Podcast
Questions and Answers
What is the normal pH range for the human body?
What is the normal pH range for the human body?
- 7.35 to 7.45 (correct)
- 7.0 to 7.5
- 8.0 to 8.5
- 6.5 to 7.0
How does aging affect the alveoli in the lungs?
How does aging affect the alveoli in the lungs?
- Deteriorates the walls, reducing capacity (correct)
- Maintains their elasticity
- Strengthens the alveolar walls
- Increases their size significantly
What is the effectiveness of respiratory compensation?
What is the effectiveness of respiratory compensation?
- 90%
- 75% (correct)
- 50%
- 100%
Which of the following factors is NOT associated with aging in the respiratory system?
Which of the following factors is NOT associated with aging in the respiratory system?
Which condition is likely to be more common in elderly individuals due to the effects of aging on the respiratory system?
Which condition is likely to be more common in elderly individuals due to the effects of aging on the respiratory system?
How does intrapleural pressure behave during inhalation?
How does intrapleural pressure behave during inhalation?
What role do the diaphragm and external intercostal muscles play during inhalation?
What role do the diaphragm and external intercostal muscles play during inhalation?
What triggers forced exhalation?
What triggers forced exhalation?
What is the primary function of the chemoreceptors in the respiratory system?
What is the primary function of the chemoreceptors in the respiratory system?
Which pulmonary volume refers to the maximum amount of air expelled after a forceful exhalation?
Which pulmonary volume refers to the maximum amount of air expelled after a forceful exhalation?
What occurs during external respiration?
What occurs during external respiration?
What is the primary consequence of decreased respiratory rate in respiratory acidosis?
What is the primary consequence of decreased respiratory rate in respiratory acidosis?
Which center of the brain is responsible for automatically generating impulses for inhalation?
Which center of the brain is responsible for automatically generating impulses for inhalation?
What is the primary regulatory factor for respiration in healthy individuals?
What is the primary regulatory factor for respiration in healthy individuals?
What is the role of the pons in respiration?
What is the role of the pons in respiration?
What type of breathing is characterized as normally a passive process?
What type of breathing is characterized as normally a passive process?
How does the hypothalamus influence the respiratory rate?
How does the hypothalamus influence the respiratory rate?
What describes the relationship between residual air and vital capacity?
What describes the relationship between residual air and vital capacity?
What role do the intercostal muscles play in the process of inhalation?
What role do the intercostal muscles play in the process of inhalation?
Which statement accurately describes intrapulmonic pressure during the inhalation process?
Which statement accurately describes intrapulmonic pressure during the inhalation process?
What is the primary reason why exhalation is considered a passive process?
What is the primary reason why exhalation is considered a passive process?
During forced exhalation, which muscles are primarily responsible for expelling air forcefully from the lungs?
During forced exhalation, which muscles are primarily responsible for expelling air forcefully from the lungs?
What type of receptors play a crucial role in detecting changes in blood gases and influencing respiration?
What type of receptors play a crucial role in detecting changes in blood gases and influencing respiration?
What happens to intrapleural pressure during inhalation compared to its state at rest?
What happens to intrapleural pressure during inhalation compared to its state at rest?
Which pulmonary volume refers to the total amount of air exhaled after the deepest possible inhalation?
Which pulmonary volume refers to the total amount of air exhaled after the deepest possible inhalation?
How does the hypothalamus affect breathing during times of emotional stress?
How does the hypothalamus affect breathing during times of emotional stress?
Which of the following best describes respiratory acidosis?
Which of the following best describes respiratory acidosis?
What is a significant age-related change in the respiratory system regarding lung function?
What is a significant age-related change in the respiratory system regarding lung function?
What is a characteristic feature of internal intercostal muscles during exhalation?
What is a characteristic feature of internal intercostal muscles during exhalation?
How does intrapleural pressure change during inhalation?
How does intrapleural pressure change during inhalation?
