Podcast
Questions and Answers
What is the primary function of the alveoli in the respiratory system?
What is the primary function of the alveoli in the respiratory system?
- To facilitate the exchange of O2 and CO2 (correct)
- To humidify the inspired air
- To filter particulate material from inspired air
- To provide structural support to bronchial tubes
Which component is NOT part of the conducting portion of the respiratory system?
Which component is NOT part of the conducting portion of the respiratory system?
- Bronchioles
- Alveolar ducts (correct)
- Trachea
- Nasal cavities
Which structure helps move air through the lungs during ventilation?
Which structure helps move air through the lungs during ventilation?
- Bronchioles
- Alveoli
- Olfactory epithelium
- Diaphragm (correct)
What are the two anatomical divisions of the respiratory system?
What are the two anatomical divisions of the respiratory system?
What type of epithelial tissue lines the nasal cavities?
What type of epithelial tissue lines the nasal cavities?
What role does the conducting portion of the respiratory system play?
What role does the conducting portion of the respiratory system play?
Which structures provide rigid support and flexibility to the conducting portion of the respiratory system?
Which structures provide rigid support and flexibility to the conducting portion of the respiratory system?
Which of the following is NOT a component of the respiratory portion of the respiratory system?
Which of the following is NOT a component of the respiratory portion of the respiratory system?
What type of epithelium covers the upper surface of the epiglottis?
What type of epithelium covers the upper surface of the epiglottis?
Which structure plays a key role in preventing swallowed food from entering the airway?
Which structure plays a key role in preventing swallowed food from entering the airway?
What type of cartilage reinforces the wall of the larynx?
What type of cartilage reinforces the wall of the larynx?
What is the primary role of the vocal folds during phonation?
What is the primary role of the vocal folds during phonation?
Which is NOT a component that contributes to the resonance of sounds produced in the larynx?
Which is NOT a component that contributes to the resonance of sounds produced in the larynx?
Which type of connective tissue is found supporting the vocal folds?
Which type of connective tissue is found supporting the vocal folds?
What is primarily caused by rapid air movement through the vocal cords?
What is primarily caused by rapid air movement through the vocal cords?
Which type of glands are found beneath the epithelium of the vocal folds?
Which type of glands are found beneath the epithelium of the vocal folds?
Which feature is common between the vestibular folds and the vocal folds?
Which feature is common between the vestibular folds and the vocal folds?
How does the male larynx differ from the female larynx after puberty?
How does the male larynx differ from the female larynx after puberty?
What is the primary reflex action associated with irritation of the trachea?
What is the primary reflex action associated with irritation of the trachea?
What happens to the vocal folds during laryngitis?
What happens to the vocal folds during laryngitis?
What type of cartilage is found in the epiglottis?
What type of cartilage is found in the epiglottis?
What is the main function of the olfactory glands (of Bowman) in the olfactory epithelium?
What is the main function of the olfactory glands (of Bowman) in the olfactory epithelium?
Which type of epithelium lines the nasopharynx?
Which type of epithelium lines the nasopharynx?
What is a potential consequence of head trauma to the ethmoid bone?
What is a potential consequence of head trauma to the ethmoid bone?
Which of the following structures is NOT found in the nasopharynx?
Which of the following structures is NOT found in the nasopharynx?
Which cell type is most abundant in the respiratory epithelium?
Which cell type is most abundant in the respiratory epithelium?
What characteristic distinguishes the respiratory epithelium from the olfactory epithelium?
What characteristic distinguishes the respiratory epithelium from the olfactory epithelium?
What is the primary role of ciliary movements in the respiratory tract?
What is the primary role of ciliary movements in the respiratory tract?
Which structure communicates with the nasal cavities through small openings?
Which structure communicates with the nasal cavities through small openings?
Which condition is characterized by an inflammatory process of the sinuses?
Which condition is characterized by an inflammatory process of the sinuses?
What type of cells account for approximately 30% of the respiratory epithelium?
What type of cells account for approximately 30% of the respiratory epithelium?
