Podcast
Questions and Answers
What function do the conducting airways serve in the respiratory system?
What function do the conducting airways serve in the respiratory system?
- Trapping foreign particles in the air
- Facilitating gas exchange in the lungs
- Moving air to and from the lungs (correct)
- Protecting the lungs from infections
Which part of the lungs is responsible for the majority of gas exchange?
Which part of the lungs is responsible for the majority of gas exchange?
- Diaphragm
- Alveoli (correct)
- Pleura
- Bronchi
What term describes the movement of blood through the lungs?
What term describes the movement of blood through the lungs?
- Ventilation
- Diffusion
- Perfusion (correct)
- Inspiration
Which structure is located at the apex of the lung?
Which structure is located at the apex of the lung?
Which mechanism triggers a reflex to remove foreign particles from the air?
Which mechanism triggers a reflex to remove foreign particles from the air?
What occurs during the process of inspiration?
What occurs during the process of inspiration?
What is the primary role of the mucosal lining in the airways?
What is the primary role of the mucosal lining in the airways?
Which of the following statements about the lungs is incorrect?
Which of the following statements about the lungs is incorrect?
What is the primary reason glucocorticoids are used during acute exacerbations?
What is the primary reason glucocorticoids are used during acute exacerbations?
When administering multiple inhalers, which should be used first?
When administering multiple inhalers, which should be used first?
Which of the following is NOT a common adverse reaction associated with glucocorticoids?
Which of the following is NOT a common adverse reaction associated with glucocorticoids?
What is the therapeutic range for theophylline, which must be monitored closely?
What is the therapeutic range for theophylline, which must be monitored closely?
What should clients be advised to avoid when taking theophylline?
What should clients be advised to avoid when taking theophylline?
What should a nurse monitor for with long-term glucocorticoid therapy?
What should a nurse monitor for with long-term glucocorticoid therapy?
What is the mechanism of action of inhaled anticholinergic drugs?
What is the mechanism of action of inhaled anticholinergic drugs?
What should patients taking theophylline be educated about regarding toxicity?
What should patients taking theophylline be educated about regarding toxicity?
Which of the following interactions increases theophylline levels?
Which of the following interactions increases theophylline levels?
What nursing intervention is essential when a patient is prescribed high-dose glucocorticoids?
What nursing intervention is essential when a patient is prescribed high-dose glucocorticoids?
What does tidal volume (TV) represent?
What does tidal volume (TV) represent?
What role do peripheral chemoreceptors play in respiratory control?
What role do peripheral chemoreceptors play in respiratory control?
Which of the following correctly describes vital capacity (VC)?
Which of the following correctly describes vital capacity (VC)?
What is the primary function of lung receptors?
What is the primary function of lung receptors?
Which statement about central chemoreceptors is true?
Which statement about central chemoreceptors is true?
What characterizes forced vital capacity (FVC)?
What characterizes forced vital capacity (FVC)?
What does residual volume (RV) refer to?
What does residual volume (RV) refer to?
What occurs at the alveolar capillary junctions?
What occurs at the alveolar capillary junctions?
What is the primary action of inhaled glucocorticoids in asthma management?
What is the primary action of inhaled glucocorticoids in asthma management?
What is the duration of action for the short-acting beta 2 agonist albuterol?
What is the duration of action for the short-acting beta 2 agonist albuterol?
Which of the following should be monitored in a patient taking monoamine oxidase inhibitors (MAOI)?
Which of the following should be monitored in a patient taking monoamine oxidase inhibitors (MAOI)?
What is a common adverse reaction associated with inhaled glucocorticoids?
What is a common adverse reaction associated with inhaled glucocorticoids?
Which of the following is a common adverse reaction associated with intranasal decongestants?
Which of the following is a common adverse reaction associated with intranasal decongestants?
How often should long-acting beta 2 agonists like salmeterol and formoterol be administered?
How often should long-acting beta 2 agonists like salmeterol and formoterol be administered?
What is the primary mechanism of action for sympathomimetic decongestants?
What is the primary mechanism of action for sympathomimetic decongestants?
Which of the following best describes intranasal glucocorticoids?
Which of the following best describes intranasal glucocorticoids?
What is a recommended practice to prevent oropharyngeal candidiasis when using inhaled glucocorticoids?
What is a recommended practice to prevent oropharyngeal candidiasis when using inhaled glucocorticoids?
Which medication should not be used alone for asthma management when a glucocorticoid is ineffective?
Which medication should not be used alone for asthma management when a glucocorticoid is ineffective?
What should be avoided in patients with cardiovascular conditions when taking oral decongestants?