In which condition is respiratory compensation likely triggered?
In which condition is respiratory compensation likely triggered?
What is the role of the apneustic center in the brain?
What is the role of the apneustic center in the brain?
Which factor primarily influences the respiratory rate according to blood gas levels?
Which factor primarily influences the respiratory rate according to blood gas levels?
Which pulmonary volume would best represent the air exchanged during vigorous exercise?
Which pulmonary volume would best represent the air exchanged during vigorous exercise?
What condition can arise from aging affecting the respiratory system?
What condition can arise from aging affecting the respiratory system?
What defines the role of the cerebral cortex in respiration?
What defines the role of the cerebral cortex in respiration?
What is the effect of lung elasticity on the process of exhalation?
What is the effect of lung elasticity on the process of exhalation?
What characterizes tidal volume during normal breathing?
What characterizes tidal volume during normal breathing?
Which pressure is always slightly below atmospheric pressure during ventilation?
Which pressure is always slightly below atmospheric pressure during ventilation?
What action primarily occurs during forced exhalation when internal intercostal muscles contract?
What action primarily occurs during forced exhalation when internal intercostal muscles contract?
What describes the main role of the pneumotaxic center in the pons?
What describes the main role of the pneumotaxic center in the pons?
What is the primary effect of hypoxia detected by chemoreceptors?
What is the primary effect of hypoxia detected by chemoreceptors?
Which pulmonary volume can be calculated by multiplying tidal volume by the number of respirations per minute?
Which pulmonary volume can be calculated by multiplying tidal volume by the number of respirations per minute?
What effect does respiratory alkalosis have on the body's carbon dioxide levels?
What effect does respiratory alkalosis have on the body's carbon dioxide levels?
Which structure controls coughing and sneezing actions when stimulated?
Which structure controls coughing and sneezing actions when stimulated?
What is the primary physiological response when the body detects an increase in carbon dioxide levels?
What is the primary physiological response when the body detects an increase in carbon dioxide levels?
In terms of lung mechanics, what primarily drives the movement of air into the lungs during inhalation?
In terms of lung mechanics, what primarily drives the movement of air into the lungs during inhalation?
Flashcards are hidden until you start studying
Study Notes
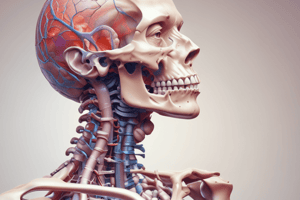
Ventilation
- Movement of air into and out of the alveoli
- Inhalation and exhalation controlled by the nervous system and respiratory muscles - Respiratory centers in the medulla and pons of the brain - Medulla generates impulses to the respiratory muscles
Respiratory Muscles
- Diaphragm: Dome-shaped muscle below the lungs - Contracts and flattens, increasing lung size
- Intercostal muscles: Muscles between ribs
- External intercostal muscles: Pull ribs upward and outward
- Internal intercostal muscles: Pull ribs downward and inward
Pressures During Ventilation
- Atmospheric pressure: Pressure of air surrounding us
- Intrapleural pressure: Pressure within the potential space between the parietal and visceral pleural membranes - Always slightly below atmospheric pressure, referred to as negative pressure
- Intrapulmonic pressure: Pressure within the bronchial tree and alveoli - Fluctuates above and below atmospheric pressure during breathing
Inhalation
- Motor impulses from medulla: Travel to diaphragm and external intercostal muscles
- Diaphragm contracts: Flattens and moves downward, expanding the chest cavity from top to bottom
- External intercostal muscles contract: Pull ribs upward and outward, expanding the chest cavity from side to side and front to back
- Parietal pleura expands: Due to its attachment to the chest wall
- Intrapleural pressure becomes more negative: Creates suction between parietal and visceral pleura
- Visceral pleura expands: Due to its attachment to the parietal pleura and serous fluid
- Lung expansion: Leads to a decrease in intrapulmonic pressure, pulling air into the lungs
- Air continues to enter the lungs until intrapulmonic pressure equals atmospheric pressure
Exhalation
- Diaphragm and external intercostal muscles relax: Chest cavity decreases in size
- Intrapulmonic pressure increases above atmospheric pressure: Air is forced out of the lungs