What type of epithelium lines the laryngopharynx?
What type of epithelium lines the laryngopharynx?
Which of the following is a characteristic feature of brush cells in the respiratory epithelium?
Which of the following is a characteristic feature of brush cells in the respiratory epithelium?
What effect does chronic sinusitis have in the context of primary ciliary dyskinesia?
What effect does chronic sinusitis have in the context of primary ciliary dyskinesia?
What are singer’s nodules?
What are singer’s nodules?
What structure helps maintain the tracheal lumen open?
What structure helps maintain the tracheal lumen open?
What is the primary role of the trachealis muscle?
What is the primary role of the trachealis muscle?
What do the tertiary bronchi give rise to?
What do the tertiary bronchi give rise to?
How does the respiratory portion of the bronchi change as they become smaller?
How does the respiratory portion of the bronchi change as they become smaller?
Which type of epithelium lines the larger bronchi?
Which type of epithelium lines the larger bronchi?
What is the function of the crisscrossing bundles of smooth muscle in the bronchi?
What is the function of the crisscrossing bundles of smooth muscle in the bronchi?
What characterizes the terminal branches of the bronchi?
What characterizes the terminal branches of the bronchi?
What is a significant feature of the bronchial tree related to lung surgery?
What is a significant feature of the bronchial tree related to lung surgery?
What role do seromucous glands in the trachea primarily serve?
What role do seromucous glands in the trachea primarily serve?
What common respiratory diseases are associated with inhaled pathogens?
What common respiratory diseases are associated with inhaled pathogens?
What anatomical feature is unique to the trachea compared to other bronchial structures?
What anatomical feature is unique to the trachea compared to other bronchial structures?
How do the open ends of the tracheal cartilage rings positioned?
How do the open ends of the tracheal cartilage rings positioned?
Which histological organization change occurs as bronchi become smaller?
Which histological organization change occurs as bronchi become smaller?
What is the primary role of the mucosa in the nasal cavities?
What is the primary role of the mucosa in the nasal cavities?
Which type of epithelium covers the upper portion of the nasal cavity?
Which type of epithelium covers the upper portion of the nasal cavity?
What type of cells in the respiratory epithelium are responsible for mucus production?
What type of cells in the respiratory epithelium are responsible for mucus production?
Which of the following statements about the chronic effects of smoking on the nasal epithelium is true?
Which of the following statements about the chronic effects of smoking on the nasal epithelium is true?
How often are olfactory neurons replaced in the olfactory epithelium?
How often are olfactory neurons replaced in the olfactory epithelium?
What is the primary function of the supporting cells in the olfactory epithelium?
What is the primary function of the supporting cells in the olfactory epithelium?
What structures help to warm and humidify inhaled air within the nasal cavities?
What structures help to warm and humidify inhaled air within the nasal cavities?
What is the consequence of immobilized cilia in the respiratory epithelium?
What is the consequence of immobilized cilia in the respiratory epithelium?
What role do small granule cells play in the respiratory epithelium?
What role do small granule cells play in the respiratory epithelium?
Where do the axons from olfactory neurons pass after leaving the olfactory epithelium?
Where do the axons from olfactory neurons pass after leaving the olfactory epithelium?
Which of the following cell types have a limited regenerative capability in the olfactory epithelium?
Which of the following cell types have a limited regenerative capability in the olfactory epithelium?
What type of epithelium is found in the conducting portion of the respiratory system?
What type of epithelium is found in the conducting portion of the respiratory system?
The lamina propria in the nasal cavity mucosa is important for which function?
The lamina propria in the nasal cavity mucosa is important for which function?
What type of epithelium is present in the larger bronchioles?
What type of epithelium is present in the larger bronchioles?
Which cells are primarily found in the epithelium of respiratory bronchioles?
Which cells are primarily found in the epithelium of respiratory bronchioles?
What induces endocytosis in type II cells during coronavirus infection?
What induces endocytosis in type II cells during coronavirus infection?
What is a consequence of reduced surfactant production in infected cells?
