Podcast
Questions and Answers
What is the primary function of the respiratory system?
What is the primary function of the respiratory system?
- Excretion of waste products
- Circulation of blood
- Gas exchange (correct)
- Nutrient absorption
Internal respiration refers to the exchange of gases between the lung tissues and blood.
Internal respiration refers to the exchange of gases between the lung tissues and blood.
False (B)
Name one function of the respiratory system aside from gas exchange.
Name one function of the respiratory system aside from gas exchange.
Regulates blood pH
The portion of the respiratory system that includes the nose and nasal cavity is called the _____ upper _____ respiratory system.
The portion of the respiratory system that includes the nose and nasal cavity is called the _____ upper _____ respiratory system.
Match the parts of the respiratory system with their descriptions:
Match the parts of the respiratory system with their descriptions:
What physiological response occurs when blood pH is low?
What physiological response occurs when blood pH is low?
Hypocapnia can result from hyperventilation.
Hypocapnia can result from hyperventilation.
Name one effect of increased blood pressure on respiration rate.
Name one effect of increased blood pressure on respiration rate.
The response to low blood pH involves the stimulation of the _____ to increase breathing.
The response to low blood pH involves the stimulation of the _____ to increase breathing.
Match the following terms with their correct descriptions:
Match the following terms with their correct descriptions:
Which of the following describes the effect of emotions on the respiratory system?
Which of the following describes the effect of emotions on the respiratory system?
The inflation reflex prevents underinflation of the lungs during exercise.
The inflation reflex prevents underinflation of the lungs during exercise.
What variable is primarily increased during exercise that stimulates the DRG?
What variable is primarily increased during exercise that stimulates the DRG?
What separates the left and right halves of the nasal cavity?
What separates the left and right halves of the nasal cavity?
The vocal folds are made of keratinized stratified squamous epithelium.
The vocal folds are made of keratinized stratified squamous epithelium.
What is the primary function of the tonsils?
What is the primary function of the tonsils?
The tube comprising nine rings of cartilage that connects the pharynx to the trachea is called the ________.
The tube comprising nine rings of cartilage that connects the pharynx to the trachea is called the ________.
Match the following parts of the larynx with their descriptions:
Match the following parts of the larynx with their descriptions:
Which of the following structures is responsible for swirling inhaled air in the nasal cavity?
Which of the following structures is responsible for swirling inhaled air in the nasal cavity?
The trachea is anterior to the esophagus.
The trachea is anterior to the esophagus.
What type of cartilage forms the anterior surface of the larynx, commonly known as the Adam's apple?
What type of cartilage forms the anterior surface of the larynx, commonly known as the Adam's apple?
The ridge at the branch point of the trachea that triggers the cough reflex is called the ________.
The ridge at the branch point of the trachea that triggers the cough reflex is called the ________.
What type of epithelium lines the oropharynx?
What type of epithelium lines the oropharynx?
What is the primary function of pleural fluid?
What is the primary function of pleural fluid?
The inferior portion of the lungs is called the apex.
The inferior portion of the lungs is called the apex.
What are the two types of cells found in the alveoli?
What are the two types of cells found in the alveoli?
The space between the lungs is called the ________.
The space between the lungs is called the ________.
Match the following parts of the lung with their respective functions:
Match the following parts of the lung with their respective functions:
Which structure permits the passage of bronchi, blood vessels, nerves, and lymphatic vessels?
Which structure permits the passage of bronchi, blood vessels, nerves, and lymphatic vessels?
What percentage of hemoglobin is almost saturated at a partial pressure of oxygen (PO2) between 60–100 mm Hg?
What percentage of hemoglobin is almost saturated at a partial pressure of oxygen (PO2) between 60–100 mm Hg?
Hemoglobin consists of four protein subunits, each containing one heme molecule.
Hemoglobin consists of four protein subunits, each containing one heme molecule.
The left lung has a middle lobe.
The left lung has a middle lobe.
What is the purpose of surfactant in the alveoli?
What is the purpose of surfactant in the alveoli?
What molecule binds to the iron atom in heme?
What molecule binds to the iron atom in heme?