- Exhalation is normally a passive process: Relies on elasticity of the lungs
- Forced exhalation: Can be achieved by contracting the internal intercostal muscles, which push ribs down and in
Pulmonary Volumes
- Tidal volume: Amount of air involved in one normal inhalation and exhalation (approximately 50 ml)
- Minute respiratory volume: Amount of air inhaled and exhaled in one minute (calculated by multiplying tidal volume by respirations per minute)
- Inspiratory reserve: Amount of air beyond tidal volume that can be taken in with the deepest possible inhalation (2,000-3,000 ml)
- Expiratory reserve: Amount of air beyond tidal volume that can be expelled with the most forceful exhalation (1,000-1,500 ml)
- Vital capacity: Amount of air involved in the deepest inhalation followed by the most forceful exhalation (3,500-5,000 ml)
- Residual air: Amount of air remaining in the lungs after the most forceful exhalation (1,000-1,500 ml)
Respiration
- External respiration: Exchange of gases between the air in the alveoli and blood in the pulmonary capillaries - Oxygen diffuses from alveoli to blood - Carbon dioxide diffuses from blood to alveoli
- Internal respiration: Exchange of gases between the blood in systemic capillaries and the tissues of the body - Oxygen diffuses from blood to tissues - Carbon dioxide diffuses from tissues to blood
Nervous Regulation
- Inspiration center: Automatically generates impulses to stimulate contraction of respiratory muscles, leading to inhalation
- Baroreceptors: Detect lung stretching and send sensory impulses to the medulla, inhibiting the inspiration center
- Expiration center: Activated by the inspiration center during forceful exhalation, sends impulses to internal intercostal and abdominal muscles
Respiratory Centers in the Pons
- Apneustic center: Prolongs inhalation
- Pneumotaxic center: Contributes to exhalation
Hypothalamus and Cerebral Cortex
- Hypothalamus: Modifies breathing rate during emotional stress (e.g., anger, fright)
- Cerebral Cortex: Enables voluntary control of breathing rate and rhythm
Coughing and Sneezing
- Medulla controls both actions:
- Coughing: Stimulated by irritation of the mucosa in the pharynx, larynx, or trachea
- Sneezing: Stimulated by irritation of the nasal mucosa
Chemical Regulation
- Chemoreceptors: Located in the carotid and aortic bodies and medulla, detect changes in blood gases and pH
- Hypoxia: Low oxygen level in blood, detected by chemoreceptors, leading to an increase in respiratory rate
- Excess carbon dioxide (CO2): Lowers blood pH, detected by chemoreceptors, leading to an increase in respiratory rate to exhale CO2
- Carbon dioxide is the major regulator of respiration
Acid-Base Balance
- Respiratory acidosis: Decreased rate or efficiency of respiration, leading to carbon dioxide accumulation in body fluids (e.g., pneumonia, emphysema, asthma)
- Respiratory alkalosis: Increased rate of respiration, leading to rapid carbon dioxide expulsion from the body (e.g., hyperventilation, trauma, anxiety)
- Respiratory compensation: Respiratory center attempts to fix a pH imbalance caused by factors other than the respiratory system (e.g., metabolic acidosis or alkalosis)
- Metabolic acidosis: Caused by factors other than the respiratory system (e.g., diabetes, kidney disease, diarrhea), leading to an increase in hydrogen ions (acid) - Respiratory compensation: Increase in respiratory rate and depth to remove CO2 (acid) and raise pH
- Metabolic alkalosis: Caused by factors other than the respiratory system (e.g., ingestion of alkaline substances, excessive vomiting), leading to a decrease in hydrogen ions (acid) - Respiratory compensation: Decrease in respiratory rate to retain CO2 (acid) and lower pH### pH Scale
- 0 is the most acidic, 14 is the most alkaline, and 7 is neutral
- The normal pH for the human body is 7.35 to 7.45
- There is a small range for normal pH in the body
Respiratory Compensation
- Respiratory compensation is only about 75% effective
Aging and Respiratory System
- Respiratory muscles weaken with age
- Lung tissue and alveoli lose elasticity
- The walls of the alveoli deteriorate, leading to a smaller remaining capacity
- Cilia deteriorate with age
- Macrophages become less efficient, increasing risk of pneumonia
- Chronic diseases such as emphysema and bronchitis are more common in the elderly
- Pulmonary hypertension can result from aging, leading to an overworked right ventricle
- Hypertension can lead to an overworked left ventricle and heart failure
- Pulmonary edema can also occur with aging
### Ventilation
- Movement of air in and out of the lungs, controlled by the nervous system and respiratory muscles.