What should be avoided in patients with cardiovascular conditions when taking oral decongestants?
Which of these drugs is an effective non-opioid antitussive?
Which of these drugs is an effective non-opioid antitussive?
What is the typical dosing schedule for short-acting beta 2 agonists for acute bronchospasm?
What is the typical dosing schedule for short-acting beta 2 agonists for acute bronchospasm?
What potential effect can occur with the misuse of dextromethorphan?
What potential effect can occur with the misuse of dextromethorphan?
Which symptom may be a result of the adverse reactions from intranasal glucocorticoids?
Which symptom may be a result of the adverse reactions from intranasal glucocorticoids?
Which is true concerning the administration of intranasal decongestants?
Which is true concerning the administration of intranasal decongestants?
What is the primary mechanism of action for opioid cough suppressants?
What is the primary mechanism of action for opioid cough suppressants?
Which of the following is a common adverse reaction associated with opioid cough suppressants?
Which of the following is a common adverse reaction associated with opioid cough suppressants?
What should clients be advised regarding the use of guaifenesin?
What should clients be advised regarding the use of guaifenesin?
What is an important nursing intervention for clients using acetylcysteine?
What is an important nursing intervention for clients using acetylcysteine?
Which of the following statements about the administration of mucolytics is true?
Which of the following statements about the administration of mucolytics is true?
What is a key precaution to take when administering opioid cough suppressants?
What is a key precaution to take when administering opioid cough suppressants?
What might clients experience when using acetylcysteine, and what should they be informed about?
What might clients experience when using acetylcysteine, and what should they be informed about?
For which situation might laxatives be necessary when taking opioid cough suppressants?
For which situation might laxatives be necessary when taking opioid cough suppressants?
Flashcards
Respiratory System
Respiratory System
The system responsible for moving air between the atmosphere and the lungs, including the airways and lungs
Conducting Airways
Conducting Airways
The air passages that carry air to and from the lungs, but do not participate in gas exchange
Respiratory Tissues
Respiratory Tissues
The part of the lungs where gas exchange happens
Ventilation
Ventilation
Signup and view all the flashcards
Inspiration
Inspiration
Signup and view all the flashcards
Expiration
Expiration
Signup and view all the flashcards
Perfusion
Perfusion
Signup and view all the flashcards
Diffusion
Diffusion
Signup and view all the flashcards
Respiratory Control Centers
Respiratory Control Centers
Signup and view all the flashcards
Lung Receptors
Lung Receptors
Signup and view all the flashcards
What do chemoreceptors sense?
What do chemoreceptors sense?
Signup and view all the flashcards
Central Chemoreceptors
Central Chemoreceptors
Signup and view all the flashcards
Peripheral Chemoreceptors
Peripheral Chemoreceptors
Signup and view all the flashcards
Tidal Volume (TV)
Tidal Volume (TV)
Signup and view all the flashcards
Vital Capacity (VC)
Vital Capacity (VC)
Signup and view all the flashcards
Gas Exchange
Gas Exchange
Signup and view all the flashcards
Opioid Cough Suppressants
Opioid Cough Suppressants
Signup and view all the flashcards
Guaifenesin
Guaifenesin
Signup and view all the flashcards
Acetylcysteine
Acetylcysteine
Signup and view all the flashcards
Adverse Reactions of Opioid Cough Suppressants
Adverse Reactions of Opioid Cough Suppressants
Signup and view all the flashcards
Drug and Food Interactions of Opioid Cough Suppressants
Drug and Food Interactions of Opioid Cough Suppressants
Signup and view all the flashcards
Nursing Interventions for Opioid Cough Suppressants
Nursing Interventions for Opioid Cough Suppressants
Signup and view all the flashcards
Nursing Interventions for Guaifenesin
Nursing Interventions for Guaifenesin
Signup and view all the flashcards
Nursing Interventions for Acetylcysteine
Nursing Interventions for Acetylcysteine
Signup and view all the flashcards
Second Generation Antihistamines
Second Generation Antihistamines
Signup and view all the flashcards
Sympathomimetic Decongestants
Sympathomimetic Decongestants
Signup and view all the flashcards
Intranasal Decongestants: Onset and Effects
Intranasal Decongestants: Onset and Effects
Signup and view all the flashcards
Oral Decongestants: Onset and Effects
Oral Decongestants: Onset and Effects
Signup and view all the flashcards
Intranasal Decongestant Rebound Congestion
Intranasal Decongestant Rebound Congestion
Signup and view all the flashcards
Intranasal Glucocorticoids for Allergies
Intranasal Glucocorticoids for Allergies
Signup and view all the flashcards
Intranasal Glucocorticoid Administration
Intranasal Glucocorticoid Administration
Signup and view all the flashcards
Dextromethorphan: Non-opioid Cough Suppressant
Dextromethorphan: Non-opioid Cough Suppressant
Signup and view all the flashcards
MAOIs
MAOIs
Signup and view all the flashcards
Beta 2 Agonists
Beta 2 Agonists
Signup and view all the flashcards
Short-Acting Beta 2 Agonists
Short-Acting Beta 2 Agonists
Signup and view all the flashcards
Long-Acting Beta 2 Agonists
Long-Acting Beta 2 Agonists
Signup and view all the flashcards
Inhaled Glucocorticoids
Inhaled Glucocorticoids
Signup and view all the flashcards
Oral Candidiasis (Thrush)
Oral Candidiasis (Thrush)
Signup and view all the flashcards
What is the purpose of gargling after using an inhaled glucocorticoid?
