygen to the body's cells.
- Removing carbon dioxide waste from the body.
- Facilitating ventilation for gas exchange.
- Regulating blood pH levels. (correct)
What is the role of mitochondria in relation to the respiratory system?
What is the role of mitochondria in relation to the respiratory system?
- Mitochondria produce and transport oxygen throughout the body.
- Mitochondria facilitate gas exchange directly in the lungs.
- Mitochondria require oxygen to produce ATP, which powers cellular functions. (correct)
- Mitochondria remove carbon dioxide from the blood.
Which of the following structures is primarily responsible for warming and moistening air as it enters the respiratory system?
Which of the following structures is primarily responsible for warming and moistening air as it enters the respiratory system?
- Trachea
- Nasal cavity and sinuses (correct)
- Alveoli
- Larynx
What structural feature of the pharynx contributes to the filtering of air?
What structural feature of the pharynx contributes to the filtering of air?
Which structure prevents solids and liquids from entering the trachea?
Which structure prevents solids and liquids from entering the trachea?
What is the significance of the cardiac notch in the left lung?
What is the significance of the cardiac notch in the left lung?
Which of the following lists the correct order of structures air passes through as it moves deeper into the bronchial tree?
Which of the following lists the correct order of structures air passes through as it moves deeper into the bronchial tree?
What is the primary function of alveolar macrophages?
What is the primary function of alveolar macrophages?
How does the mucociliary escalator protect the respiratory system?
How does the mucociliary escalator protect the respiratory system?
What is the role of the C-shaped cartilaginous rings in the trachea?
What is the role of the C-shaped cartilaginous rings in the trachea?
During inhalation, what pressure change occurs in the intrapleural cavity?
During inhalation, what pressure change occurs in the intrapleural cavity?
How does surfactant aid in ventilation?
How does surfactant aid in ventilation?
What effect does broncho-constriction have on airway resistance?
What effect does broncho-constriction have on airway resistance?
In a mixed gas, what is the relationship between total pressure and partial pressures?
In a mixed gas, what is the relationship between total pressure and partial pressures?
What drives gas exchange during external respiration?
What drives gas exchange during external respiration?
Where does external respiration primarily occur?
Where does external respiration primarily occur?
How does oxygen get transported in the blood?
How does oxygen get transported in the blood?
What is the primary difference between anatomical dead space and physiological dead space?
What is the primary difference between anatomical dead space and physiological dead space?
During forced breathing, which of the following occurs?
During forced breathing, which of the following occurs?
What is alveolar ventilation a measure of?
What is alveolar ventilation a measure of?
Consider a scenario where the partial pressure of oxygen in the alveoli is significantly lower than normal. Which of the following would be the MOST likely consequence?
Consider a scenario where the partial pressure of oxygen in the alveoli is significantly lower than normal. Which of the following would be the MOST likely consequence?
A patient has a condition that increases the amount of mucus produced in their airways. How will this affect their breathing?
A patient has a condition that increases the amount of mucus produced in their airways. How will this affect their breathing?
A person is experiencing an allergic reaction that causes their bronchioles to constrict. Predict the immediate physiological response.
A person is experiencing an allergic reaction that causes their bronchioles to constrict. Predict the immediate physiological response.
A mountain climber ascends to high altitude where the partial pressure of oxygen in the air is significantly reduced. Which of the following compensatory mechanisms would be MOST beneficial in the short term?
A mountain climber ascends to high altitude where the partial pressure of oxygen in the air is significantly reduced. Which of the following compensatory mechanisms would be MOST beneficial in the short term?
If a person's tidal volume is 500 mL and their physiological dead space is 150 mL, what is their alveolar ventilation rate if they are breathing at a rate of 12 breaths per minute?
If a person's tidal volume is 500 mL and their physiological dead space is 150 mL, what is their alveolar ventilation rate if they are breathing at a rate of 12 breaths per minute?
Flashcards
Respiratory System Function
Respiratory System Function
Transports oxygen to cells and removes carbon dioxide.
Secondary Functions of the Respiratory System
Secondary Functions of the Respiratory System
Regulates blood pH, aids vocalization and circulation, and enables smell.