What is a consequence of reduced surfactant production in infected cells?
What pathological condition can result from blockage in the bronchi due to excess mucus?
What pathological condition can result from blockage in the bronchi due to excess mucus?
What major feature distinguishes alveolar ducts from respiratory bronchioles?
What major feature distinguishes alveolar ducts from respiratory bronchioles?
What characteristic distinguishes active alveolar macrophages from type II pneumocytes?
What characteristic distinguishes active alveolar macrophages from type II pneumocytes?
What is the composition of the lamina propria in alveolar ducts?
What is the composition of the lamina propria in alveolar ducts?
Which process removes alveolar lining fluids from the lungs?
Which process removes alveolar lining fluids from the lungs?
Which type of cells help reduce surface tension in the bronchioles?
Which type of cells help reduce surface tension in the bronchioles?
What is the fate of most filled macrophages in the lungs?
What is the fate of most filled macrophages in the lungs?
Where are the capillaries predominantly located in relation to the alveoli?
Where are the capillaries predominantly located in relation to the alveoli?
Which agents are contained in bronchoalveolar fluid that contribute to its bacteriostatic properties?
Which agents are contained in bronchoalveolar fluid that contribute to its bacteriostatic properties?
What can persistent blockage in the bronchi lead to, aside from atelectasis?
What can persistent blockage in the bronchi lead to, aside from atelectasis?
What pathological change occurs due to infection in the lungs?
What pathological change occurs due to infection in the lungs?
What cells give rise to all cells within the bronchiolar epithelium?
What cells give rise to all cells within the bronchiolar epithelium?
In congestive heart failure, which specific cells are identified in the lung and sputum due to the presence of hemosiderin?
In congestive heart failure, which specific cells are identified in the lung and sputum due to the presence of hemosiderin?
Which of the following features is characteristic of very small bronchioles?
Which of the following features is characteristic of very small bronchioles?
What is the role of the fibroblasts seen in the interalveolar septum?
What is the role of the fibroblasts seen in the interalveolar septum?
What type of cells produce the pulmonary surfactant that lines the alveoli?
What type of cells produce the pulmonary surfactant that lines the alveoli?
What is the primary function of club cells in the bronchioles?
What is the primary function of club cells in the bronchioles?
What changes occur in the alveolar structure as one proceeds distally along the respiratory bronchioles?
What changes occur in the alveolar structure as one proceeds distally along the respiratory bronchioles?
Which type of epithelium is featured in terminal bronchioles?
Which type of epithelium is featured in terminal bronchioles?
What is the effect of elastic fibers in the bronchiole walls?
What is the effect of elastic fibers in the bronchiole walls?
What is the primary role of the smooth muscle in bronchioles?
What is the primary role of the smooth muscle in bronchioles?
Which type of cells predominantly line the terminal bronchioles?
Which type of cells predominantly line the terminal bronchioles?
What is a major consequence of bronchiolitis in young children?
What is a major consequence of bronchiolitis in young children?
What functions are performed by club cells in the terminal bronchioles?
What functions are performed by club cells in the terminal bronchioles?
Which structure does NOT have cartilage present?
Which structure does NOT have cartilage present?
What happens to the epithelial lining height as the bronchial tree branches further?
What happens to the epithelial lining height as the bronchial tree branches further?
In which locations does gas exchange primarily take place?
In which locations does gas exchange primarily take place?
What is indicated by the term 'mucociliary apparatus'?
What is indicated by the term 'mucociliary apparatus'?
Which type of viral infection is often associated with bronchiolitis in children?
Which type of viral infection is often associated with bronchiolitis in children?
How does the muscle layer in bronchi compare to that of bronchioles?
How does the muscle layer in bronchi compare to that of bronchioles?
Which type of alveolar cells are responsible for producing surfactant?
Which type of alveolar cells are responsible for producing surfactant?
What influence does the autonomic nervous system have on bronchi and bronchioles?
What influence does the autonomic nervous system have on bronchi and bronchioles?