What is the purpose of gargling after using an inhaled glucocorticoid?
Signup and view all the flashcards
Glucocorticoids for Asthma
Glucocorticoids for Asthma
Signup and view all the flashcards
Glucocorticoid Administration
Glucocorticoid Administration
Signup and view all the flashcards
Glucocorticoid Timing
Glucocorticoid Timing
Signup and view all the flashcards
Glucocorticoid Long-Term Use
Glucocorticoid Long-Term Use
Signup and view all the flashcards
Glucocorticoid & Bone Health
Glucocorticoid & Bone Health
Signup and view all the flashcards
Glucocorticoid & Blood Sugar
Glucocorticoid & Blood Sugar
Signup and view all the flashcards
Glucocorticoid & GI Effects
Glucocorticoid & GI Effects
Signup and view all the flashcards
Order of Inhaler Use
Order of Inhaler Use
Signup and view all the flashcards
Theophylline: Mechanism of Action
Theophylline: Mechanism of Action
Signup and view all the flashcards
Theophylline: Adverse Reactions
Theophylline: Adverse Reactions
Signup and view all the flashcards
Study Notes
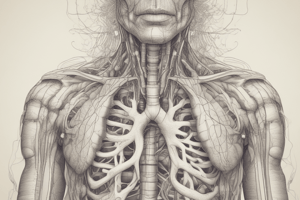
Respiratory System
- The respiratory system comprises the air passages and the lungs.
- It's divided into two parts based on function:
- Conducting airways: air moves through these passages from the atmosphere to the lungs.
- Respiratory tissues: gas exchange occurs within these tissues.
- Lungs are soft, spongy, cone-shaped organs located in the chest cavity.
- They are separated by the mediastinum and are divided into lobes (three in the right lung, two in the left).
- The apex (top) of the lung lies against the top of the thoracic cavity.
- The base (bottom) of the lung lies against the diaphragm.
Respiratory Structures
- The structures involved in respiration include:
- Nasal cavity
- Nasopharynx
- Oropharynx
- Epiglottis
- Laryngeal pharynx
- Esophagus
- Visceral pleura
- Parietal pleura
- Upper lobe of right lung
- Right main bronchus
- Trachea
- Left main bronchus
- Middle lobe
- Lower lobe
- Bronchioles
- Alveolar duct
- Alveolus
- Pulmonary vein
- Respiratory bronchioles
- Lobules
- Pulmonary artery
- Surfactant
- Alveolar macrophage
- Red blood cell
- Capillary
- Alveolar epithelium
- Alveolar capillary junction
- Alveolar basement membrane
- Mediastinum
- Diaphragm
Protective Structures
- Hairs and turbinates in the nose trap and remove foreign particles.
- Cilia in the upper and lower airways remove particles along with mucus.
- The mucosal lining warms and humidifies air.
- Irritant receptors trigger a sneeze or cough reflex to remove irritants.
- Immune protections include an immune coating in the respiratory tract mucosa, and macrophages in the alveoli.
Ventilation
- Depends on the conducting airways including:
- Nasopharynx
- Oropharynx
- Larynx
- Tracheobronchial tree
- Main function is to move air into and out of the lungs without participating in gas exchange.
- Inspiration is the drawing of air into the lungs as respiratory muscles expand the chest cavity.
- Expiration is the movement of air out of the lungs as the chest muscles recoil and the chest cavity becomes smaller.
Respiratory Control
- Brainstem (Pons and Medulla) control centers: Send neural impulses to the diaphragm, intercostal muscles, and accessory muscles causing contraction or relaxation.
- Lung receptors located in the epithelium and smooth muscles of airways near alveolar-capillary junctions.