- The respiratory centers in the medulla and pons of the brain control this process.
Respiratory Muscles
- The diaphragm, a dome-shaped muscle, contracts and flattens to increase lung size during inhalation.
- Intercostal muscles found between the ribs also aid in breathing.
- External intercostal muscles pull ribs upward and outward, expanding the chest cavity.
- Internal intercostal muscles pull ribs downward and inward during forced exhalation.
Pressures During Ventilation
- Atmospheric pressure: The pressure of the air surrounding us.
- Intrapleural pressure: The pressure within the space between the parietal and visceral pleura, always slightly lower than atmospheric pressure, creating negative pressure.
- Intrapulmonic pressure: The pressure within the bronchi and alveoli, fluctuating above and below atmospheric pressure during breathing.
Inhalation
- Motor impulses from the medulla stimulate the diaphragm and external intercostal muscles to contract.
- This contraction expands the chest cavity, leading to a decrease in intrapulmonic pressure.
- The negative intrapleural pressure causes the lungs to expand, allowing air to enter the lungs until intrapulmonic pressure equals atmospheric pressure.
Exhalation
- The diaphragm and external intercostal muscles relax, decreasing the chest cavity size.
- This increases intrapulmonic pressure, forcing air out of the lungs.
- Exhalation is typically a passive process relying on lung elasticity.
- Forced exhalation is achieved by contracting the internal intercostal muscles.
Pulmonary Volumes
- Tidal volume: The amount of air involved in normal breathing, approximately 500 ml.
- Minute respiratory volume: The total volume of air inhaled and exhaled in one minute, calculated by multiplying tidal volume by the number of breaths per minute.
- Inspiratory reserve: The additional air that can be inhaled beyond tidal volume during a deep breath, ranging from 2,000-3,000 ml.
- Expiratory reserve: The additional air that can be exhaled beyond tidal volume during a forceful exhalation, ranging from 1,000-1,500 ml.
- Vital capacity: The total volume of air that can be inhaled and exhaled during a deep breath, ranging from 3,500-5,000 ml.
- Residual air: The amount of air remaining in the lungs after forceful exhalation, ranging from 1,000-1,500 ml.
Respiration
- External respiration: Exchange of gases between the alveoli and the blood in the pulmonary capillaries.
- Oxygen diffuses from the alveoli into the blood.
- Carbon dioxide diffuses from the blood into the alveoli.
- Internal respiration: Exchange of gases between the blood in systemic capillaries and the body's tissues.
- Oxygen diffuses from the blood into the tissues.
- Carbon dioxide diffuses from the tissues into the blood.
Nervous Regulation of Respiration
- Inspiration center: Automatically generates impulses to stimulate the contraction of respiratory muscles, leading to inhalation.
- Baroreceptors: Detect lung stretching and send signals to the medulla, inhibiting the inspiration center.
