Podcast
Questions and Answers
What indicates a potential reversible airway obstruction?
What indicates a potential reversible airway obstruction?
- Improvement in FEV1 or FVC by at least 12% (correct)
- Increase in RV
- Decrease in TLC
- Normal FEV1/FVC ratio
Which measurement is NOT consistent with restrictive lung disease?
Which measurement is NOT consistent with restrictive lung disease?
- Decreased FEV1/FVC ratio (correct)
- Decreased RV
- Decreased TLC
- Decreased FRC
What is the characteristic feature of a combined respiratory disorder?
What is the characteristic feature of a combined respiratory disorder?
- Decreased TLC with decreased FEV1 and FEV1/FVC (correct)
- Increased TLC with decreased FEV1
- Normal TLV and FEV1
- Increased RV with normal FEV1/FVC
Which blood gas value would indicate respiratory alkalosis?
Which blood gas value would indicate respiratory alkalosis?
How is indicated metabloic acidosis determined?
How is indicated metabloic acidosis determined?
Which condition is associated with a normal PFT but decreased DLCO?
Which condition is associated with a normal PFT but decreased DLCO?
What is the primary factor indicating respiratory failure in ABG values?
What is the primary factor indicating respiratory failure in ABG values?
What is indicated by a pH of 7.35?
What is indicated by a pH of 7.35?
What characterizes uncompensated acid-base imbalance?
What characterizes uncompensated acid-base imbalance?
Which imaging technique is primarily used for soft tissue visualization?
Which imaging technique is primarily used for soft tissue visualization?
What is the normal range for PaO2 levels?
What is the normal range for PaO2 levels?
What is the main purpose of a pulmonary angiogram?
What is the main purpose of a pulmonary angiogram?
Which condition indicates moderate hypoxemia?
Which condition indicates moderate hypoxemia?
What is the typical tidal volume for adults?
What is the typical tidal volume for adults?
Which surgical procedure involves the removal of an entire lung?
Which surgical procedure involves the removal of an entire lung?
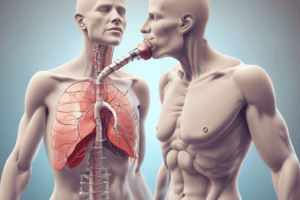
What best describes a bronchoscopy?
What best describes a bronchoscopy?
What is a common complication associated with lung transplants?
What is a common complication associated with lung transplants?
What is the purpose of a radionuclide V/Q scan?
What is the purpose of a radionuclide V/Q scan?
What is the primary benefit of early mobilization for post-operative patients?
What is the primary benefit of early mobilization for post-operative patients?
Which condition is NOT an indication for oxygen therapy?
Which condition is NOT an indication for oxygen therapy?
Which mode of mechanical ventilation allows spontaneous breathing with machine support?
Which mode of mechanical ventilation allows spontaneous breathing with machine support?
What is the primary risk associated with hyperoxia during oxygen therapy?
What is the primary risk associated with hyperoxia during oxygen therapy?
Which component is NOT part of a tracheostomy tube?
Which component is NOT part of a tracheostomy tube?
What does the Positive End Expiratory Pressure (PEEP) do during ventilation?
What does the Positive End Expiratory Pressure (PEEP) do during ventilation?
Which medication type is specifically used to manage airway secretions?
Which medication type is specifically used to manage airway secretions?
What does the Oxygen Extraction Ratio (OER) indicate?
What does the Oxygen Extraction Ratio (OER) indicate?
Which is an accurate statement regarding Non-Invasive Ventilation (NIV)?
Which is an accurate statement regarding Non-Invasive Ventilation (NIV)?
What is the main purpose of suctioning during mechanical ventilation?
What is the main purpose of suctioning during mechanical ventilation?
Which condition would contraindicate the use of Positive Pressure Ventilation (PPV)?
Which condition would contraindicate the use of Positive Pressure Ventilation (PPV)?
What is the role of iron lung in mechanical ventilation?
What is the role of iron lung in mechanical ventilation?
What parameter indicates that a patient might be fatiguing on mechanical ventilation?
What parameter indicates that a patient might be fatiguing on mechanical ventilation?
What is the significance of the rate at which the ventilator delivers breaths?
What is the significance of the rate at which the ventilator delivers breaths?
How does oxygen delivery (DO2) change during exercise in a healthy individual?
How does oxygen delivery (DO2) change during exercise in a healthy individual?
What is the primary purpose of Oxygen Debt or Deficit during recovery?
What is the primary purpose of Oxygen Debt or Deficit during recovery?
Which of the following is NOT a task needed after strenuous exercise?