What is the effect of asthma on the bronchial tree?
What is the effect of asthma on the bronchial tree?
What structures are present in bronchi but not in bronchioles?
What structures are present in bronchi but not in bronchioles?
What are the primary functions of the alveoli in the lungs?
What are the primary functions of the alveoli in the lungs?
What role do elastic and reticular fibers play in the alveoli?
What role do elastic and reticular fibers play in the alveoli?
What primarily separates alveolar air from capillary blood?
What primarily separates alveolar air from capillary blood?
How does oxygen get from the alveoli into the blood?
How does oxygen get from the alveoli into the blood?
Which component of alveolar structure is crucial for equalizing air pressure in adjacent alveoli?
Which component of alveolar structure is crucial for equalizing air pressure in adjacent alveoli?
What type of cells line the alveoli, contributing to the respiratory membrane?
What type of cells line the alveoli, contributing to the respiratory membrane?
What occurs to most carbon dioxide as it travels in the bloodstream to the lungs?
What occurs to most carbon dioxide as it travels in the bloodstream to the lungs?
How does the structure of alveolar walls enhance gas exchange?
How does the structure of alveolar walls enhance gas exchange?
What is the primary role of macrophages located within the interalveolar septa?
What is the primary role of macrophages located within the interalveolar septa?
Which of the following structures directly branches from terminal bronchioles?
Which of the following structures directly branches from terminal bronchioles?
What is the significance of the capillary networks surrounding alveoli?
What is the significance of the capillary networks surrounding alveoli?
What is the diameter range of alveolar pores?
What is the diameter range of alveolar pores?
In which aspect do respiratory bronchioles differ from terminal bronchioles?
In which aspect do respiratory bronchioles differ from terminal bronchioles?
How does the arrangement of anatomical structures in the alveoli contribute to lung function?
How does the arrangement of anatomical structures in the alveoli contribute to lung function?
What is the primary function of type I alveolar cells?
What is the primary function of type I alveolar cells?
What constitutes the majority of the alveolar lining?
What constitutes the majority of the alveolar lining?
What is the primary role of lamellar bodies in type II alveolar cells?
What is the primary role of lamellar bodies in type II alveolar cells?
How do type II alveolar cells contribute to lung function?
How do type II alveolar cells contribute to lung function?
What type of junctions do type I alveolar cells have to prevent leakage of fluids?
What type of junctions do type I alveolar cells have to prevent leakage of fluids?
What happens to surfactant during fetal development?
What happens to surfactant during fetal development?
Which component is critical for the proper orientation of DPPC in the surfactant film?
Which component is critical for the proper orientation of DPPC in the surfactant film?
What major problem occurs in premature neonates related to surfactant?
What major problem occurs in premature neonates related to surfactant?
What type of cells primarily line the alveolar surfaces?
What type of cells primarily line the alveolar surfaces?
Which surfactant proteins are important for innate immune protection?
Which surfactant proteins are important for innate immune protection?
How does the surfactant layer affect alveoli functionality?
How does the surfactant layer affect alveoli functionality?
Which of the following is a role of pinocytotic vesicles in type I alveolar cells?
Which of the following is a role of pinocytotic vesicles in type I alveolar cells?
What is the effect of surfactant on lung mechanics?
What is the effect of surfactant on lung mechanics?
Which of the following statements is true about type II alveolar cells?
Which of the following statements is true about type II alveolar cells?
Flashcards
Respiratory System
Respiratory System
The system responsible for gas exchange between the body and the environment, allowing for the intake of oxygen and the expulsion of carbon dioxide.
Conducting Portion
Conducting Portion
The network of tubes that carry air from the nose and mouth to the lungs.
Respiratory Portion
Respiratory Portion
The area in the lungs where gas exchange occurs, involving the transfer of oxygen into the bloodstream and carbon dioxide out.