- Expiration center: Activated during forced exhalation, sends impulses to internal intercostal and abdominal muscles.
Respiratory Centers in the Pons
- Apneustic center: Prolongs inhalation.
- Pneumotaxic center: Contributes to exhalation.
Hypothalamus and Cerebral Cortex
- Hypothalamus: Modifies breathing rate during emotional stress.
- Cerebral cortex: Enables voluntary control of breathing rate and rhythm.
Coughing and Sneezing
- Both are controlled by the medulla.
- Coughing: Stimulated by irritation in the pharynx, larynx, or trachea.
- Sneezing: Stimulated by irritation of the nasal mucosa.
Chemical Regulation of Respiration
- Chemoreceptors: Located in the carotid and aortic bodies and medulla, detect changes in blood gases and pH.
- Hypoxia: Low oxygen levels in the blood, detected by chemoreceptors, leading to an increase in respiratory rate.
- Excess carbon dioxide (CO2): Lowers blood pH, detected by chemoreceptors, leading to an increase in respiratory rate to exhale CO2.
- Carbon dioxide is the primary regulator of respiration.
Acid-Base Balance
- Respiratory acidosis: Decreased respiration rate or efficiency leads to CO2 accumulation in body fluids, lowering pH.
- Respiratory alkalosis: Increased respiration rate leads to rapid CO2 expulsion, increasing pH.
- Respiratory compensation: The respiratory center attempts to adjust pH imbalances caused by factors outside the respiratory system.
- Metabolic acidosis: Increased hydrogen ions (acid) in the blood due to factors other than the respiratory system, causing a drop in pH.
- Respiratory compensation: Increased respiratory rate and depth to remove acidic CO2 and raise pH.
- Metabolic alkalosis: Decreased hydrogen ions (acid) in the blood due to factors other than the respiratory system, causing an increase in pH.
- Respiratory compensation: Decreased respiratory rate to retain acidic CO2 and lower pH.
pH Scale
- Ranges from 0 (most acidic) to 14 (most alkaline), with 7 being neutral.
- Normal human body pH falls between 7.35 and 7.45.
Respiratory Compensation
- Respiratory compensation is only about 75% effective.
Aging & The Respiratory System
- Respiratory muscles weaken.
- Lung tissue and alveoli lose elasticity.
- Alveoli walls deteriorate, reducing lung capacity.
- Cilia deteriorate, increasing risk of pneumonia.
- Macrophages become less efficient.
- Chronic lung diseases (emphysema, bronchitis) are more common in the elderly.
- Pulmonary hypertension, an overworked right ventricle, can result from aging.
- Hypertension can lead to an overworked left ventricle and heart failure.
- Pulmonary edema (fluid buildup in the lungs) can also occur with aging.