Hb has a low affinity for oxygen at _____ pH.
Hb has a low affinity for oxygen at _____ pH.
The ________ bronchi branch into segmental bronchi.
The ________ bronchi branch into segmental bronchi.
Which of the following describes Boyle's Law?
Which of the following describes Boyle's Law?
Match the following terms with their definitions:
Match the following terms with their definitions:
What is the role of 2,3-bisphosphoglycerate (BPG) in the body?
What is the role of 2,3-bisphosphoglycerate (BPG) in the body?
The bronchial arteries deliver deoxygenated blood to the lung tissue.
The bronchial arteries deliver deoxygenated blood to the lung tissue.
The pulmonary capillaries are where carbon dioxide is absorbed into the bloodstream.
The pulmonary capillaries are where carbon dioxide is absorbed into the bloodstream.
How does inhalation occur with respect to pressure changes?
How does inhalation occur with respect to pressure changes?
The ________ membrane consists of the alveoli and associated capillaries.
The ________ membrane consists of the alveoli and associated capillaries.
What is the primary role of the dorsal respiratory group (DRG)?
What is the primary role of the dorsal respiratory group (DRG)?
Carbon dioxide in the blood is primarily transported as _____ bicarbonate.
Carbon dioxide in the blood is primarily transported as _____ bicarbonate.
What term describes the ability of a passageway to remain unobstructed?
What term describes the ability of a passageway to remain unobstructed?
Gas exchange occurs in the alveoli.
Gas exchange occurs in the alveoli.
What happens to the affinity of hemoglobin for oxygen as temperature increases?
What happens to the affinity of hemoglobin for oxygen as temperature increases?
Erythrocytes have mitochondria and produce energy through aerobic respiration.
Erythrocytes have mitochondria and produce energy through aerobic respiration.
Which two centers in the brain regulate the action of respiratory muscles?
Which two centers in the brain regulate the action of respiratory muscles?
At systemic capillaries, the saturation of hemoglobin is approximately _____%.
At systemic capillaries, the saturation of hemoglobin is approximately _____%.
Match the chemoreceptors with their locations:
Match the chemoreceptors with their locations:
What is the primary function of the diaphragm during inhalation?
What is the primary function of the diaphragm during inhalation?
Exhalation is typically an active process.
Exhalation is typically an active process.
What are the two main components that ensure lung tissue expands during inhalation?
What are the two main components that ensure lung tissue expands during inhalation?
The contraction of the diaphragm ________ the thoracic cavity by approximately ________ cm during normal inhalation.
The contraction of the diaphragm ________ the thoracic cavity by approximately ________ cm during normal inhalation.
Match the following pulmonary conditions with their effects:
Match the following pulmonary conditions with their effects:
During strenuous inhalation, how much can the diaphragm be depressed?
During strenuous inhalation, how much can the diaphragm be depressed?
Compliance refers to the distensibility of elastic tissues.
Compliance refers to the distensibility of elastic tissues.
What is the primary gas that affects the rate of respiration due to its higher solubility in water?
What is the primary gas that affects the rate of respiration due to its higher solubility in water?
The movement of gases in the body occurs from areas of ________ partial pressure to areas of ________ partial pressure.
The movement of gases in the body occurs from areas of ________ partial pressure to areas of ________ partial pressure.
What percentage of oxygen in blood is transported on hemoglobin?
What percentage of oxygen in blood is transported on hemoglobin?
Air through the respiratory system faces resistance regardless of airway diameter.
Air through the respiratory system faces resistance regardless of airway diameter.
What is the term used for the accumulation of pleural fluid in the pleural cavity?
What is the term used for the accumulation of pleural fluid in the pleural cavity?
Gas exchange between the alveoli and blood occurs during ________ respiration.
Gas exchange between the alveoli and blood occurs during ________ respiration.
Which factor does NOT affect the rate of passive diffusion of gases?
Which factor does NOT affect the rate of passive diffusion of gases?
What process occurs when tissue cells produce carbon dioxide?
What process occurs when tissue cells produce carbon dioxide?