- These receptors sense irritants and trigger a cough to prevent excessive lung inflation and reduce capillary pressure.
Chemoreceptors
- Key sensors for alterations in blood chemistry (oxygen, carbon dioxide, and acid-base status).
- Two types:
- Central chemoreceptors are located in the brainstem and respond to pH changes.
- Peripheral chemoreceptors are located in the carotid and aortic bodies and trigger an increase in ventilation to low oxygen levels.
Lung Capacities
- Tidal Volume (TV): Approximate volume of air that moves into and out of the lungs during a normal breath (500 ml).
- Inspiratory Reserve Volume (IRV): Additional volume of air that can be inhaled after a normal breath (Approx. 3000 ml).
- Expiratory Reserve Volume (ERV): Additional volume of air that can be exhaled after a normal breath (Approx. 1100 ml).
- Vital Capacity (VC): The maximal volume of air that can be moved in and out of the lungs. (Approx. 4600 ml). This is the sum of IRV, TV and ERV.
- Forced Vital Capacity (FVC): Maximal amount of air that can be exhaled from the lungs during forced exhalation.
- Residual Volume (RV): Amount of air that remains in the lungs after maximum exhalation.
- Total Lung Capacity (TLC): Total amount of air in the lungs when they are maximally expanded. This is the sum of VC and RV.
Diffusion
- Oxygen and carbon dioxide are exchanged at alveolar capillary junctions.
- Effectiveness depends on partial pressure and solubility of gases, as well as the thickness of membranes.
Partial Pressure
- The collision of oxygen and carbon dioxide creates pressure.
- Partial pressure of oxygen (PaO2) in arterial blood.
- Partial pressure of carbon dioxide (PaCO2) in arterial blood. Both are measured in mm Hg.
Gas Exchange
- The exchange of gases (oxygen and carbon dioxide) between the alveoli and blood.
Alveolar Gas Exchange
- Oxygen moves from the alveoli into the capillaries, and carbon dioxide moves from the capillaries into the alveoli.
- This is driven by differences in partial pressure.
Oxygen and Carbon Dioxide Transport
- PaO2 of arterial blood normally is above 80 mm Hg.
- PaO2 is a major factor in determining the percentage of hemoglobin bound to oxygen (known as oxygen saturation).
- Carbon dioxide is transported dissolved in plasma, as bicarbonate, or bound to hemoglobin.
Carbon Dioxide Diffusion and Transport
- Carbon dioxide is a cellular waste product released into the bloodstream.
- It's dissolved in the plasma, bound to hemoglobin, and diffused into red blood cells as bicarbonate.
- It diffuses through the alveolar capillary junction to be exhaled through the lungs.
Functions of Bronchial Smooth Muscle
- Tone of the bronchial smooth muscles surrounding the airways determines the airway radius.
- The presence or absence of airway secretions influences airway patency.
- Bronchial smooth muscle is innervated by the autonomic nervous system (sympathetic, parasympathetic).
Impaired Ventilation
- A problem of blocking air flow in and out of the lungs due to compression or narrowing of the airways.
- Also, disruption of the neuronal transmissions needed to stimulate the mechanics of breathing.
Impaired Diffusion
- Restricted transfer of oxygen or carbon dioxide across the alveolar capillary junction.
- Depends on solubility, partial pressure of the gas, and membrane thickness and surface area.
Impaired Ventilation-Perfusion (V/Q) Matching
- Causes of increased V/Q ratio (lung ventilated but not perfused):
- Emphysema
- Heart disease
- Pulmonary hypertension
- Liver disease
- Causes of decreased V/Q ratio (lung perfused but not ventilated):
- COPD
- Chronic bronchitis
- Asthma
- Pulmonary edema
- Airway obstruction
- Pneumonia
Altered Ventilation and Diffusion
- Obstruction or restriction of airflow: examples are bronchoconstriction and suffocation.
- Inhibition of neural stimulation/mechanics of breathing: examples are drug overdose and cervical nerve damage.
- Increased thickness or decreased surface area of alveolar-capillary junction
- Decreased partial pressure or decreased solubility of gases.
General Manifestations of Impaired Ventilation and Diffusion
- Cough, mucus, hemoptysis
- Dyspnea, orthopnea
- Adventitious lung sounds
- Use of accessory respiratory muscles
- Chest pain
- Barrel chest
Effects of Impaired Ventilation and Diffusion
- Hypoxemia: Decreased oxygen in arterial blood, leads to decrease in PaO2.
- Hypoxia: Oxygen deprivation in the cells.
- Hypercapnia: Increase in carbon dioxide in the blood.