Ventilation
- Movement of air into & out of the lungs
- Controlled by the nervous system & respiratory muscles
- Respiratory centers in the medulla & pons of the brain control the process
- The medulla generates impulses to the respiratory muscles
Respiratory Muscles
- The diaphragm is a dome-shaped muscle located below the lungs
- The diaphragm contracts & flattens during inhalation, increasing lung size
- Intercostal muscles are located between the ribs
- External intercostal muscles pull ribs upward & outward, expanding the chest cavity
- Internal intercostal muscles pulls ribs downward & inward during forceful exhalation
Pressures During Ventilation
- Atmospheric pressure: Air pressure surrounding our bodies
- Intrapleural pressure: Pressure within the space between parietal & visceral pleura
- Always slightly below atmospheric pressure, referred to as negative pressure
- Intrapulmonary pressure: Pressure within the bronchi & alveoli
- Intrapulmonary pressure fluctuates above & below atmospheric pressure during breathing
Inhalation
- Motor impulses from the medulla travel to the diaphragm & external intercostal muscles
- Diaphragm contracts & flattens, expanding the chest cavity from top to bottom
- External intercostal muscles contract, pulling ribs upward & outward, expanding the chest cavity from side to side & front to back
- Parietal pleura expands due to its attachment to the chest wall
- Intrapleural pressure becomes more negative, creating suction between parietal & visceral pleura
- Visceral pleura expands due to its attachment to parietal pleura & serous fluid
- Lung expansion leads to a decrease in intrapulmonary pressure, pulling air into the lungs
- Air continues to enter the lungs until intrapulmonary pressure equals atmospheric pressure
Exhalation
- Diaphragm & external intercostal muscles relax, decreasing the size of the chest cavity
- Intrapulmonic pressure increases above atmospheric pressure, forcing air out of the lungs
- Exhalation is normally a passive process relying on the elasticity of the lungs
- Forced exhalation is achieved by contracting the internal intercostal muscles, pushing ribs down & in
Pulmonary Volumes
- Tidal volume: Amount of air involved in one normal inhalation & exhalation (about 500 ml)
- Minute respiratory volume: Amount of air inhaled & exhaled in one minute (calculated by multiplying tidal volume by respirations per minute)
- Inspiratory reserve: Amount of air beyond tidal volume that can be taken in with the deepest possible inhalation (2,000 to 3,000 ml)
- Expiratory reserve: Amount of air beyond tidal volume that can be expelled with the most forceful exhalation (1,000 to 1,500 ml)
- Vital capacity: Amount of air involved in the deepest inhalation followed by the most forceful exhalation (3,500 to 5,000 ml)
- Residual air: Amount of air remaining in the lungs after the most forceful exhalation (1,000 to 1,500ml)
Respiration
- External respiration: Exchange of gases between the air in the alveoli & blood in the pulmonary capillaries
- Oxygen diffuses from alveoli to blood
- Carbon dioxide diffuses from blood to alveoli
- Internal respiration: Exchange of gases between the blood in systemic capillaries & the tissues of the body
- Oxygen diffuses from blood to tissues
- Carbon dioxide diffuses from tissues to blood
Nervous Regulation
- Inspiration center: Automatically generates impulses to stimulate contraction of respiratory muscles, leading to inhalation
- Baroreceptors: Detect lung stretching & send sensory impulses to the medulla, inhibiting the inspiration center
- Expiration center: Activated by the inspiration center during forceful exhalation, sends impulses to internal intercostal & abdominal muscles
Respiratory Centers in the Pons
- Apneustic center: Prolongs inhalation
- Pneumotaxic center: Contributes to exhalation
Hypothalamus & Cerebral Cortex
- Hypothalamus: Modifies breathing rate during emotional stress, such as anger or fright
- Cerebral cortex: Enables voluntary control of breathing rate and rhythm
Coughing & Sneezing
- Coughing: Stimulated by irritation of the mucosa in the pharynx, larynx, or trachea
- Sneezing: Stimulated by irritation in the nasal mucosa
- Both actions are controlled by the medulla
Chemical Regulation
- Chemoreceptors: Located in the carotid & aortic bodies & medulla, detect changes in blood gases & pH
- Hypoxia: Low oxygen level in blood, detected by chemoreceptors, leading to an increase in respiratory rate
- Excess carbon dioxide (CO2): Lowers blood pH, detected by chemoreceptors, leading to an increase in respiratory rate to exhale CO2
- Carbon dioxide is the major regulator of respiration
Acid-Base Balance
- Respiratory acidosis: Decreased rate or efficiency of respiration, leading to carbon dioxide accumulation in body fluids