Alveoli
Alveoli
Signup and view all the flashcards
Ventilation
Ventilation
Signup and view all the flashcards
Vestibule
Vestibule
Signup and view all the flashcards
Pseudostratified Columnar Epithelium
Pseudostratified Columnar Epithelium
Signup and view all the flashcards
Olfactory Epithelium
Olfactory Epithelium
Signup and view all the flashcards
Nasal Cavities
Nasal Cavities
Signup and view all the flashcards
Conchae (Turbinate Bones)
Conchae (Turbinate Bones)
Signup and view all the flashcards
Nasal Mucosa
Nasal Mucosa
Signup and view all the flashcards
Nasal Mucosa Vasculature
Nasal Mucosa Vasculature
Signup and view all the flashcards
Mucus
Mucus
Signup and view all the flashcards
Immunoglobulin A (IgA)
Immunoglobulin A (IgA)
Signup and view all the flashcards
Olfactory Neurons
Olfactory Neurons
Signup and view all the flashcards
Olfactory Neuron Dendrite
Olfactory Neuron Dendrite
Signup and view all the flashcards
Olfactory Cilia
Olfactory Cilia
Signup and view all the flashcards
Olfactory Axons
Olfactory Axons
Signup and view all the flashcards
Supporting Cells
Supporting Cells
Signup and view all the flashcards
Basal Cells
Basal Cells
Signup and view all the flashcards
Respiratory Epithelium
Respiratory Epithelium
Signup and view all the flashcards
Goblet Cells
Goblet Cells
Signup and view all the flashcards
Paranasal Sinuses
Paranasal Sinuses
Signup and view all the flashcards
Olfactory Glands (of Bowman)
Olfactory Glands (of Bowman)
Signup and view all the flashcards
Cilia
Cilia
Signup and view all the flashcards
Nasopharynx
Nasopharynx
Signup and view all the flashcards
Oropharynx
Oropharynx
Signup and view all the flashcards
Laryngopharynx
Laryngopharynx
Signup and view all the flashcards
Larynx
Larynx
Signup and view all the flashcards
Primary Ciliary Dyskinesia (Kartagener Syndrome)
Primary Ciliary Dyskinesia (Kartagener Syndrome)
Signup and view all the flashcards
Sinusitis
Sinusitis
Signup and view all the flashcards
Olfaction
Olfaction
Signup and view all the flashcards
Hyposmia
Hyposmia
Signup and view all the flashcards
Anosmia
Anosmia
Signup and view all the flashcards
What is the larynx and what is it specialized for?
What is the larynx and what is it specialized for?
Signup and view all the flashcards
Name the major cartilages of the larynx.
Name the major cartilages of the larynx.
Signup and view all the flashcards
What does the epiglottis do?
What does the epiglottis do?
Signup and view all the flashcards
Describe the lining of the larynx.
Describe the lining of the larynx.
Signup and view all the flashcards
What are the vocal folds?
What are the vocal folds?
Signup and view all the flashcards
How does the larynx produce sound?
How does the larynx produce sound?
Signup and view all the flashcards
What is the trachea and what is it made of?
What is the trachea and what is it made of?
Signup and view all the flashcards
What is the lining of the trachea?
What is the lining of the trachea?
Signup and view all the flashcards
Describe the branching of the bronchi.
Describe the branching of the bronchi.
Signup and view all the flashcards
What are bronchioles and what do they lead to?
What are bronchioles and what do they lead to?
Signup and view all the flashcards
What is laryngitis?
What is laryngitis?
Signup and view all the flashcards
What is croup?
What is croup?
Signup and view all the flashcards
What is a cough?
What is a cough?
Signup and view all the flashcards
What are cough suppressants?
What are cough suppressants?
Signup and view all the flashcards
What are expectorants?
What are expectorants?
Signup and view all the flashcards
What are Singer's Nodules?
What are Singer's Nodules?
Signup and view all the flashcards
What is the Trachea?
What is the Trachea?
Signup and view all the flashcards
What is Respiratory Mucosa?
What is Respiratory Mucosa?
Signup and view all the flashcards
What are the C-shaped rings of cartilage in the trachea?