Which of the following is NOT a task needed after strenuous exercise?
What effect does exercise have on oxygen extraction in the body?
What effect does exercise have on oxygen extraction in the body?
In the context of inspiratory muscle training, which condition is optimal for patients with a tidal volume (VT) higher than 500?
In the context of inspiratory muscle training, which condition is optimal for patients with a tidal volume (VT) higher than 500?
What is the main goal of the Active Cycles of Breathing (ACB) technique?
What is the main goal of the Active Cycles of Breathing (ACB) technique?
What happens during the Collection phase of Autogenic Drainage (AD)?
What happens during the Collection phase of Autogenic Drainage (AD)?
What effect does increased temperature have on oxygen transport?
What effect does increased temperature have on oxygen transport?
What characterizes the inspiratory phase of an effective cough?
What characterizes the inspiratory phase of an effective cough?
Which variable is used to calculate maximum heart rate according to the formula HRMax = 208 – 0.7(age)?
Which variable is used to calculate maximum heart rate according to the formula HRMax = 208 – 0.7(age)?
In the context of percussion during respiratory therapy, what is the intended outcome?
In the context of percussion during respiratory therapy, what is the intended outcome?
What does the term 'forced expiratory technique' refer to in the ACB approach?
What does the term 'forced expiratory technique' refer to in the ACB approach?
What is the recommended duration for maintaining postural drainage in each segmented position?
What is the recommended duration for maintaining postural drainage in each segmented position?
Which breath sound is associated with fluid in the airways and is often described as fine or coarse?
Which breath sound is associated with fluid in the airways and is often described as fine or coarse?
What lung disease is characterized by irreversible dilation of bronchi and can lead to frequent infections and purulent sputum?
What lung disease is characterized by irreversible dilation of bronchi and can lead to frequent infections and purulent sputum?
Which breath sound indicates airflow obstruction at the upper airway, often associated with foreign bodies or laryngeal edema?
Which breath sound indicates airflow obstruction at the upper airway, often associated with foreign bodies or laryngeal edema?
What type of lung sound would be expected if there is abnormal airflow in the lower lung regions due to consolidation?
What type of lung sound would be expected if there is abnormal airflow in the lower lung regions due to consolidation?
In the context of pulmonary diseases, what does a hyper-resonant sound typically indicate?
In the context of pulmonary diseases, what does a hyper-resonant sound typically indicate?
Which condition is characterized by a chronic inflammation of the airways leading to episodic respiratory distress and increased mucosal edema?
Which condition is characterized by a chronic inflammation of the airways leading to episodic respiratory distress and increased mucosal edema?
What test result would typically be seen in a patient with restrictive lung disease due to pulmonary fibrosis?
What test result would typically be seen in a patient with restrictive lung disease due to pulmonary fibrosis?
Which type of cough is commonly associated with pneumonia due to infection in the lower respiratory tract?
Which type of cough is commonly associated with pneumonia due to infection in the lower respiratory tract?
What lung sound may indicate the presence of a pleural effusion?
What lung sound may indicate the presence of a pleural effusion?
What breathing pattern is most commonly affected in acute respiratory distress syndrome (ARDS)?
What breathing pattern is most commonly affected in acute respiratory distress syndrome (ARDS)?
Which of the following conditions results in a loud or dull percussion note when the affected area of the lung is examined?
Which of the following conditions results in a loud or dull percussion note when the affected area of the lung is examined?
What is the typical auscultation finding in a patient with pulmonary embolism?
What is the typical auscultation finding in a patient with pulmonary embolism?
What characteristic cough is associated with bronchitis, particularly in the morning hours?
What characteristic cough is associated with bronchitis, particularly in the morning hours?
In the context of lung diseases, what classifies Acute Respiratory Distress Syndrome (ARDS) as a restrictive lung disease?
In the context of lung diseases, what classifies Acute Respiratory Distress Syndrome (ARDS) as a restrictive lung disease?
Flashcards
Obstructive Lung Disease
Obstructive Lung Disease
A decreased FEV1 (forced expiratory volume in one second) and FEV1/FVC (forced expiratory volume in one second / forced vital capacity) ratio, along with an increased RV (residual volume) and potentially normal or increased TLC (total lung capacity).
Restrictive Lung Disease
Restrictive Lung Disease
A decrease in TLC (total lung capacity) accompanied by a decrease in RV (residual volume), VC (vital capacity), FRC (functional residual capacity), and FEV1/FVC within normal limits.
Combined Lung Disorder
Combined Lung Disorder
A combination of decreased TLC (total lung capacity) with associated decreased flow, indicated by reduced FEV1 (forced expiratory volume in one second) and FEV1/FVC (forced expiratory volume in one second / forced vital capacity) ratio.