Hypoxemia
- Results from inadequate oxygen in the air or disease of the respiratory system, dysfunction of the neurological system, or alterations in circulatory function.
- Mechanisms include hypoventilation, impaired diffusion of gases, or inadequate circulation through the pulmonary capillaries, or mismatching of ventilation and perfusion.
Hypercapnia
- Caused by hypoventilation or mis-match between ventilation and perfusion
- Common causes include COPD and sleep apnea
Symptoms of Respiratory Distress and Hypoxia
- Early: restlessness, tachycardia, tachypnea, exertional dyspnea, orthopnea, anxiety.
- Late: extreme restlessness, severe dyspnea, slowing of respiratory rate, bradycardia, peripheral or central cyanosis, and intercostal retractions
Cyanosis
- Oxygen saturation < 85%.
- Discoloration of the skin (bluish or purple)
- Different types:
- Central: skins and lips affected
- Peripheral: hands, fingers, feet, and toes
- Circumoral (perioral): only the mouth and lips affected
Clubbing
- Caused by chronic low blood oxygen.
Treating Impaired Ventilation and Diffusion
- Remove obstructions
- Restore integrity of chest wall and lungs
- Decrease inflammation and mucus
- Open and maintain integrity of airways
- Provide supplemental oxygen
- Control infectious processes
- Use mechanical ventilation when needed (priority).
Lab or Diagnostic Tests (for respiratory problems)
- Pulmonary function test (PFTs): evaluate lung function during breathing.
- Arterial blood gas (ABG): determines acid-base imbalances, and the degree of hypoxemia and hypercapnia in arterial blood.
- Pulse oximetry: non-invasive; measures oxygen saturation in the blood.
- Bronchoscopy: direct visualization of bronchioles.
- Radiograph, CT, MRI: detect structural problems, presence of consolidation, obstruction, or cavities in the lungs
- Nuclear (V/Q) lung scan: detects pulmonary embolism, and lung diseases like COPD and emphysema by using radioactive material inspired into the lungs.
- Culture and sensitivity test: determines microorganisms in blood or sputum from the lungs to dictate appropriate antibiotic treatment (if indicated).
- Thoracentesis: determines presence of pleural effusion.
Alterations of the Respiratory System
- Asthma, Pneumonia, COPD (including emphysema and chronic bronchitis), Acute respiratory distress syndrome (ARDS), Respiratory Syncytial Virus (RSV), and COVID-19
Asthma
- Intermittent or persistent airway obstruction due to bronchial hyper-responsiveness, chronic inflammation, bronchoconstriction, and excess mucous production.
- Pathogenesis: allergens trigger mast cells to release mediators leading to bronchoconstriction and inflammation causing airflow limitation and increased airway responsiveness.
Asthma Pathophysiology
- Tracheal and bronchial linings overreact to stimuli (allergens, etc).
- Smooth muscle spasms constrict airways.
- Mucosal edema and thickened secretions further block airways.
- IgE antibodies attached to mast cells combine with antigens.
Asthma Pathogenesis
- Allergen triggers mast cells, releasing histamine, leukotrienes, interleukins, and prostaglandins
- Inflammatory cells infiltrate the airways and release cytokines and other mediators
- Edema and epithelial injury lead to impaired mucociliary function.
- Airflow limitation and increased airway responsiveness occur.
Asthma Attack Anatomy
- Inhaled air → primary bronchi → trachea → bronchial tubes→alveoli.
Asthma: Narrowed Bronchiole
- Airway obstructed with mucus plug or spasm in the bronchioles.
- Blood vessels engorged from inflammation.
Asthma Causes
-
Extrinsic:
- Pollen
- Animal dander
- Feather or down pillows
- Dust or mold
- Irritants or noxious fumes
- Variations in temperature or humidity
- Food additives containing sulfites
-
Intrinsic
- Emotional stress or anxiety
- Fatigue
- Endocrine changes (hypo/hyperthyroidism)
- Genetic predisposition
- Physical exertion
Asthma Pathophysiologic Changes Asthma
- Sudden dyspnea, wheezing, chest tightness, diminished breath sounds (due to bronchial constriction)
- Initially non-productive cough.
- Later, coughing with thick, clear, or yellow sputum (due to excess mucous).
- Tachycardia, tachypnea, use of accessory respiratory muscles (due to hypoxemia).
Asthma Treatment
- Stepwise approach based on asthma severity
- Control of symptoms: ranged from controlled to very poorly controlled.
- Mild intermittent, mild persistent, moderate persistent, severe persistent.