Flashcards
Pulmonary Ventilation
Pulmonary Ventilation
The process of moving air between the atmosphere and the lungs. This involves inhalation (taking air in) and exhalation (expelling air).
External Respiration
External Respiration
The exchange of gases between the lungs and the blood. Oxygen from the inhaled air moves into the bloodstream, while carbon dioxide from the blood moves into the lungs to be exhaled.
Internal Respiration
Internal Respiration
The exchange of gases between the blood and the body's tissues. Oxygen from the blood moves into the cells for energy production, and carbon dioxide produced by the cells moves into the blood to be transported to the lungs.
Upper Respiratory System
Upper Respiratory System
Signup and view all the flashcards
Lower Respiratory System
Lower Respiratory System
Signup and view all the flashcards
Nasal Cavity
Nasal Cavity
Signup and view all the flashcards
Nasal Septum
Nasal Septum
Signup and view all the flashcards
What are paranasal sinuses?
What are paranasal sinuses?
Signup and view all the flashcards
Nasal Conchae
Nasal Conchae
Signup and view all the flashcards
Olfactory Epithelium
Olfactory Epithelium
Signup and view all the flashcards
Pharynx
Pharynx
Signup and view all the flashcards
Nasopharynx
Nasopharynx
Signup and view all the flashcards
Larynx
Larynx
Signup and view all the flashcards
Thyroid Cartilage
Thyroid Cartilage
Signup and view all the flashcards
Epiglottis
Epiglottis
Signup and view all the flashcards
Pleural Membrane
Pleural Membrane
Signup and view all the flashcards
Pleural Cavity
Pleural Cavity
Signup and view all the flashcards
What does pleural fluid do?
What does pleural fluid do?
Signup and view all the flashcards
Mediastinum
Mediastinum
Signup and view all the flashcards
Lung Base
Lung Base
Signup and view all the flashcards
Lung Apex
Lung Apex
Signup and view all the flashcards
Hilum
Hilum
Signup and view all the flashcards
Cardiac Notch
Cardiac Notch
Signup and view all the flashcards
Fissures
Fissures
Signup and view all the flashcards
Oblique Fissure
Oblique Fissure
Signup and view all the flashcards
Lobar Bronchi
Lobar Bronchi
Signup and view all the flashcards
Bronchopulmonary Segment
Bronchopulmonary Segment
Signup and view all the flashcards
Lobules
Lobules
Signup and view all the flashcards
Respiratory Bronchioles
Respiratory Bronchioles
Signup and view all the flashcards
Alveoli
Alveoli
Signup and view all the flashcards
Low blood pH
Low blood pH
Signup and view all the flashcards
Hyperventilation
Hyperventilation
Signup and view all the flashcards
Hypocapnia
Hypocapnia
Signup and view all the flashcards
Hypoxia
Hypoxia
Signup and view all the flashcards
Inflation Reflex
Inflation Reflex
Signup and view all the flashcards
Baroreceptors
Baroreceptors
Signup and view all the flashcards
Vagus Nerve
Vagus Nerve
Signup and view all the flashcards
Pulmonary Perfusion
Pulmonary Perfusion
Signup and view all the flashcards
Diaphragm's role in inhalation
Diaphragm's role in inhalation
Signup and view all the flashcards
Intercostal muscle assistance
Intercostal muscle assistance
Signup and view all the flashcards
Diaphragm's impact on pressure
Diaphragm's impact on pressure
Signup and view all the flashcards
Role of external intercostal muscles
Role of external intercostal muscles
Signup and view all the flashcards
Intrapleural pressure
Intrapleural pressure
Signup and view all the flashcards
Passive exhalation
Passive exhalation
Signup and view all the flashcards
Active exhalation
Active exhalation
Signup and view all the flashcards
Surfactant's role
Surfactant's role
Signup and view all the flashcards
Compliance
Compliance
Signup and view all the flashcards
Resistance in the respiratory system
Resistance in the respiratory system
Signup and view all the flashcards
Lung volume
Lung volume
Signup and view all the flashcards
Lung capacity
Lung capacity
Signup and view all the flashcards
Gases move by diffusion
Gases move by diffusion
Signup and view all the flashcards
Solubility of gases
Solubility of gases
Signup and view all the flashcards
CO2 solubility vs. O2
CO2 solubility vs. O2
Signup and view all the flashcards
Hemoglobin's Structure
Hemoglobin's Structure
Signup and view all the flashcards
Hemoglobin Saturation
Hemoglobin Saturation
Signup and view all the flashcards
What makes Hb bind/release oxygen?