What are the C-shaped rings of cartilage in the trachea?
Signup and view all the flashcards
What lies at the open ends of the C-shaped cartilaginous rings in the trachea?
What lies at the open ends of the C-shaped cartilaginous rings in the trachea?
Signup and view all the flashcards
What is the function of the trachealis muscle during swallowing?
What is the function of the trachealis muscle during swallowing?
Signup and view all the flashcards
What is the function of the trachealis muscle during coughing?
What is the function of the trachealis muscle during coughing?
Signup and view all the flashcards
What are bronchopulmonary segments?
What are bronchopulmonary segments?
Signup and view all the flashcards
Why are bronchopulmonary segments important for surgery?
Why are bronchopulmonary segments important for surgery?
Signup and view all the flashcards
What are bronchioles?
What are bronchioles?
Signup and view all the flashcards
What is a pulmonary lobule?
What is a pulmonary lobule?
Signup and view all the flashcards
Why are the lungs susceptible to infections?
Why are the lungs susceptible to infections?
Signup and view all the flashcards
How does the structure of the bronchial tree change from larger to smaller branches?
How does the structure of the bronchial tree change from larger to smaller branches?
Signup and view all the flashcards
How does the cartilage support change in the bronchial tree?
How does the cartilage support change in the bronchial tree?
Signup and view all the flashcards
What is present in the lamina propria of bronchi?
What is present in the lamina propria of bronchi?
Signup and view all the flashcards
Terminal Bronchioles
Terminal Bronchioles
Signup and view all the flashcards
Club Cells
Club Cells
Signup and view all the flashcards
Bronchoconstriction and Bronchodilation
Bronchoconstriction and Bronchodilation
Signup and view all the flashcards
Asthma
Asthma
Signup and view all the flashcards
Mucociliary Escalator
Mucociliary Escalator
Signup and view all the flashcards
Alveolar Cells (Pneumocytes)
Alveolar Cells (Pneumocytes)
Signup and view all the flashcards
Surfactant
Surfactant
Signup and view all the flashcards
Bronchospasm
Bronchospasm
Signup and view all the flashcards
Bronchiolitis
Bronchiolitis
Signup and view all the flashcards
Bronchi
Bronchi
Signup and view all the flashcards
Bronchiolar Lamina Propria
Bronchiolar Lamina Propria
Signup and view all the flashcards
Respiratory Bronchiole
Respiratory Bronchiole
Signup and view all the flashcards
Atelectasis
Atelectasis
Signup and view all the flashcards
Diffuse Alveolar Damage (Adult Respiratory Distress Syndrome)
Diffuse Alveolar Damage (Adult Respiratory Distress Syndrome)
Signup and view all the flashcards
Alveolar Ducts
Alveolar Ducts
Signup and view all the flashcards
Alveolar Sacs
Alveolar Sacs
Signup and view all the flashcards
Lamina Propria (of Alveoli)
Lamina Propria (of Alveoli)
Signup and view all the flashcards
Tracheal Cartilage
Tracheal Cartilage
Signup and view all the flashcards
Trachealis Muscle
Trachealis Muscle
Signup and view all the flashcards
Tracheal Mucosa
Tracheal Mucosa
Signup and view all the flashcards
Simple Squamous Epithelium
Simple Squamous Epithelium
Signup and view all the flashcards
Tracheal Submucosa
Tracheal Submucosa
Signup and view all the flashcards
Alveolar Pores (of Kohn)
Alveolar Pores (of Kohn)
Signup and view all the flashcards
Respiratory Membrane (Blood-Air Barrier)
Respiratory Membrane (Blood-Air Barrier)
Signup and view all the flashcards
Bronchial Tree
Bronchial Tree
Signup and view all the flashcards
Bronchioles
Bronchioles
Signup and view all the flashcards
Alveolar Wall
Alveolar Wall
Signup and view all the flashcards
Alveolar lining cells
Alveolar lining cells
Signup and view all the flashcards
Pulmonary Capillaries
Pulmonary Capillaries
Signup and view all the flashcards