Isolated Gas Exchange Abnormality
Isolated Gas Exchange Abnormality
Signup and view all the flashcards
Acid-Base Balance
Acid-Base Balance
Signup and view all the flashcards
Metabolic Acidosis
Metabolic Acidosis
Signup and view all the flashcards
Metabolic Alkalosis
Metabolic Alkalosis
Signup and view all the flashcards
Alveolar Ventilation
Alveolar Ventilation
Signup and view all the flashcards
Uncompensated Acid-Base Disturbance
Uncompensated Acid-Base Disturbance
Signup and view all the flashcards
Partially Compensated Acid-Base Disturbance
Partially Compensated Acid-Base Disturbance
Signup and view all the flashcards
Compensated Acid-Base Disturbance
Compensated Acid-Base Disturbance
Signup and view all the flashcards
Wedge Resection
Wedge Resection
Signup and view all the flashcards
Bullectomy
Bullectomy
Signup and view all the flashcards
Lobectomy
Lobectomy
Signup and view all the flashcards
Pneumonectomy
Pneumonectomy
Signup and view all the flashcards
Lung Volume Reduction Surgery (LVRS)
Lung Volume Reduction Surgery (LVRS)
Signup and view all the flashcards
Lung Transplant
Lung Transplant
Signup and view all the flashcards
Thoracotomy
Thoracotomy
Signup and view all the flashcards
Convective Oxygen Transport
Convective Oxygen Transport
Signup and view all the flashcards
Diffusive Oxygen Transport
Diffusive Oxygen Transport
Signup and view all the flashcards
Oxygen Demand
Oxygen Demand
Signup and view all the flashcards
Oxygen Delivery (DO2)
Oxygen Delivery (DO2)
Signup and view all the flashcards
Oxygen Consumption (VO2)
Oxygen Consumption (VO2)
Signup and view all the flashcards
Oxygen Extraction Ratio (OER)
Oxygen Extraction Ratio (OER)
Signup and view all the flashcards
Basal Metabolic Rate (BMR)
Basal Metabolic Rate (BMR)
Signup and view all the flashcards
MET (Metabolic Equivalent)
MET (Metabolic Equivalent)
Signup and view all the flashcards
Maximum Oxygen Consumption (VO2max)
Maximum Oxygen Consumption (VO2max)
Signup and view all the flashcards
Peak Oxygen Consumption (VO2peak)
Peak Oxygen Consumption (VO2peak)
Signup and view all the flashcards
Effect of Exercise on DO2 and VO2
Effect of Exercise on DO2 and VO2
Signup and view all the flashcards
Recruitment
Recruitment
Signup and view all the flashcards
Derecruitment
Derecruitment
Signup and view all the flashcards
Positive End Expiratory Pressure (PEEP)
Positive End Expiratory Pressure (PEEP)
Signup and view all the flashcards
Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP)
Signup and view all the flashcards
Wheezes/Rhonchi
Wheezes/Rhonchi
Signup and view all the flashcards
Percussion
Percussion
Signup and view all the flashcards
Crackles/Rales
Crackles/Rales
Signup and view all the flashcards
Tracheal Breath Sounds
Tracheal Breath Sounds
Signup and view all the flashcards
Adventitious Breath Sounds
Adventitious Breath Sounds
Signup and view all the flashcards
Vesicular Breath Sounds
Vesicular Breath Sounds
Signup and view all the flashcards
Bronchial Breath Sounds
Bronchial Breath Sounds
Signup and view all the flashcards
Pleural Rub
Pleural Rub
Signup and view all the flashcards
Wheezes
Wheezes
Signup and view all the flashcards
Stridor
Stridor
Signup and view all the flashcards
Pulmonary Function Testing (PFT)
Pulmonary Function Testing (PFT)
Signup and view all the flashcards
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD)
Signup and view all the flashcards
Lung Function Test
Lung Function Test
Signup and view all the flashcards
Resting Oxygen Delivery (DO2)
Resting Oxygen Delivery (DO2)
Signup and view all the flashcards
Exercise and Oxygen Delivery
Exercise and Oxygen Delivery
Signup and view all the flashcards
Oxygen Debt or Deficit
Oxygen Debt or Deficit
Signup and view all the flashcards
Post Exercise Oxygen Consumption (PEOC)
Post Exercise Oxygen Consumption (PEOC)
Signup and view all the flashcards
Factors that Perturb Oxygen Transport
Factors that Perturb Oxygen Transport
Signup and view all the flashcards
Exercise Stress and Oxygen Transport
Exercise Stress and Oxygen Transport
Signup and view all the flashcards
Maximum Heart Rate (HRMax)
Maximum Heart Rate (HRMax)
Signup and view all the flashcards
6-Minute Walk Test
6-Minute Walk Test
Signup and view all the flashcards
Heart Rate Reserve (HRR) Calculation
Heart Rate Reserve (HRR) Calculation
Signup and view all the flashcards
VO2 Reserve Calculation
VO2 Reserve Calculation
Signup and view all the flashcards
MET Level
MET Level
Signup and view all the flashcards
Postural Drainage
Postural Drainage
Signup and view all the flashcards
Percussion (P)
Percussion (P)
Signup and view all the flashcards
Vibration
Vibration
Signup and view all the flashcards
Study Notes
Pulmonary Breath Sounds
- Tracheal: Normal air movement through the trachea. Loud, high-pitched, equal inspiratory/ expiratory phases (1:1).