Chronic Obstructive Pulmonary Disease (COPD)
- Emphysema and chronic bronchitis.
- Emphysema: permanent enlargement of air sacs (alveoli) and destruction of lung tissue caused by chronic smoking.
- Chronic bronchitis: chronic inflammation of the bronchial lining with an accumulation of mucus, often in the setting of smoking, but other causes exist.
Emphysema
- Irreversible enlargement of the air spaces beyond terminal bronchioles.
- Destruction of alveolar walls → obstruction of airflow.
- Chronic smoking is a major cause
Emphysema Clinical Manifestations
- Persistent cough
- Dyspnea
- Wheezing
- Barrel chest
- Pursed lip breathing
Emphysema Treatment
- Maintain optimal lung function
- Smoking cessation
- Pharmacologic therapy (possibly)
- Lung volume reduction or transplant (possibly).
Chronic Bronchitis
- Persistent, productive cough lasting ≥3 months, for ≥2 consecutive years.
- Chronic inflammation and edema of airways.
- Hyperplasia of bronchial mucus glands & smooth muscles.
- Destruction of cilia.
- Squamous cell metaplasia.
- Bronchial wall thickening, fibrosis
Chronic Bronchitis Clinical Manifestations
- Productive cough
- Purulent sputum
- Dyspnea
- Adventitious lung sounds
- Hypoxemia and hypercapnia
- Cyanosis ("Blue Bloater")
Chronic Bronchitis Treatment
- Smoking cessation
- Pulmonary rehabilitation
- Pharmacologic therapy:
- Bronchodilators
- Steroidal anti-inflammatory drugs
- Mucolytic agents
- Supplemental oxygen
Management of COPD
- Measurement of lung function.
- Classification of COPD severity (mild, moderate, severe, very severe)
Management of Stable COPD
- Pharmacologic management:
- Bronchodilators
- Glucocorticoids
- Phosphodiesterase-4 inhibitors (PDE4 inhibitor)
Management of COPD Exacerbations
- Pharmacologic management:
- Short-acting beta agonists (SABAs) - specifically inhaled.
- Inhaled anticholinergics
- Systemic glucocorticoids
- Antibiotics
- Supplemental oxygen (to maintain oxygen saturation of 88% - 92%).
Pneumonia
- Infectious process; respiratory droplet spread.
- Causes inflammation in the lungs, mostly in bronchioles, interstitial lung tissue, and alveoli.
- Products of inflammation accumulate → consolidation.
Pneumonia Clinical Manifestations
- Sudden onset fever
- Chills
- Cough
- Sputum production
- Fatigue
- Loss of appetite
- Dyspnea
- Tachypnea
- Tachycardia
- Pleuritic pain
- Crackles in lungs
Pneumonia Diagnostic Criteria
- History and physical examination
- Complete blood cell count
- Chest X-ray
- Thoracic CT scan
- Gram stain
- Culture and sensitivity test
- Pulse oximetry and arterial blood gases
Classifications of Pneumonia
- Source of infection: Community-acquired, Hospital-acquired
- Immune status of host: Pneumonia in the immunocompromised person.
Pneumonia Treatment
- Restore optimal ventilation and diffusion
- Identify pathogen and target with appropriate pharmacologic treatment
- Supplemental oxygen
Acute Respiratory Distress Syndrome (ARDS)
- Progression from lung injury to respiratory distress within 24 to 48 hours.
- Severe acute inflammation and pulmonary edema (without fluid overload or impaired cardiac function).
- Mortality rate 30-40% if untreated. (multisystem organ failure).
- Caused by injury to alveolar and pulmonary capillaries, which causes inflammatory mediators to increase capillary permeability. This leads to increased interstitial osmotic pressure and pulmonary edema.
ARDS Pathophysiology
- Progression from lung injury to respiratory distress within 24-48 hours.
- Severe acute inflammation and pulmonary edema.
ARDS Phases 1 and 2
- Phase 1: injury reduces blood flow; results in platelets aggregating and releasing histamine, serotonin, and bradykinin.
- Phase 2: these substances damage the alveolar-capillary membrane, increasing capillary permeability. Fluid shifts to the interstitial space.
ARDS Phases 3 and 4
- Phase 3: capillary permeability increases resulting to fluid and protein leakage; increasing interstitial osmotic pressure causing pulmonary edema.
- Phase 4: decreased blood flow and fluids in the alveoli cause surfactant damage and impair production; resulting in alveoli collapse. This impedes gas exchange and decreases lung compliance.
ARDS Phases 5 and 6
- Phase 5: insufficient oxygen can cross alveolar-capillary junction, but carbon dioxide can release. Oxygen and carbon dioxide levels decrease.