Lung Parenchyma
Lung Parenchyma
Signup and view all the flashcards
Gas Exchange
Gas Exchange
Signup and view all the flashcards
Bronchial Vessels
Bronchial Vessels
Signup and view all the flashcards
Partial Pressure Gradient
Partial Pressure Gradient
Signup and view all the flashcards
Type I Alveolar Cells
Type I Alveolar Cells
Signup and view all the flashcards
Type II Alveolar Cells
Type II Alveolar Cells
Signup and view all the flashcards
Pulmonary Surfactant
Pulmonary Surfactant
Signup and view all the flashcards
Dipalmitoylphosphatidylcholine (DPPC)
Dipalmitoylphosphatidylcholine (DPPC)
Signup and view all the flashcards
Surfactant Proteins (SP-A, SP-B, SP-C, SP-D)
Surfactant Proteins (SP-A, SP-B, SP-C, SP-D)
Signup and view all the flashcards
Surfactant Turnover
Surfactant Turnover
Signup and view all the flashcards
Respiratory Distress Syndrome (RDS)
Respiratory Distress Syndrome (RDS)
Signup and view all the flashcards
Blood-Air Barrier
Blood-Air Barrier
Signup and view all the flashcards
Alveolar Macrophages (Dust Cells)
Alveolar Macrophages (Dust Cells)
Signup and view all the flashcards
Angiotensin-Converting Enzyme 2 (ACE2)
Angiotensin-Converting Enzyme 2 (ACE2)
Signup and view all the flashcards
Type II Pneumocytes
Type II Pneumocytes
Signup and view all the flashcards
How does Coronavirus enter a cell?
How does Coronavirus enter a cell?
Signup and view all the flashcards
What effect does coronavirus have on lung function?
What effect does coronavirus have on lung function?
Signup and view all the flashcards
What are alveolar macrophages and their function?
What are alveolar macrophages and their function?
Signup and view all the flashcards
How can you distinguish alveolar macrophages from type II pneumocytes?
How can you distinguish alveolar macrophages from type II pneumocytes?
Signup and view all the flashcards
What happens to filled alveolar macrophages?
What happens to filled alveolar macrophages?
Signup and view all the flashcards
How are alveolar lining fluids removed?
How are alveolar lining fluids removed?
Signup and view all the flashcards
What are some properties of bronchoalveolar fluid?
What are some properties of bronchoalveolar fluid?
Signup and view all the flashcards
What are heart failure cells?
What are heart failure cells?
Signup and view all the flashcards
What is the role of type II alveolar cells?
What is the role of type II alveolar cells?
Signup and view all the flashcards
Study Notes
Respiratory System Overview
- The respiratory system facilitates gas exchange (O2 and CO2) between blood and the environment.
- It comprises the lungs and bronchial tubes connecting exchange sites to the outside.
- Ventilation moves air through the lungs, using the thoracic cage, intercostal muscles, diaphragm, and lung tissue elasticity.
Anatomical Divisions
- The respiratory system is divided into upper and lower tracts. (Image shown as Figure 17-1)
- The conducting portion prepares inhaled air (cleans, humidifies), transporting it to alveoli.
- The respiratory portion carries out gas exchange, involving respiratory bronchioles, alveolar ducts, and alveoli.
Alveoli
- Alveoli are tiny air sacs responsible for oxygen and carbon dioxide exchange with the blood.
- They are the major component of lung structure.
Nasal Cavities
- The nasal cavities are divided into a vestibule and internal cavity.
- Coarse hairs, sweat glands, and sebaceous glands in the vestibule filter inhaled air.
- The internal structure features bony projections called conchae, with moist mucous membranes lining the surfaces.
- The vasculature warms and humidifies incoming air while trapping foreign particles.
- Secretions trap and remove inhaled particles and microorganisms (immunoglobulin A [IgA] is a critical component).
- Part of one type of nasal epithelium (olfactory epithelium) is specialized for smell.