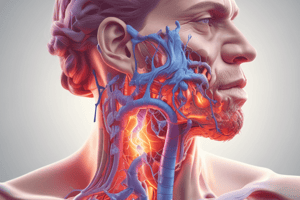
Major Respiratory Structures
Major Respiratory Structures
Nostrils, nasal cavity, sinuses, pharynx, larynx, trachea, and lungs.
Function of Nostrils, Nasal Cavity, and Sinuses
Function of Nostrils, Nasal Cavity, and Sinuses
Signup and view all the flashcards
Pharynx Function
Pharynx Function
Signup and view all the flashcards
Larynx Function
Larynx Function
Signup and view all the flashcards
Trachea Function
Trachea Function
Signup and view all the flashcards
Lungs
Lungs
Signup and view all the flashcards
Bronchial Tree
Bronchial Tree
Signup and view all the flashcards
Alveolar Sacs
Alveolar Sacs
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Respiratory System Defense Against Temperature and Moisture
Respiratory System Defense Against Temperature and Moisture
Signup and view all the flashcards
Role of Nasal Conchae and Pharynx in Defense
Role of Nasal Conchae and Pharynx in Defense
Signup and view all the flashcards
Sneeze Reflex
Sneeze Reflex
Signup and view all the flashcards
Mucociliary Escalator
Mucociliary Escalator
Signup and view all the flashcards
Tonsils
Tonsils
Signup and view all the flashcards
Trachea Structure
Trachea Structure
Signup and view all the flashcards
Alveolar Macrophages
Alveolar Macrophages
Signup and view all the flashcards
Inhalation (Inspiration)
Inhalation (Inspiration)
Signup and view all the flashcards
Exhalation (Expiration)
Exhalation (Expiration)
Signup and view all the flashcards
Forced Breathing
Forced Breathing
Signup and view all the flashcards
Surfactant
Surfactant
Signup and view all the flashcards
Airway Resistance
Airway Resistance
Signup and view all the flashcards
Partial Pressure Gradients
Partial Pressure Gradients
Signup and view all the flashcards
External Respiration
External Respiration
Signup and view all the flashcards
Study Notes
- Cells require energy to survive, which comes from ATP produced by mitochondria.
- Mitochondria need oxygen and glucose to create ATP.
- The primary function of the respiratory system is to deliver oxygen to cells and remove carbon dioxide waste.
- The system uses ventilation to facilitate oxygen intake and carbon dioxide removal.
- Secondary functions include regulating blood pH, vocalization, smell, and aiding circulation.
Structure and Function
- The main function is to ventilate air into the lungs and exchange oxygen and carbon dioxide between the lungs and cells.
- Three major components of the respiratory system are airways for ventilation, muscles for ventilation, and alveoli for gas exchange.
Nostrils, Nasal Cavity, and Sinuses
- These structures channel air into the pharynx.
- They warm, moisten, and filter air.
- They connect to olfactory bulbs, which are involved in smell.
- These structures are mucous membranes and are highly vascular.
Pharynx
- Channels air into the larynx.
- Warms, moistens, and filters air.
- Is made of mucous membranes, is highly vascular, and has an L-shaped bend.
Larynx
- Channels air into the trachea.
- Modulates vocalizations.
- Excludes solids and liquids from the trachea.
- Is a cartilaginous chamber with rings of muscle, glottis, epiglottis, and laryngeal muscles.
Trachea
- Channels air into the lungs.
- Is a flexible tube about 12cm long.
- Is anterior to the esophagus.
Lungs
- Large sacs containing airways and blood vessels.
- Divided into lobes by fissures.
- The right lung has three lobes.
- The left lung has two lobes to accommodate the cardiac notch for the heart.
Bronchial Tree
- Air flows through the trachea, bronchi, lobar bronchi, and segmental bronchi (all surrounded by cartilage).
- The air further splits into bronchioles, terminal bronchioles, respiratory bronchioles, and alveolar ducts (surrounded by smooth muscle lining).
Alveoli
- Alveolar sacs consist of multiple alveoli in a "bunch of grapes" arrangement.
- Individual alveoli are like individual grapes in the bunch.
- They have a thin film of liquid on the inside.
- Structure includes a thin membrane with a capillary network.
Defense Systems
- The body must defend against moisture, temperature, pathogens, and particulates in the atmosphere.
