Podcast
Questions and Answers
What is the primary stimulant for central chemoreceptors?
What is the primary stimulant for central chemoreceptors?
- Decreased partial pressure of CO2 in blood
- Increased hydrogen ion concentration (correct)
- Increased partial pressure of CO2 in blood
- Increased partial pressure of O2 in blood
What is the response of peripheral chemoreceptors to a reduction in partial pressure of oxygen?
What is the response of peripheral chemoreceptors to a reduction in partial pressure of oxygen?
- No response
- Strong inhibition
- Mild stimulation
- Strong stimulation (correct)
What is the function of chemoreceptors in the regulation of respiration?
What is the function of chemoreceptors in the regulation of respiration?
- To regulate body temperature
- To decrease ventilation in response to hypoxia
- To increase ventilation in response to hypercapnea (correct)
- To control blood pressure
Where are peripheral chemoreceptors located?
Where are peripheral chemoreceptors located?
What happens to the excess carbon dioxide in the blood when ventilation increases?
What happens to the excess carbon dioxide in the blood when ventilation increases?
Why can't hydrogen ions from the blood directly stimulate central chemoreceptors?
Why can't hydrogen ions from the blood directly stimulate central chemoreceptors?
What is the result of carbon dioxide combining with water in the brain?
What is the result of carbon dioxide combining with water in the brain?
What type of impulses do chemoreceptors send to the dorsal respiratory group of neurons?
What type of impulses do chemoreceptors send to the dorsal respiratory group of neurons?
What is the total lung capacity (TLC) in milliliters?
What is the total lung capacity (TLC) in milliliters?
What is the term for the volume of air remaining in the lungs after a normal expiration?
What is the term for the volume of air remaining in the lungs after a normal expiration?
Which of the following factors contributes to lung compliance?
Which of the following factors contributes to lung compliance?
What is the normal value of pulmonary ventilation?
What is the normal value of pulmonary ventilation?
Which of the following is NOT a component of vital capacity (VC)?
Which of the following is NOT a component of vital capacity (VC)?
What is the difference between pulmonary ventilation and alveolar ventilation?
What is the difference between pulmonary ventilation and alveolar ventilation?
What is the normal value of alveolar ventilation?
What is the normal value of alveolar ventilation?
Which of the following is a factor that affects airway resistance?
Which of the following is a factor that affects airway resistance?
Which part of the brain is responsible for regulating the rate and rhythm of breathing?
Which part of the brain is responsible for regulating the rate and rhythm of breathing?
What is the primary function of the dorsal respiratory group?
What is the primary function of the dorsal respiratory group?
Which of the following is NOT a function of the ventral respiratory group?
Which of the following is NOT a function of the ventral respiratory group?
How does the pneumotaxic center affect breathing?
How does the pneumotaxic center affect breathing?
What is the role of afferent nerves in the regulation of respiration?
What is the role of afferent nerves in the regulation of respiration?
How does the nervous system ensure adequate ventilation during heavy exercise?
How does the nervous system ensure adequate ventilation during heavy exercise?
What is the primary function of efferent nerves in the regulation of respiration?
What is the primary function of efferent nerves in the regulation of respiration?
What is the approximate maximum duration of voluntary apnea?
What is the approximate maximum duration of voluntary apnea?
What is the normal value of tidal volume in mL?
What is the normal value of tidal volume in mL?
Which lung volume represents the additional air that can be forcefully inspired after normal inspiration?
Which lung volume represents the additional air that can be forcefully inspired after normal inspiration?
What is the primary functionality of spirometry in pulmonary function tests?
What is the primary functionality of spirometry in pulmonary function tests?
Which of the following lung capacities includes both tidal volume and inspiratory reserve volume?
Which of the following lung capacities includes both tidal volume and inspiratory reserve volume?
What is the term used for the graphical recording of lung volumes and capacities?
What is the term used for the graphical recording of lung volumes and capacities?
What is the normal value for residual volume in mL?
What is the normal value for residual volume in mL?
Which lung volume can be expired forcefully after normal expiration?
Which lung volume can be expired forcefully after normal expiration?
Lung capacities are defined as:
Lung capacities are defined as:
Which of these is NOT a mechanism proposed to explain the link between oral health and respiratory infections?
Which of these is NOT a mechanism proposed to explain the link between oral health and respiratory infections?
What is a key factor in the potential link between periodontal disease and respiratory infections?
What is a key factor in the potential link between periodontal disease and respiratory infections?
How do salivary enzymes potentially contribute to respiratory infections?
How do salivary enzymes potentially contribute to respiratory infections?
What is the role of hydrolytic enzymes from periodontal bacteria in the context of respiratory infections?
What is the role of hydrolytic enzymes from periodontal bacteria in the context of respiratory infections?
What role do cytokines play in the potential link between periodontal disease and respiratory infections?
What role do cytokines play in the potential link between periodontal disease and respiratory infections?
Why is the link between poor oral hygiene and respiratory disease considered plausible?