Respiratory Epithelium
- Ciliated pseudostratified columnar epithelium lines most of the conducting portion.
- It has several cell types: cilia (sweep mucus), goblet cells (secrete mucus), brush cells (chemosensors), and small granule cells (part of a system for neuroendocrine control).
- Basal cells are stem cells, replacing damaged cells.
- Toxins (like in smoking) can negatively impact the epithelium, leading to cilia immobilization and a chance of cancerous changes.
Olfactory Epithelium
- Located in the superior conchae.
- Contains olfactory receptor neurons detecting odors.
- Olfactory cilia amplify sensory area of olfactory cells and are crucial for odor detection.
- Supporting cells maintain olfactory environment.
- Basal cells are progenitor cells, replacing olfactory cells.
Paranasal Sinuses
- Air-filled cavities in skull bones (frontal, maxillary, ethmoid, sphenoid).
- They have a thinner respiratory epithelium than nasal cavities, with fewer goblet cells.
Pharynx
- It's a passageway from nasal cavities to larynx and esophagus.
- Different sections of the pharynx have differing types of linings suited to their functions.
Larynx
- Connects pharynx with trachea, serving as airflow passage; vital for speech.
- The larynx's walls include hyaline and elastic cartilages, providing structure and flexibility during phonation.
- Vocal folds and vestibular folds enable vocalization.
- The epiglottis's primary function is food and fluid blockage from entrance into respiratory passages.
Trachea
- The trachea is about 10-12 cm long.
- Its walls are supported by C-shaped hyaline cartilage rings.
- Smooth trachealis muscle relaxes during swallowing to prevent obstruction of both esophagus and trachea.
Bronchial Tree & Lungs
- Trachea divides into primary bronchi entering the lungs at the hilum.
- They further branch into smaller bronchi, bronchioles, and finally terminal bronchioles in the pulmonary lobules.
- Histological features simplify as airways narrow.
- Bronchioles lack cartilage, contain more smooth muscle contributing to bronchoconstriction and bronchodilation, and are lined with club cells.
Respiratory Bronchioles
- Respiratory bronchioles are the first part of the respiratory portion, having alveolar openings.
- The lining includes club cells, simple squamous cells, and smooth muscle.
Alveolar Ducts and Alveolar Sacs
- Alveolar ducts connect respiratory bronchioles with alveolar sacs (clusters of alveoli).
- Alveolar walls are extremely thin, enabling efficient gas exchange.
- The walls contain elastic fibers enabling expansion during inhalation and passive recoil in exhalation.
- Pulmonary capillaries are concentrated around alveoli.
Alveoli
- Alveoli are the primary sites of gas exchange in lungs.
- An adult human has approximately 200 million alveoli.
- Alveoli have extremely thin walls, surrounded by rich capillary networks.
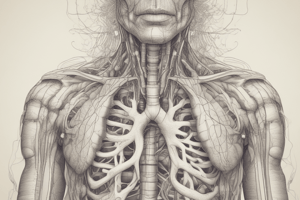
Respiratory Membrane
- The respiratory membrane facilitates gas exchange between air and blood.
- Three layers form the respiratory membrane: alveolar cells, fused basal laminae, and capillary endothelial cells.
Type I and Type II Alveolar Cells
- Type I alveolar cells are exceptionally thin, maximizing gas exchange.
- Type II alveolar cells produce surfactant, a crucial substance lowering surface tension in the alveoli.
- Premature infants often have difficulties as their surfactant production is still developing.
Alveolar Macrophages
- Macrophages (dust cells) remove foreign particles and debris from alveoli.
Other Points
- The system is highly susceptible to inhaled pathogens causing respiratory diseases.
- Chronic conditions like sinusitis, asthma, and bronchitis can result from various factors, such as infections, inflammation, allergies, or mucus buildup.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.
Description
Test your knowledge about the respiratory system, its anatomical divisions, and the role of alveoli in gas exchange. This quiz covers essential concepts including ventilation and the structure of nasal cavities. Perfect for students studying biology or health sciences.