Temperature and Moisture Regulation
- Very dry or cold air can irritate alveoli.
- Vascular epithelium warms cold air.
- Mucous membranes moisten the air.
- Nasal conchae slow down and disrupt airflow, increasing contact with the mucous membrane for moistening and warming.
Particulates and Pathogens
- Nasal conchae, nasal hairs, and the L-shaped bend in the pharynx slow airflow.
- This increases the likelihood of particulates and pathogens interacting with and sticking to the mucous membrane.
Sneeze Reflex
- Triggered by chemical or physical irritants in the nasal mucosa.
- Expels irritants from the body.
Mucociliary Escalator
- Goblet cells in the mucous membrane produce mucus, which traps debris.
- The mucociliary escalator sweeps debris toward the pharynx.
- Coughing expels the debris, or it is swallowed.
Tonsils
- Located in the mucous membrane of the pharynx.
- Detect and trap inhaled pathogens.
- Pathogens are flushed via the lymph system once a certain amount is collected.
Trachea Form
- C-shaped cartilaginous rings with muscles in between allow expansion and prevent blockages.
Alveolar Macrophages
- Phagocytic cells in alveoli walls.
- Destroy particulates and pathogens.
- Collect dust particles.
Ventilation
- Pressure is the force exerted on a container by its contents.
- A pressure gradient moves contents from a higher-pressure container to a lower-pressure one to equalize pressure.
Process of Ventilation
- Two stages include inhalation and exhalation.
Inhalation/Inspiration
- The diaphragm contracts and ribs expand, increasing pressure in the intrapleural cavity.
- This causes the lungs to expand.
- A pressure gradient is created between the lungs and the atmosphere, causing air to enter the lungs.
Expiration/Exhalation
- Ribs and diaphragm relax, causing the lungs to contract.
- Air escapes the lungs due to the pressure difference with the atmosphere.
Forced Breathing
- Used when more oxygen is needed.
- Extra muscles are engaged during inhalation to expand the ribs more than usual.
- Extra muscles are engaged during exhalation to contract ribs more than usual.
Surface Tension in the Alveoli
- A liquid layer inside alveoli assists with gas exchange, provides a barrier, and prevents drying out.
- Surface tension exerts inward pressure.
- Without air remaining, surface tension could cause collapse upon exhalation (making inflation difficult).
- Surfactant reduces the surface tension of water, which makes it easier to inflate the alveolus.
Airway Resistance
- Airflow through airways is driven by pressure gradients.
- Resistance, or friction against the walls of airways, slows airflow.
- Airways are surrounded by smooth muscle.
- Bronchoconstriction and bronchodilation alter resistance.
- Constrictive lung diseases increase airway resistance, making inhalation difficult.
Gases, Location, and Purpose
- Total pressure is the sum of all partial pressures in a mixed gas.
Partial Pressure Gradients
- Partial pressures equalize overall pressure.
Types of Gas Exchange
- Both types are driven by diffusion across membranes down partial pressure gradients.
External Respiration
- Occurs between the alveoli in the lungs and the atmosphere.
- Alveoli in lungs have high oxygen and low carbon dioxide.
- Deoxygenated blood has low oxygen and high carbon dioxide.
- Oxygen diffuses into the blood, and carbon dioxide diffuses out.
Internal Respiration
- Occurs between the cells interior and oxygenated blood.
- Cell interior has low oxygen and high carbon dioxide.
- Oxygenated blood has high oxygen and low carbon dioxide.
- Oxygen enters the cell, and carbon dioxide enters the blood.
Conducting Zone
- Passage for moving air into and out of lungs where gas exchange does not occur.
- Anatomical dead space in males is about 150ml
Anatomical Dead Space
- Volume of air in the conducting zone, ~150ml in males.
Physiologic Dead Space
- Combination of anatomical dead space and alveolar dead space.
- Alveolar dead space is the volume of air in the respiratory zone not involved in gas transfer.
- Alveolar dead space is usually negligible in healthy people.
Alveolar Ventilation
- Air volume available for gas exchange per breath = (tidal volume - physiological dead space) x breaths per minute = liters per minute
Respiratory Zone
- Surfaces involved in gas exchange.
Gas Transport in Blood
- Arterial blood concentration = ~20ml O2 / 100ml blood.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.