What makes Hb bind/release oxygen?
Signup and view all the flashcards
Acidity and Hb affinity
Acidity and Hb affinity
Signup and view all the flashcards
CO2 and Hb affinity
CO2 and Hb affinity
Signup and view all the flashcards
Temperature and Hb affinity
Temperature and Hb affinity
Signup and view all the flashcards
BPG and Hb affinity
BPG and Hb affinity
Signup and view all the flashcards
Fetal Hb vs. Adult Hb
Fetal Hb vs. Adult Hb
Signup and view all the flashcards
CO2 Transport: Dissolved
CO2 Transport: Dissolved
Signup and view all the flashcards
CO2 Transport: Bound to proteins
CO2 Transport: Bound to proteins
Signup and view all the flashcards
CO2 Transport: Bicarbonate
CO2 Transport: Bicarbonate
Signup and view all the flashcards
Chloride Shift
Chloride Shift
Signup and view all the flashcards
Reverse Chloride Shift
Reverse Chloride Shift
Signup and view all the flashcards
Respiratory Centre Location
Respiratory Centre Location
Signup and view all the flashcards
Medulla Oblongata Role
Medulla Oblongata Role
Signup and view all the flashcards
Pons Role
Pons Role
Signup and view all the flashcards
Study Notes
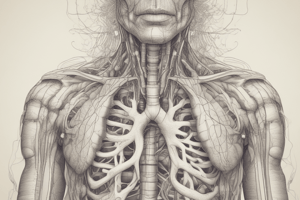
Respiration Overview
- Respiration is the process of acquiring oxygen and eliminating carbon dioxide.
- Three steps occur within the human body:
- Pulmonary ventilation: Gas exchange between the atmosphere and lung tissues.
- External respiration: Gas exchange between lung tissues and blood.
- Internal respiration: Gas exchange between blood and body tissues.
- Respiratory system functions:
- Gas exchange.
- Regulates blood pH.
- Phonation (speech), sense of smell, filters inhaled air, and excretes wastes during exhalation.
- Oto(rhino)laryngology is the study of the respiratory system.
- Cells need oxygen for aerobic cellular respiration.
Anatomy of the Respiratory System
- Structurally divided into:
- Upper respiratory system: Nose, nasal cavity, pharynx, and associated structures.
- Lower respiratory system: Larynx, trachea, bronchi, and lungs.
- Functionally divided into:
- Conducting zone: Directs air towards the respiratory zone; filters, warms, and humidifies air.
- Respiratory zone: Site of gas exchange; includes respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli.
Upper Respiratory System
- Nose: Made of bone, cartilage, and connective tissues; has external nares (nostrils).
- Nasal Cavity: Interior anterior space of the nose, divided by the nasal septum, contains conchae (swirl air), olfactory epithelium (smell receptors).
- Pharynx: Tube of skeletal muscle with mucosa:
- Nasopharynx (superior): Ciliated pseudostratified columnar epithelium; sweeps mucus to pharynx.
- Oropharynx (intermediate): Common passage for air and food; non-keratinized stratified squamous epithelium.
- Laryngopharynx (inferior): Similar to oropharynx, but inferior.
Larynx
- Nine rings of cartilage:
- Thyroid cartilage: Anterior surface of larynx; Adam's apple (larger in males).
- Epiglottis: Flap of elastic cartilage; covers larynx opening during swallowing.
- Cricoid cartilage: Inferior ring of larynx.
- Vocal cords/folds:
- True vocal cords (inferior): Non-keratinized stratified squamous epithelium, generate sound.
- False vocal cords (superior): Protect true cords.
Trachea
- 2.5 cm wide x 12 cm long tube, 16-20 C-shaped hyaline cartilage rings.
- Cartilage maintains patency (openness).