- Phase 6: pulmonary edema worsens causing inflammation to lead to fibrosis impeding gas exchange even further.
ARDS Treatment
- Humidified oxygen
- Ventilatory support
- Sedatives, opioids, neuromuscular blockers
- Sodium bicarbonate
- IV fluids, vasopressors (to maintain blood pressure).
COVID-19
- A novel coronavirus that causes respiratory symptoms (ranging from mild to severe).
- Life-threatening coronaviruses include SARS-CoV, MERS-CoV, and SARS-CoV-2.
- Symptoms: early includes fever, nausea, vomiting, diarrhea, sore throat, cough, dyspnea.
- Later include hypoxia (cyanosis, confusion, somnolence, chest pain/pressure), anosmia/ageusia, malaise, myalgia, fatigue, anorexia.
- Attacks alveolar epithelial cells and capillary endothelial cells; can cause strong inflammatory response leading to cytokine storm, pulmonary edema and ARDS.
- Other organ systems can be affected and hypercoagulability can lead to clots.
- Post-acute complications ("Long Covid-19"): fatigue, dyspnea, arthralgias, lingering lung damage (impaired diffusion capacity & restrictive lung damage)
- Death risk increased in vulnerable populations (elderly, obese, pre-existing disease)
RSV
- Common viral infection of the lungs
- Most children have RSV once by age 2.
- Severe RSV is seen in babies under 12 months or older patients.
RSV Symptoms
- Congested or runny nose
- Dry cough
- Low-grade fever
- Sore throat
- Sneezing
- Headache
RSV Prevention
- Hand washing
- Avoiding exposure (November-March)
- Avoiding smoking
- Pharmacology for preventing RSV infection in infants, children, and elderly (ex: nirsevimab, aka Beyfortus) - antibody injection
RSV Diagnosis and Treatment
- Diagnosis: physical symptoms, labs (CBC), rapid antigen test (swab), X-rays
- Treatment: supportive care (fever reducers, nasal drops); hospitalization if severe (fluids, oxygen)
Pharmacology (general notes)
- Targets components of illness (bronchoconstriction and inflammation).
- Guidelines for treating asthma and COPD are available from GINA or similar resources.
Administration of Asthma Drugs
- Technique for using inhalers is critical for effective drug delivery to the lung site..
- Types of inhalers: Metered dose inhalers (MDIs), dry-powder inhalers (DPIs), and nebulizers.
Asthma, COPD, and Other Respiratory Medicines
- Short-acting beta agonists (SABAs), inhaled corticosteroids (inhalers), combination therapies (inhalers) are commonly used.
- Other add-on medications exist (e.g., monoclonal antibodies, PDE4 inhibitors, long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LAMAs)
- Use a valved holding chamber/spacer with HFA inhalers to help manage drug delivery more effectively.
Beta-2 Agonists
- Drugs: Albuterol, salmeterol, levalbuterol, formoterol
- MOA: activate beta-2 receptors in lungs, causing bronchodilation
- Administration: inhaled (preferred over oral).
- Adverse reactions: tachycardia, tremor, angina
- Drug-food interactions: beta blockers (especially non-selective) and MAOIs.
- Nursing considerations: monitor heart rate (avoid >20 bpm from baseline); monitor for angina symptoms (chest pain, arm pain, palpitations; avoid substances with caffeine).
Inhaled Glucocorticoids
- Drugs include: beclomethasone, fluticasone, budesonide.
- MOA: primarily suppress inflammation, may increase beta receptors, & decrease mucous production..
- Uses: maintenance/prophylaxis of asthma (fixed schedule).
- Adverse reactions: hoarseness, oropharyngeal candidiasis ("thrush")
- Nursing interventions: monitor for oral candidiasis; advise clients to rinse and spit after inhaler use, report any oral white patches.
Glucocorticoids for acute exacerbations
- Drugs = Prednisone, methylprednisolone
- Administration= mainly oral, or IV
- Use = short high-dose course (5-7 days) for exacerbations (reduces inflammation)
- Adverse reactions = include adrenal suppression, osteoporosis, hyperglycemia, GI upset and peptic ulcer.
- Interventions: Taper dose, monitor glucose, advise clients to take with food. Monitor for infections.
Order of Inhaler Use
- If multiple inhalers are used, the short-acting beta-2 agonist is usually administered first, followed by the glucocorticoid. Time administration of different medications by 5 minutes or as directed.
Theophylline
- MOA: relaxes smooth muscles of bronchi causing bronchodilation.