- Bronchial: Air moving through large airways. High pitched, hollow, louder expiration than inspiration (1:2).
- Bronchovesicular: Air movement in mid-sized airways. Moderate pitch and intensity, equal inspiration/expiration phases (1:1).
- Vesicular: Air moving through small airways. Soft, low pitched, longer inspiration than expiration (3:1).
- Crackles/Rales: Fluid or alveolar popping, represents wetness in the airways. Consistent sound; associated with pneumonia, heart failure, pulmonary fibrosis, or atelectasis.
- Wheezes/Rhonchi: Airflow obstruction, usually heard during exhalation (bronchoconstriction/secretions). Associated with asthma, COPD, bronchitis. Continuous, high-pitched sound. Rhonchi are lower pitched and snoring, often clearing with coughing.
- Stridor: Airflow obstruction at upper airway. Continuous, high-pitched sound; associated with epiglottis, foreign body, laryngeal edema.
- Pleural Rub: Visceral and parietal pleura rubbing together. Creaking or grating sound, heard during both inspiration and exhalation. Associated with pleuritis or pleural effusion.
Mediate Percussion Sounds
- Resonant: Loud/low pitched, heard over air-filled organs (lungs).
- Hyper Resonant: Very low-pitched, heard over tissue with decreased density (diseased lungs, emphysema, inflated lungs).
- Tympanic: High-pitched, heard over hollow organs, (stomach/gas bubbles).
- Dull: Low amplitude, medium to high-pitched, heard over solid organs (lungs with increased tissue density); decreased air.
- Flat: Very dull sound/high pitch; very dense tissues; heard over muscle mass.
Lung Diseases/Pathology
- Bronchitis (Blue Bloater): Airway disease, inflammation of bronchi, obstruction of airways, alveolar wall destruction. Associated with PFT: decreased VC, increased TLC, and RV; CXR: overinflated lungs/horizontal ribs/increased subcostal angle. Barrel chest, slower/shallower breaths, increased vibration over mucosal areas, and dull sounds over the mucosal area.
- Emphysema (Pink Puffer): Abnormal/irreversible enlargement of airways distal to terminal bronchioles. Associated with PFT: decreased VC, increased TLC, and RV; CXR: overinflated lungs/horizontal ribs/increased subcostal angle. Barrel chest, short/faster breath sounds, signs of right heart failure, flat diaphragm, and less fremitus (vibration).
- Asthma: Chronic, reversible obstruction to airflow, bronchospasm. Associated with CXR: hyperinflation. Wheezing, exhalation longer than inhalation. Possible small areas of atelectasis
- Bronchiectasis: Abnormal, permanent dilation of bronchi/bronchioles; chronic inflammation/infection; destruction of elastic and muscular tissue. PFT: with advanced disease may see decreased FEV1 and increased RV. Frequent infections and muscopurulent sputum. Dyspnea, clubbing.
- Cystic Fibrosis: Obstructive disease characterized by thick, excessive secretions and poor ciliary function, leading to obstruction of small airways, affecting bronchial hygiene.
- Bronchopulmonary Dysplasia (BPD): Obstructive/restrictive disease. Associated with underdeveloped lungs, inflammation, scarring of lungs, and most common in children (often related to birth complications).
- Pulmonary Fibrosis: Restrictive lung disease. Associated with scarring, stiffness, and decreased compliance of alveolar walls and stiffness of tissues. Progressive shortness of breath, nonproductive cough, and dyspnea.
- Pneumonia: Restrictive. Inflammation of the lung, often starting in the lower respiratory tract due to infection. Associated with crackles and low-pitched wheezing, bronchial breath sounds over area of consolidation, and abnormal sputum/culture.