- Respiratory alkalosis: Increased rate of respiration, leading to rapid carbon dioxide expulsion from the body
- Respiratory compensation: Respiratory center attempts to fix a pH imbalance caused by factors other than the respiratory system
- Metabolic acidosis: Caused by factors other than the respiratory system, leading to an increase in hydrogen ions (acid)
- Respiratory compensation: Increase in respiratory rate and depth to remove CO2 (acid) and raise pH
- Metabolic alkalosis: Caused by factors other than the respiratory system, leading to a decrease in hydrogen ions (acid)
- Respiratory compensation: Decrease in respiratory rate to retain CO2 (acid) and lower pH
pH Scale
- 0 is the most acidic, 14 is the most alkaline, and 7 is neutral
- The normal pH for the human body is 7.35 to 7.45
- There is a small range for normal pH in the body
Respiratory Compensation
- Respiratory compensation is only about 75% effective
Aging & the Respiratory System
- Respiratory muscles weaken with age
- Lung tissue & alveoli lose elasticity
- The walls of the alveoli deteriorate, leading to a smaller remaining capacity
- Cilia deteriorate with age
- Macrophages become less efficient, increasing the risk of pneumonia
- Chronic diseases such as emphysema & bronchitis are more common in the elderly
- Pulmonary hypertension can result from aging, leading to an overworked right ventricle
- Hypertension can lead to an overworked left ventricle & heart failure
- Pulmonary edema can also occur with aging
### Ventilation
- The movement of air into and out of the alveoli is controlled by the nervous system and respiratory muscles.
- The respiratory centers in the medulla and pons of the brain control this process.
- The medulla generates impulses to stimulate the respiratory muscles.
Respiratory Muscles
- The diaphragm is a dome-shaped muscle located beneath the lungs.
- Contraction of the diaphragm flattens the muscle, increasing the size of the lungs.
- The intercostal muscles, located between the ribs, also play a crucial role in ventilation.
- The external intercostal muscles pull the ribs upward and outward, further increasing lung volume.
- The internal intercostal muscles pull the ribs downward and inward, decreasing lung volume.
Pressures During Ventilation
- Atmospheric pressure is the pressure exerted by the air surrounding us.
- Intrapleural pressure is the pressure within the potential space between the parietal and visceral pleura.
- It is always slightly lower than atmospheric pressure, creating a negative pressure that helps maintain lung expansion.
- Intrapulmonic pressure is the pressure within the bronchial tree and alveoli.
- It fluctuates above and below atmospheric pressure during breathing.
Inhalation
- Motor impulses from the medulla travel to the diaphragm and external intercostal muscles, initiating inhalation.
- The diaphragm contracts, flattening and moving downward, expanding the chest cavity from top to bottom.
- External intercostal muscles contract, pulling ribs upward and outward, expanding the chest cavity from side to side and front to back.
- This expansion of the chest wall stretches the parietal pleura, which in turn stretches the visceral pleura due to the serous fluid creating a suction between them.
- The lung expands, decreasing intrapulmonic pressure and drawing air into the lungs.
- Air continues to enter the lungs until intrapulmonic pressure equals atmospheric pressure.
Exhalation
- Relaxation of the diaphragm and external intercostal muscles decreases the size of the chest cavity.
- This decrease in chest cavity volume increases intrapulmonic pressure above atmospheric pressure.
- The pressure difference forces air out of the lungs.
- Exhalation is typically a passive process, relying on the elasticity of the lungs.
- Forced exhalation can be achieved by contracting the internal intercostal muscles, pushing the ribs down and inward.
Pulmonary Volumes
- Tidal volume is the amount of air involved in one normal inhalation and exhalation, typically around 500 ml.
- Minute respiratory volume is the total amount of air inhaled and exhaled in one minute.
- It is calculated by multiplying tidal volume by the number of breaths per minute.
- Inspiratory reserve volume is the additional amount of air that can be inhaled beyond tidal volume with the deepest possible inhalation, typically 2,000-3,000 ml.
- Expiratory reserve volume is the amount of air that can be exhaled beyond tidal volume with the most forceful exhalation, typically 1,000-1,500 ml.
- Vital capacity is the total amount of air involved in the deepest inhalation followed by the most forceful exhalation, typically 3,500-5,000 ml.