- Uses: for some with chronic asthma (not preferred for acute exacerbations), nocturnal symptoms.
- Administration: oral (dose individualized), IV for emergencies (as aminophylline).
- Adverse reactions: include nausea, constipation, dizziness, sedation, and GI effects. Food and Drug interactions: Avoid caffeine, cigarettes, Ciprofloxacin, and other medications that may increase blood levels.
- Nursing evaluations/interventions: Monitor for toxicity—therapeutic range is 5-15 mcg/mL, and adjust dosages accordingly. Advise clients to avoid caffeine and smoking, monitor for cardiac symptoms
Inhaled Anticholinergics
- Drugs: Ipratropium, tiotropium, and aclidinium.
- MOA: block muscarinic receptors in the bronchi to reduce bronchoconstriction.
- Administration: inhaled; do not swallow tiotropium capsules.
- Adverse reactions: some anticholinergic side effects can occur (dry mouth, headache; glaucoma). Soy lecithin is in some meds, so be careful.
Leukotriene Modifiers
- Drug = Montelukast
- MOA = blocks leukotriene receptors, reducing inflammation, edema, and decreased mucus plugging.
- Use= maintenance/prophylaxis of asthma (adults and children—over 6 months of age).
- Admin= by mouth at bedtime.
- Adverse reactions: serious neuropsychiatric disorders (suicide ideations/depression/aggressive behavior). Nursing Evaluation: monitor behavioral changes and advise clients to report any signs of these problems.
Antihistamines
- Drugs = diphenhydramine, chlorpheniramine (first generation); cetirizine, fexofenadine, loratadine, azelastine (second generation).
- MOA: inhibit H1 receptors at various sites to block histamine effects, reducing edema, redness, itching, etc.
- Uses: treat allergy and cold symptoms, allergies.
- Nursing considerations with first generation are that they are sedating and cause anticholinergic effects that are serious for the elderly.
Sympathomimetic Decongestants
- Drugs= pseudoephedrine, phenylephrine, oxymetazoline (ex: Afrin nasal drops).
- MOA: stimulate alpha-1 adrenergic receptors on blood vessels, leading to vasoconstriction, reducing edema.
- Uses= reducing nasal congestion.
- Intranasal may cause intense and rapid action, but rebound congestion may occur if administered chronically.
- Oral may cause delaying onset, but effects are more prolonged.
- Nursing consideration when administering oral or intranasal include: monitor for symptoms indicating overstimulation of the central nervous system (ex= tachycardia, increased BP or agitation).
Intranasal Glucocorticoids
- Drugs= mometasone, budesonide, fluticasone.
- First-line therapy for chronic allergic rhinitis.
- MOA= suppress inflammatory response to allergens..
- Dosage and administration: typically daily, used before symptoms start.
- Adverse reactions: localized nasal side effects (bleeding, burning, itching) or rare systemic effects (ex= adrenal suppression)
Non-Opioid Cough Suppressants
- Drug= dextromethorphan, benzonatate
- MOA= dextromethorphan is most effective but is non-opiod and opioid-derived; benzonatate is derived from tetracaine which works as a local anesthetic.
- Benzonatate reduces sensitivity so it shouldn't be chewed.
- Adverse Reactions = potential for euphoria with dextromethorphan at higher doses, and some local anesthetic effects.
- Additional Considerations = avoid use with MAOIs.
Opioid Cough Suppressants
- Drugs = opioids (codeine, hydrocodone/combination with other meds)
- MOA = suppress cough reflex directly, affecting the cough center in the brain.
- Adverse reactions = GI upset (nausea, constipation), CNS effects (dizziness, sedation), respiratory depression.
- Nursing considerations = advise that drugs should be taken with food if nausea is suspected or advise of additional effects if driving or operating dangerous machinery.
- Additional considerations: Abuse potential exists.
Expectorants- Guaifenesin
- Drug= Guaifenesin (ex= Robitussin, Mucinex)
- MOA= Stimulates respiratory secretions, making coughs more productive.
- Adverse Reactions: GI upset, dizziness/drowsiness, which warrants counseling on driving or operating dangerous machinery.
- Additional Nursing Considerations = recommend fluid intake.
Mucolytics (e.g., Acetylcysteine)
- Drug = acetylcysteine.
- MOA = decreases viscosity of mucus, enhancing flow.
- Administration = Usually via inhalation given orally or intravenously for overdose scenarios.
- Adverse reactions: Bronchospasm—possible concern in people with asthma..
- Nursing evaluations = education about smell, monitoring for aspiration, and providing suction (if necessary). Monitor for bronchospasm in clients with asthma.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.