Why is the link between poor oral hygiene and respiratory disease considered plausible?
Flashcards are hidden until you start studying
Study Notes
Pulmonary Function Tests
- Pulmonary function tests assess the functional status of the respiratory system by measuring lung volumes and capacities.
- These tests involve recording the volume movement of air into and out of the lungs using a method called spirometry.
- The graphical recording of lung volumes and capacities is called a spirogram.
Spirometer
- A spirometer measures lung volumes and capacities by recording the volume of air breathed in and out of the lungs.
- During expiration, the air enters the spirometer from the lungs, and the pen draws a downward curve on the recording drum.
Lung Volumes
- Lung volumes are the static volumes of air breathed by an individual and are classified into four types:
- Tidal volume (TV): the volume of air breathed in and out of the lungs in a single normal quiet respiration (normal value = 500 mL or 0.5 L)
- Inspiratory reserve volume (IRV): the additional volume of air that can be inspired forcefully after the end of normal inspiration (normal value = 3300 mL or 3.3 L)
- Expiratory reserve volume (ERV): the additional volume of air that can be expired out forcefully after normal expiration (normal value = 1000 mL or 1 L)
- Residual volume (RV): the volume of air remaining in the lungs even after forced expiration (normal value = 1200 mL or 1.2 L)
Lung Capacities
- Lung capacities are the combination of two or more lung volumes and are classified into four types:
- Inspiratory capacity (IC): the maximum volume of air that is inspired after normal expiration (IC = TV + IRV = 500 + 3300 = 3800 mL)
- Vital capacity (VC): the maximum volume of air that can be expelled out forcefully after a deep (maximal) inspiration (VC = IRV + TV + ERV = 3300 + 500 + 1000 = 4800 mL)
- Functional residual capacity (FRC): the volume of air remaining in the lungs after normal expiration (FRC = ERV + RV = 1000 + 1200 = 2200 mL)
- Total lung capacity (TLC): the volume of air present in the lungs after a deep (maximal) inspiration (TLC = IRV + TV + ERV + RV = 3300 + 500 + 1000 + 1200 = 6000 mL)
Pulmonary Ventilation
- Pulmonary ventilation is the volume of air moving in and out of the lungs per minute in quiet breathing (normal value = 6 L/minute).
- It is calculated by the formula: Pulmonary ventilation = Tidal volume × Respiratory rate = 500 mL × 12/minute = 6,000 mL = 6 L/minute
Alveolar Ventilation
- Alveolar ventilation is the amount of air utilized for gaseous exchange every minute (normal value = 4,200 mL or 4.2 L/minute).
- It is different from pulmonary ventilation, as only a portion of the pulmonary ventilation is utilized for gaseous exchange.
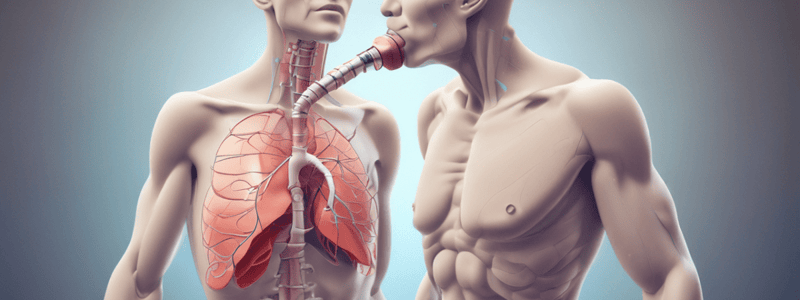
Regulation of Respiration
- Respiration is a reflex process that can be controlled voluntarily.
- The nervous mechanism regulates respiration through the respiratory centers, afferent nerves, and efferent nerves.
- The respiratory center is composed of three major collections of neurons:
- Dorsal respiratory group: causes inspiration
- Ventral respiratory group: causes expiration
- Pneumotaxic center: controls rate and depth of breathing
Chemical Mechanism
- The chemical mechanism regulates respiration through chemoreceptors, which respond to changes in blood pH, PCO2, and PO2.
- Chemoreceptors are classified into two groups:
- Central chemoreceptors: respond to changes in blood pH and are located in the brain
- Peripheral chemoreceptors: respond to changes in PO2 and PCO2 and are located in the carotid and aortic regions
Oral Health and Respiratory Disease
- There is a possible association between oral health and respiratory disease.
- Oral bacteria, especially periodontal pathogens, have been implicated as important agents in causing respiratory diseases.
- Four possible mechanisms explain the biological plausibility of this association:
- Oral pathogens directly aspirated into the lungs
- Salivary enzymes associated with periodontal disease modify respiratory tract mucosal surfaces and promote adhesion and colonization by respiratory pathogens
- Hydrolytic enzymes from periodonto-pathic bacteria may destroy the salivary film that protects against pathogenic bacteria
- The presence of cytokines and other biologically active molecules released from periodontal tissues and peripheral mononuclear cells may alter the respiratory epithelium and promote colonization by respiratory pathogens
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.