- Residual volume is the amount of air that remains in the lungs after the most forceful exhalation, typically 1,000-1,500 ml.
Respiration
- External respiration is the exchange of gases between the air in the alveoli and the blood in the pulmonary capillaries.
- Oxygen diffuses from the alveoli to the blood, while carbon dioxide diffuses from the blood to the alveoli.
- Internal respiration is the exchange of gases between the blood in systemic capillaries and the tissues of the body.
- Oxygen diffuses from the blood to the tissues, while carbon dioxide diffuses from the tissues to the blood.
Nervous Regulation
- The inspiration center automatically generates impulses to stimulate contraction of respiratory muscles, leading to inhalation.
- Baroreceptors in the lungs detect stretching, sending sensory impulses to the medulla that inhibit the inspiration center, contributing to exhalation.
- The expiration center is activated by the inspiration center during forceful exhalation, sending impulses to the internal intercostal and abdominal muscles.
Respiratory Centers in the Pons
- The apneustic center prolongs inhalation.
- The pneumotaxic center contributes to exhalation.
Hypothalamus and Cerebral Cortex
- The hypothalamus modifies breathing rate during emotional stress, such as anger or fright.
- The cerebral cortex enables voluntary control of breathing rate and rhythm.
Coughing and Sneezing
- Both coughing and sneezing are controlled by the medulla.
- Coughing is stimulated by irritation of the mucosa in the pharynx, larynx, or trachea.
- Sneezing is stimulated by irritation of the nasal mucosa.
Chemical Regulation
- Chemoreceptors located in the carotid and aortic bodies and medulla detect changes in blood gases and pH.
- Hypoxia, or low oxygen level in the blood, stimulates chemoreceptors, leading to an increase in respiratory rate.
- Excess carbon dioxide (CO2) lowers blood pH, also stimulating chemoreceptors and leading to an increase in respiratory rate to exhale CO2.
Acid-Base Balance
- Respiratory acidosis is a condition where the rate or efficiency of respiration is decreased, leading to carbon dioxide accumulation in body fluids.
- Respiratory alkalosis is a condition where the rate of respiration is increased, leading to rapid carbon dioxide expulsion from the body.
- The respiratory center attempts to compensate for pH imbalances caused by factors other than the respiratory system.
- Metabolic acidosis, a condition where factors other than the respiratory system cause an increase in hydrogen ions (acid), can be compensated for by increasing respiratory rate and depth to remove CO2 and raise pH.
- Metabolic alkalosis, a condition where factors other than the respiratory system cause a decrease in hydrogen ions (acid), can be compensated for by decreasing respiratory rate to retain CO2 and lower pH.
pH Scale
- The pH scale ranges from 0 to 14, with 7 being neutral.
- 0 is the most acidic, and 14 is the most alkaline.
- The normal pH for the human body is between 7.35 and 7.45.
- The body maintains a narrow range for normal pH.
Respiratory Compensation
- Respiratory compensation is only about 75% effective in correcting pH imbalances.
Aging and Respiratory System
- Respiratory muscles weaken with age.
- Lung tissue and alveoli lose elasticity, decreasing the efficiency of gas exchange.
- The walls of the alveoli deteriorate, leading to smaller remaining capacity.
- Cilia, responsible for clearing the respiratory tract, deteriorate with age, increasing the risk of infection.
- Macrophages, important for fighting off infection, become less efficient.
- Chronic diseases such as emphysema and bronchitis become more common in the elderly.
- Pulmonary hypertension, a condition where the pressure in the pulmonary arteries increases, is more common in older adults, leading to an overworked right ventricle.
- Hypertension can lead to an overworked left ventricle and even heart failure.
- Pulmonary edema, fluid buildup in the lungs, also becomes more common with aging.
Studying That Suits You
Use AI to generate personalized quizzes and flashcards to suit your learning preferences.