- Acute Respiratory Distress Syndrome (ARDS): Restrictive. Sudden respiratory failure due to fluid accumulating in alveoli. Diffuse crackles, wet breath sounds, decreased breath sounds; other symptoms include dyspnea, labored/rapid breathing.
- Lung Cancer: Restrictive. Malignant tumor in the lung. Diminished breath sounds, crackles/wheezing. Other symptoms may include persistent non-productive coughing up blood, chest pain.
- Pleural Effusion: Restrictive. Fluid in the pleural space. Contains decreased breath sounds, pleural rub.
- Atelectasis: Restrictive. Partial or total collapse of alveoli or lung segments/lobes. Reduced breath sounds, diminished or absent breath sounds over affected areas.
- Pneumothorax: Restrictive. Presence of air in the pleural cavity. Absent or diminished breath sounds. Associated symptoms include chest pain, hyperresonance on percussion, decreased tactile fremitus.
COVID-19
- Hypoxemic disease, may scar lungs. Shortness of breath, cough, body/muscle aches, headaches, loss of taste/smell, sore throat/congestion, runny nose, nausea/vomiting, diarrhea, multi-organ failure.
Diagnostic Testing
- Pulmonary Function Tests (PFTs): Measure the volume and flow of air during inspiration and exhalation.
- Chest X-rays (CXR): Allow visualization of the anatomy of the chest.
- Computed tomography (CT) scans: Allow visualization of tissues; used for pulmonary nodules.
- Magnetic Resonance Imaging (MRI): Used for soft tissue and lymph nodes.
Lung Volume/Capacities
- Tidal Volume (TV): Volume of air inhaled and exhaled during normal breathing.
- Inspiratory Reserve Volume (IRV): Maximum volume of air that can be inhaled after normal inspiration.
- Expiratory Reserve Volume (ERV): Maximum volume of air that can be exhaled after normal expiration.
- Residual Volume (RV): Volume of air remaining in the lungs after maximum exhalation.
- Inspiratory Capacity (IC): Maximum volume of air that can be inhaled.
- Functional Residual Capacity (FRC): Volume of air remaining in the lungs at the end of normal expiration.
- Vital Capacity (VC): Maximum volume of air that can be exhaled from a maximum inhalation.
- Total Lung Capacity (TLC): Total volume of air that the lungs can hold.
Surgical Interventiions
- Wedge Resection: Removal of section of lung tissue (triangle shaped).
- Bullectomy: Removal of 1 or more bullae.
- Lobectomy: Excision of lobe.
- Pneumonectomy: Removal of the entire lung.
- Lung Volume Reduction Surgery (LVRS): Reducing the size of lungs to minimize diseased tissue portion.
- Lung Transplant: Replacing a failing lung with a healthy one from a donor.
Pulmonary Angiogram
- Catheter inserted carefully to the pulmonary artery, dye injected to show blood flow.
- X-Ray imaging of blood flow, and detection of blockages.
Bronchoscopy
- Direct visualization of bronchial tree with a scope. Used for diagnosis and therapy.
Radionuclide Ventilation/Perfusion Scan (V/Q scan)
- Ventilation and perfusion should match.
- Poor ventilation may indicate airway obstruction.
- Poor perfusion may indicate blood flow issues (pulmonary embolism).
Oxygen Therapy
- Indications: Hypoxemia, increased work of breathing, increased myocardial work, and decreased exercise/activity tolerance.
Artificial Airways
- Reasons for intubation include airway obstruction.
- Intubation/ventillation may be necessary for patients with apnea (no breathing), ventilatory failure, airway infections, or protective airway issues resulting in aspiration.
- Common types of artificial airways, include endotracheal and tracheostomy tubes
Mechanical Ventilation
- Positive pressure ventilation is used when breathing is laboured or absent.
- Positive pressure is applied to the airway via endotracheal or tracheostomy tube to deliver gas/air into the lungs.
- PPV modes include: controlled modes (ventilator delivers all breaths at a preset frequency) and assist/control modes (ventilator delivers breaths only if patient does not initiate one).
Mechanical and Spontaneous Breaths
- Pressure Support (PS): Constant pressure, but the volume needed to reach the pressure may vary depending on lung compliance and patient effort. Allows patient to control rate and volume of breathing.
Negative Pressure Ventilator
- Also referred to as an Iron Lung, and delivers negative pressure/vacuum to expand patient's chest to allow air to flow into lungs.
Other considerations
- Chest tubes may be inserted to remove secretions or drain fluid surrounding lung tissue.
- Suctioning procedures can be conducted to remove secretions or mucus.
- Coughing exercises and postural drainage to mobilize secretions.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.