- Anterior to the esophagus; lined with ciliated pseudostratified epithelium.
Bronchi
- Carina: Ridge at the trachea's branch point (cough reflex trigger).
- Branch into smaller tubes (bronchial tree) ending in terminal bronchioles.
- Changes in respiratory tissues throughout bronchial tree.
Lungs
- Wrapped in pleural membrane (two membranes, pleural fluid reducing friction).
- Separated by mediastinum, lungs extend from clavicles to diaphragm.
- Hilum: Passage for bronchi, blood vessels, nerves, and lymphatic vessels.
- Cardiac Notch: Houses heart; decreases size of the left lung.
- Fissures divide lungs into lobes (oblique fissure divides superior and inferior lobes; horizontal fissure divides the middle lobe on the right lung).
- Lobar bronchi: named after the lobes they enter.
- Bronchopulmonary segments: supported by individual segmental bronchi; divisible regions for surgical removal.
- Lobules: Smaller compartments with a terminal bronchiole, vessels, and lymphatics, with elastic connective tissue.
- Respiratory bronchioles: Microscopic branches with simple cuboidal epithelium; branch into alveolar ducts. Alveolar ducts terminate in alveolar sacs.
- Alveoli: Air sacs for gas exchange; with Type I (thin squamous epithelium), and Type II (cuboidal, secrete surfactant) alveolar cells.
Respiratory Membrane
- Alveoli + associated capillaries; very thin (0.5 µm).
- Layers: Alveolar wall (Type I & II cells, macrophages), epithelial basement membrane, capillary basement membrane, capillary endothelium.
Blood Supply to Lungs
- Pulmonary arteries: Bring deoxygenated blood from right ventricle for oxygenation.
- Bronchial arteries: Deliver oxygenated blood to lung tissue from aorta.
Gas Exchanges and Ventilation
- Pulmonary ventilation is inhalation and exhalation, changing thoracic cavity pressure.
- Inhalation (inspiration):
- Decreasing lung pressure below atmospheric pressure to draw air inward.
- Diaphragm contracts, intercostal muscles contract, expanding the thoracic cavity, lungs expand too.
- Boyle's Law: Pressure inversely proportional to volume. Increasing volume lowers pressure, pulling air in.
- Exhalation (expiration):
- Passive process; respiratory muscles relax; lung recoil increases intraplural pressure.
- Gases move out.
Factors Affecting Pulmonary Ventilation
- Surfactant: Prevents alveolar collapse.
- Compliance: Chest wall and lung distensibility; high compliance = low effort to breathe; low compliance = high effort.
- Resistance: Determined by airway diameter; increased resistance = difficulties like in COPD.
Lung Volumes and Capacities
- Lung volumes: Specific measures of air; measured by spirometry.
- Lung capacities: Sums of lung volumes
Principles of Gas Exchange
- Passive diffusion from high to low partial pressure.
- Solubility: CO2 is more soluble in water than oxygen.
- External respiration: Gas exchange between alveoli and blood in pulmonary capillaries.
- Internal respiration: Gas exchange between blood and body tissues.
Oxygen Transport
- Hemoglobin (Hb) in erythrocytes transports 98.5% of oxygen.
- Hemoglobin saturation: affected by PO2 (high PO2 = high saturation), blood acidity, PCO2, temperature.
Carbon Dioxide Transport
- Three forms:
- Dissolved CO2.
- Bound to proteins/carbamino compounds.
- Bicarbonate form (majority).
- Chloride shift: Maintains erythrocyte electrical balance during CO2 transport.
Regulation of Breathing
- Respiratory center: Medulla oblongata and pons (DRG and VRG regulate breathing).
- Chemoreceptors (central & peripheral) sense changes in PCO2 and pH.
- Inflation reflex: Prevents overinflation.
- Factors affecting breathing rate: Emotions, temperature, pain, airway irritation, etc.
- Exercise effect: Increased pulmonary perfusion, ventilation, depth of breathing.
Homeostatic Imbalances
- COPD: Smoking associated disorder with impaired ciliary function, reduced alveolar surface area.
- Emphysema: Immune destruction of alveolar walls.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.